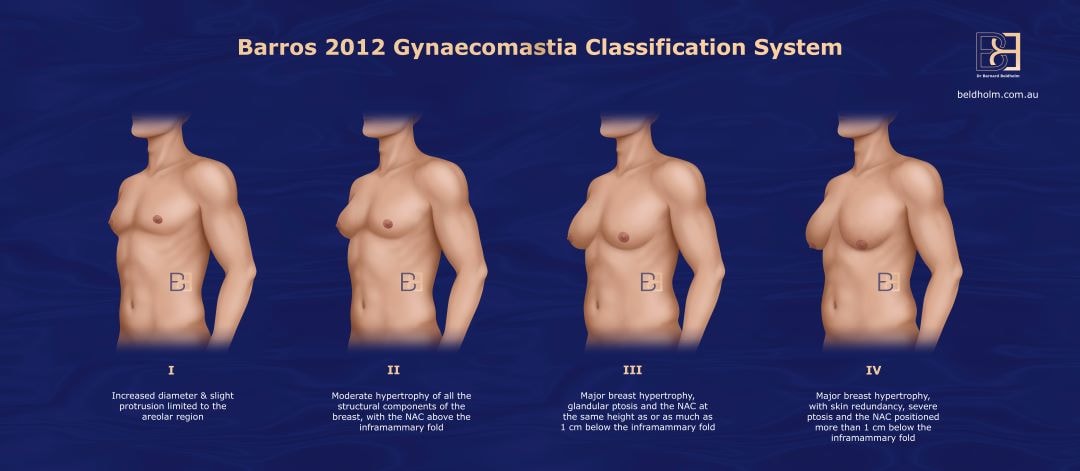
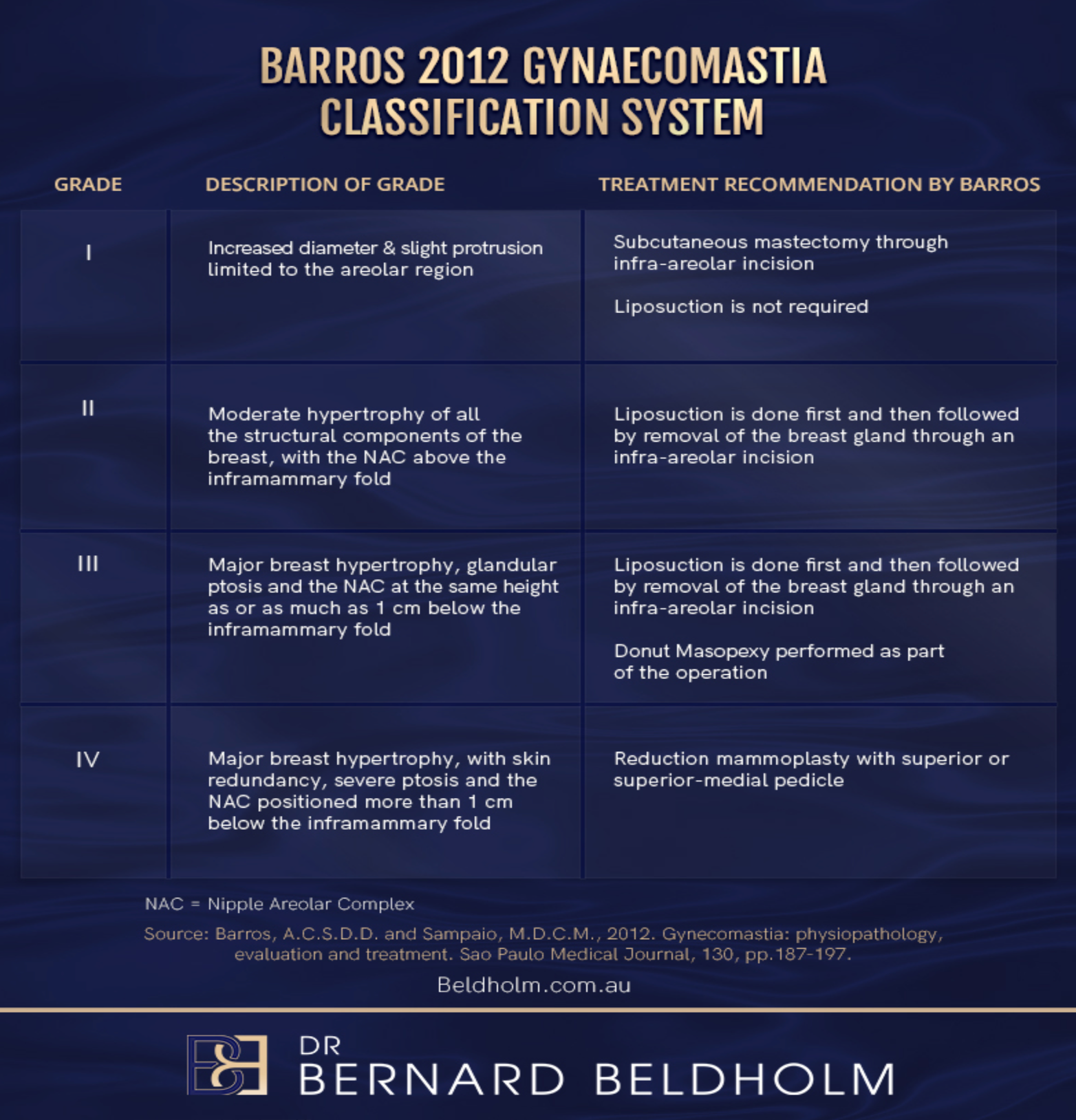
Presented by Alfredo Carlos Simões Dornellas de Barros to classify gynaecomastia based on the shape, size, and degree of male breast enlargement, as well as skin laxity, the Barros 2012 Gynaecomastia System outlines the causes, varying levels of severity, and surgical planning for each grade.
This text discusses one of the many classification systems for gynecomastia. It is based on the original scientific work of Barros to provide a more accurate overview of this grading system. However, Dr. Beldholm does not use this particular grading system in his practice; he has developed his own system, which he believes offers better grading and more effective treatment recommendations. For a comprehensive overview of the various grading systems available, you can refer to the article: Dr. Bernard Beldholm’s Comprehensive Summary of Gynecomastia Surgery Grading Systems.
