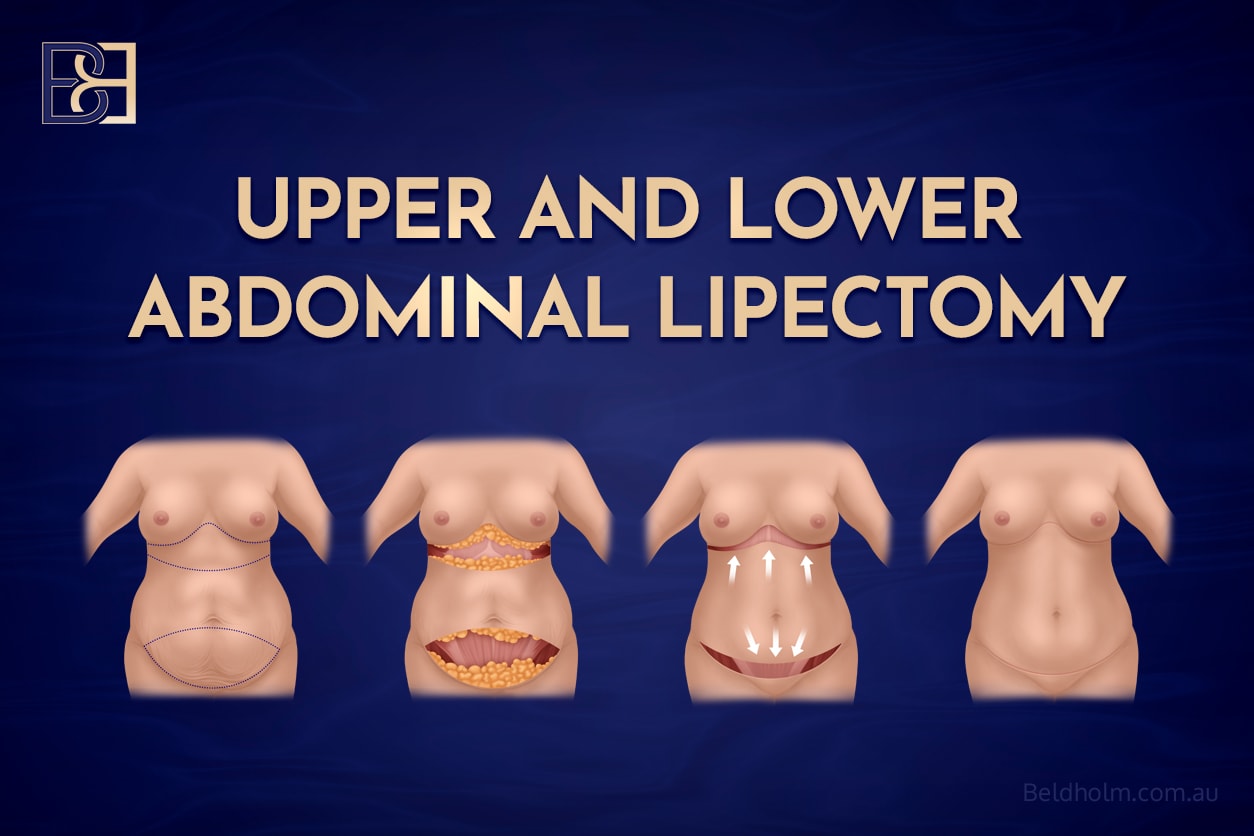