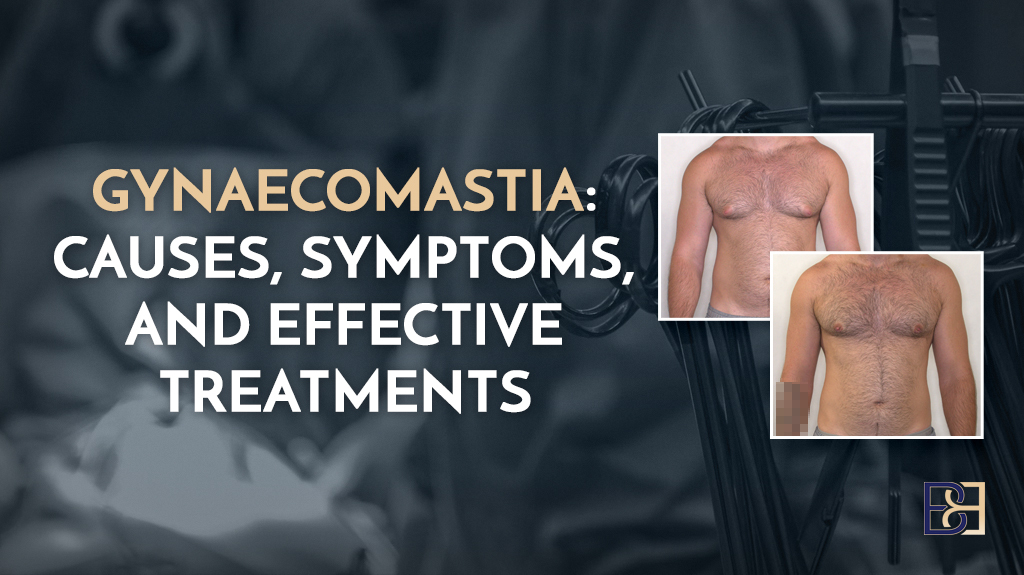
In the article, Gynecomastia: Physiopathology, Evaluation and Treatment, Barros explains, defines, and offers treatment suggestions highlighted in the Barros (2012) classification system. Closely based on the Cordova and Moschella classification system, Barros explains that gynecomastia (GM) is a benign condition characterised by enlargement of the male breast, often “attributable to proliferation of the glandular tissue and local fat deposition.” (Ref 1)
Commonly affected by hormonal imbalances, obesity, genetics, medications, or certain health conditions, Barros’ treatment recommendations range from lifestyle changes, “reassurance,” or pharmacotherapy for prepubescent patients or those with milder conditions to surgical intervention for more severe cases.
Book your appointment online now
Barros’ Key Findings
The author outlines a list of well-documented and historically accepted causes for the condition, from medication, recreational drug use, and hormonal imbalances to obesity, age, and health conditions. Barros also focuses on the psychological aspects of the condition, recognizing that the physical discomfort and psychological distress of gynaecomastia may have a negative impact on one’s body image.
On the other hand, however, the author expresses that psychological symptoms alone may not warrant surgical intervention, stating that “(i)f the GM is slight, without noteworthy psychological repercussions and the appropriate work-up does not reveal any underlying disease… (r)eassurance is widely regarded as (the most reasonable) form of treatment.”
“For mild enlargements in pubertal boys,” the author continues, “the therapeutic approach is verbal explanation and reassurance regarding the signs and symptoms. Reassurance should be based on full and authoritative explanations about the common transient hormonal imbalance at this age, the natural involution of the condition and the absence of later sexual and fertility effects.”
For this reason and, equally as important, for other developmental and psychological reasons, a weight loss program (diet and physical exercises) should be the first-line treatment.”
Barros does go on to explain that “if GM either persists or becomes more severe and is associated with pain, psychological distress or embarrassment caused by avoidance of activities in which the chest is exposed, pharmacological and surgical therapeutic options should be considered, especially when the patient wishes to pursue treatment.”
When referencing surgical treatment, Barros expresses that “in most cases…the best results are achieved by combining liposuction and mammary adenectomy,” with “the presence of cutaneous ptosis and the amount of excessive skin (being) decisive in guiding the choice between surgical treatment methods.”
When discussing pseudogynecomastia, a condition where the male chest appears enlarged due to excess fat deposits rather than the development of glandular breast tissue, the article recommends weight loss as the primary option for pseudogynecomastia, though the impact of pseudogynecomastia can be as severe as real gynecomastia.
Causes of Gynaecomastia
The author identifies the following causes of GM in order of prevalence:
- Idiopathic (no underlying detected abnormality): 50%
- Drug-induced (including cocaine, heroin, amphetamines, marijuana, androgens, anabolic steroids, and some antidepressants.): 20 to 25%
- Cirrhosis: 8%
- Primary hypogonadism: 8%
- Testicular tumours: 3%
- Secondary hypogonadism: 2%;
- Hyperthyroidism: 1.5%
- Renal disease: 1%
Evaluation
In the Barros model, clinical evaluations on men with enlarged breast tissue have three phases:
- Making the diagnosis of true GM
- Trying to find an aetiological factor to further guide case management
- Classifying into severity grades.

Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
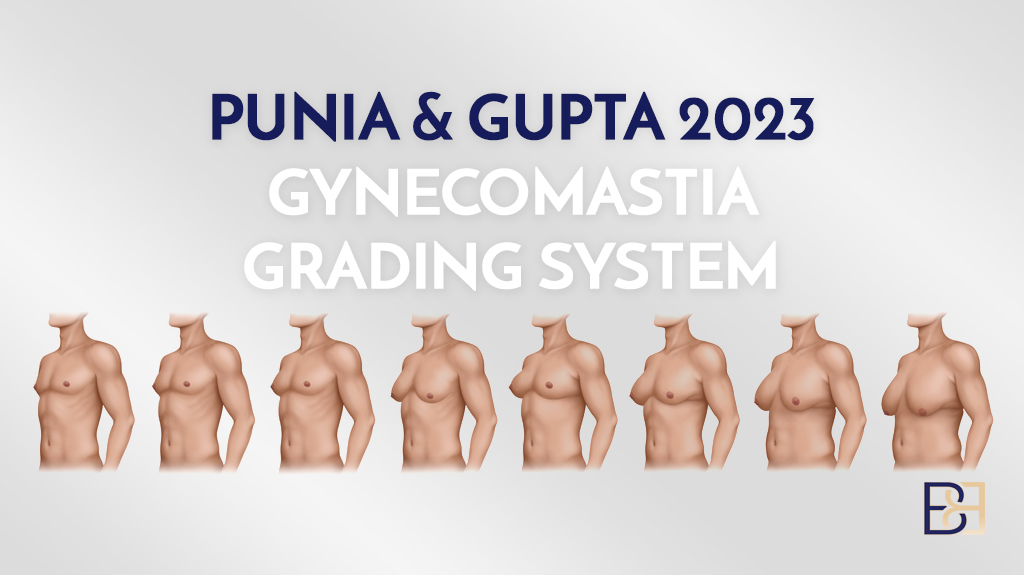
Classifying into Grades
Barros explains that gynaecomastia shows a gradation of clinical types that range from areolar protrusion to breasts with a female appearance, with the main clinical features being breast swelling, increased areolar diameter, presence of an anomalous inframammary fold, glandular ptosis, and skin redundancy.
The authors of the Barros study adopted the clinical classification of Cordova and Moschella with some modifications and notes that this classification takes into account the different relationships between the structural components of the breast, in particular the inframammary fold and nipple-areola complex (NAC), which separates mild forms from more serious cases.
Barros Grade I
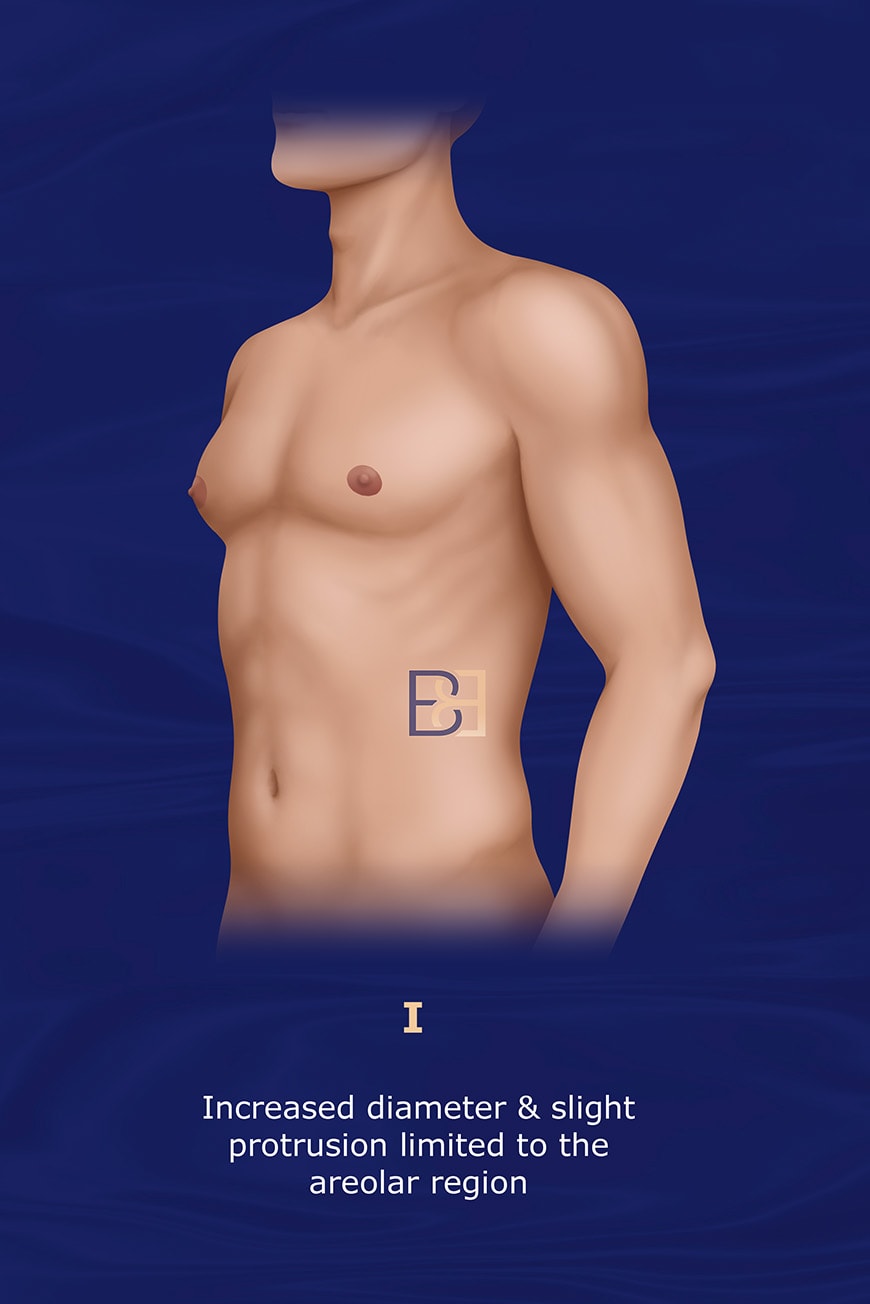
Presentation:
- Increased diameter and slight protrusion limited to the areolar region
- Small breast enlargement with well-defined contours.
- No skin excess or significant breast ** (ptosis)
- Enlargement caused solely by glandular proliferation
- Absence of adipose accumulation
Treatment recommended by Barros:
- Surgical correction involves mammary adenoidectomy performed by a semicircular inferior periareolar incision.
- Liposuction is not required
Barros Grade II
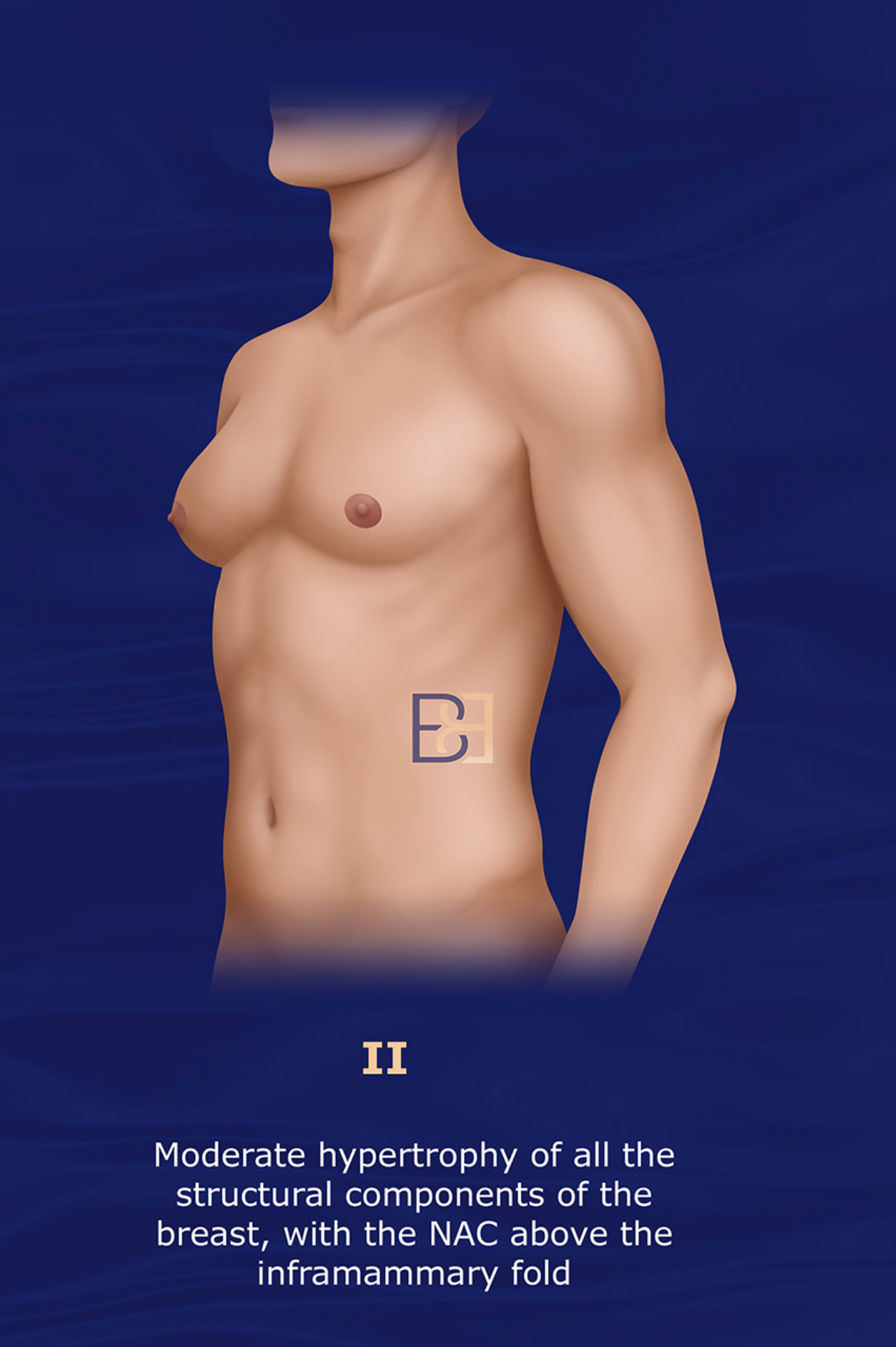
Presentation:
- Moderate hypertrophy of all the structural components of the breast, with the NAC above the inframammary fold
- Excessive glandular tissue
- Local adiposity
Treatment recommended by Barros:
- Liposuction and surgical excision should be combined in the same operation, with the procedure beginning with vacuum lipoplasty, followed by mammary adenectomy by means of a classical periareolar incision.
- Dissection flaps must be thin (0.5 cm) to avoid recurrence.
- Mammary adenectomy without liposuction leads to unsatisfactory outcomes, with an uneven surface or asymmetry
Grade III
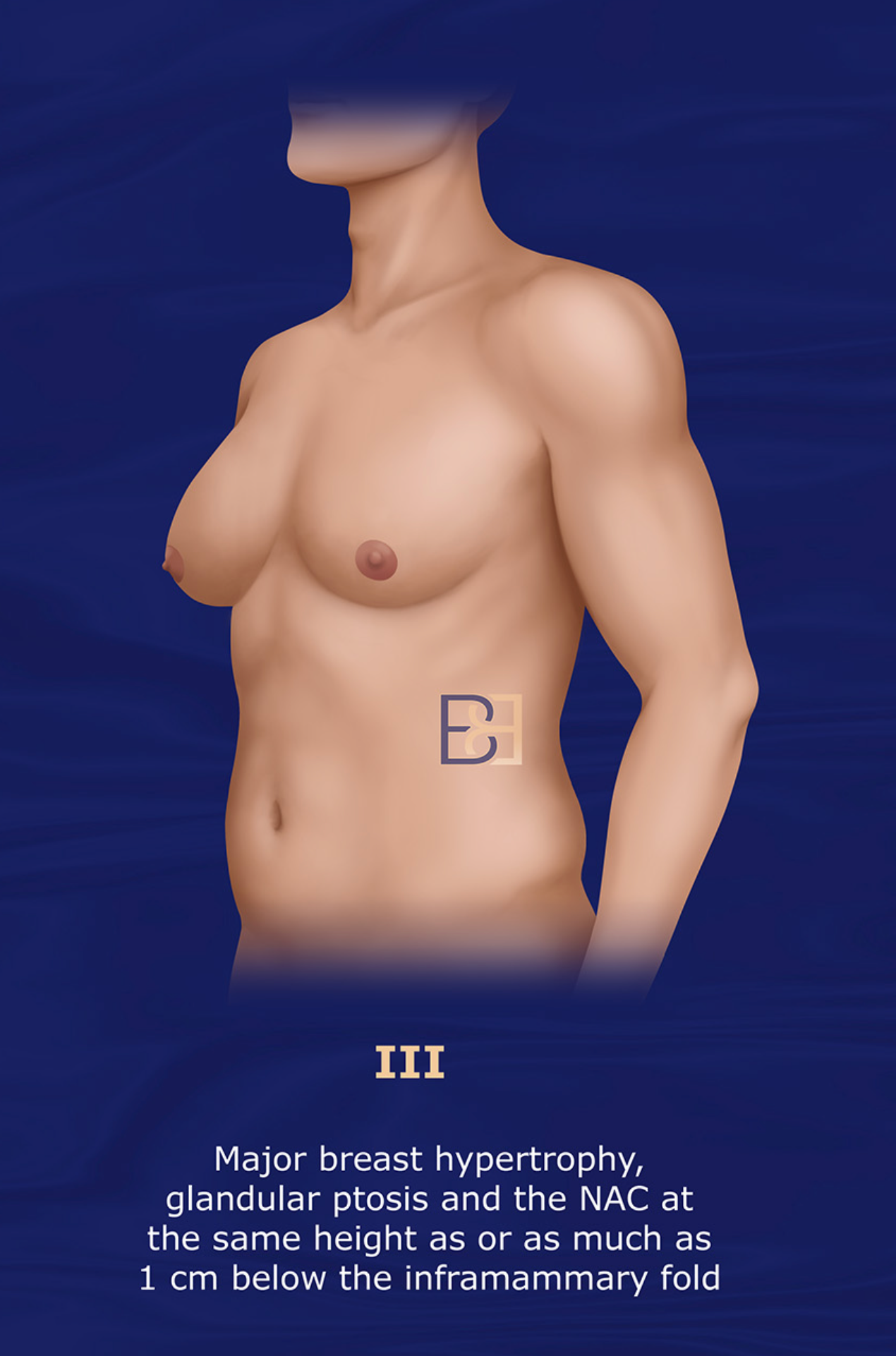
Presentation:
- Moderate hypertrophy of the structural components of the breast
- NAC at the same height as or more than 1 cm below the inframammary fold
- Early signs of breast ptosis.
- This grade involves both glandular and fatty tissue.
Treatment recommended by Barros:
- The treatment begins with liposuction, followed by glandular excision with periareolar removal of the tissue.
- A double-circle incision performed over the skin makes it possible to remove the epithelial tissue from an annular portion of skin that is as large as needed for each case.
- The author stresses the importance of scars being restricted to the periareolar area.
Barros Grade IV
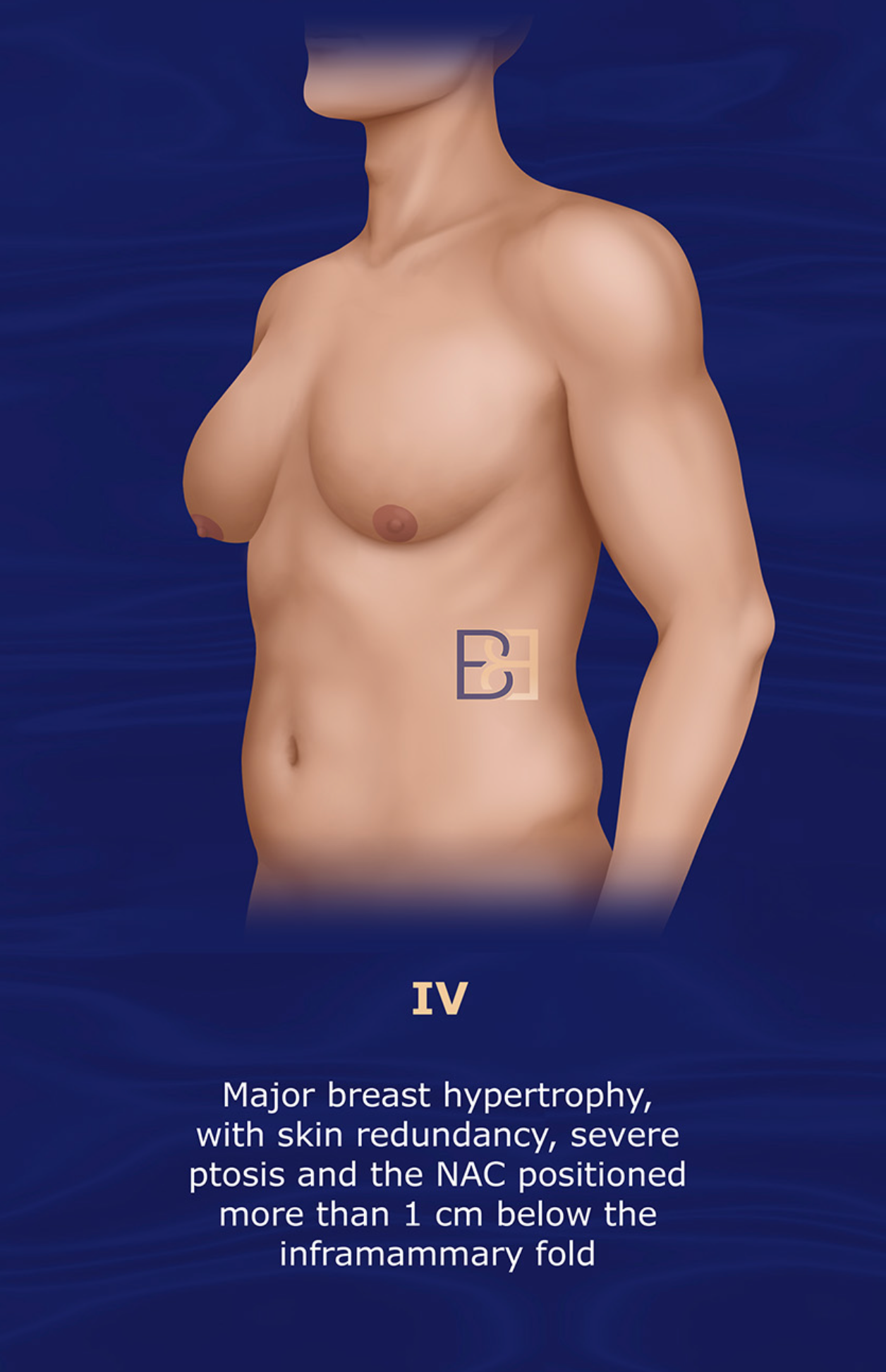
Presentation:
- Major breast hypertrophy, with skin redundancy,
- Severe ptosis and the NAC positioned more than 1 cm below the inframammary fold
Treatment recommended by Barros:
- Removal of gland and skin to flatten the chest outline.
- Inverted T-shaped resection with NAC migration using superior or superior-medial dermic pedicles
Dr Beldholm’s Review of the Barros Classification and Study

After an in-depth dive into the study, Dr. Beldholm offered the following review.
- Notably, Dr Beldholm found that the review does not contain an explanation as to why this classification system was created. Other systems, such as the Ratnam classification system, were created to build upon previous systems.
- Though the proposed classification and treatment protocol were found to help solve problems associated with surgical outcomes for all types of gynaecomastia, the Barros system does not appear to offer an actual reason for this new classification.
- The Barros Classification System does not focus on the lateral chest skin or lateral breast rolls, which must be treated to achieve an optimal outcome.
- In addition to the opinions offered above, Dr Beldholm also found that the article recommends weight loss as the primary option for pseudogynecomastia, when in fact, the impact of pseudogynecomastia can be as severe as real gynecomastia. Dr Beldholm feels that once a patient presents to a surgeon for treatment, the patient should be given the attention they deserve and receive surgical interventions to alleviate this condition.
Dr Beldholm’s Grade-by-Grade Observations
Grade 1: This 4 stage classification system has no mention of puffy nipple and, in my opinion, I feel this condition should have its own stage as the treatment is different from larger gynecomastia.
For patients with puffy nipples or minimal gynecomastia, I would treat the gynecomastia by excision only without liposuction. For more severe cases, I would add VASER liposuction to minimise the risk of saucer deformity.
Grade 2: Though I agree with this treatment, I normally perform VASER liposuction as well as gland excision. It is important to avoid cutting the muscle fascia or make the Areola (NAC) too thin to avoid tethering down of the NAC
Grade 3: in this grade there is going to be loose skin. I don’t think the Benelli lift is a good operation as it tends to leave a poor scar, and it also only provides minimal lift to the areola. U skin lift may give a better position of NAC. However all these lift techniques are very limited.
Grade 4: I agree that these need skin resection. However, mastopexy and breast reduction techniques that are used in women are not appropriate for men. They leave too much tissue and have the tendency to still look like female breasts. In my opinion, Torsoplasty with free grafts is the best option.
Final Thoughts
The Barros Classification system 2012 was created to define, classify, and offer treatments for four grades of gynaecomastia, a common condition the author attributes to an oestrogen/androgen imbalance caused by several etiological factors.
After confirming the diagnosis, searching for a specific cause and classifying the case according to severity grade, the Barros model recommends that therapy should be personalised, with lifestyle guidance, reassurance, medical treatment, and surgical correction as valid therapeutic options.
While the system presents valid treatments and approaches, Dr Beldholm is of the opinion that the Barros model does not focus on certain key aspects of the condition, nor does it offer any groundbreaking recommendations or determinations.
Medical References
- Sao Paulo Med J. 2012; 130(3):187-97
- Georgiadis E, Papandreou L, Evangelopoulou C, et al. Incidence of gynaecomastia in 954 young males and its relationship to somatometric parameters. Ann Hum Biol. 1994;21(6):579-87.
- Nuttall FQ. Gynaecomastia as a physical finding in normal men. Nydick M, Bustos J, Dale JH Jr, Rawson RW. Gynaecomastia in adolescent boys. JAMA. 1961;178:449-54.
- Niewoehner CB, Nuttall FQ. Gynaecomastia in a hospitalised male population. Am J Med. 1984;77(4):633-8.
- Bannayan GA, Hajdu SI. Gynaecomastia: clinicopathologic study of 351 cases. Am J Clin Pathol. 1972;57(4):431-7.
- Moore NP. The oestrogenic potential of the phthalate esters. Reprod Toxicol. 2000;14(3):183-92.
- Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement Endocr Rev. 2009;30(4):293-342.
- Sasano H, Kimura M, Shizawa S, Kimura N, Nagura H. Aromatase and steroid receptors in Gynaecomastia and male breast carcinoma: an immunohistochemical study. J Clin Endocrinol Metabol. 1996;81(8):3063-7.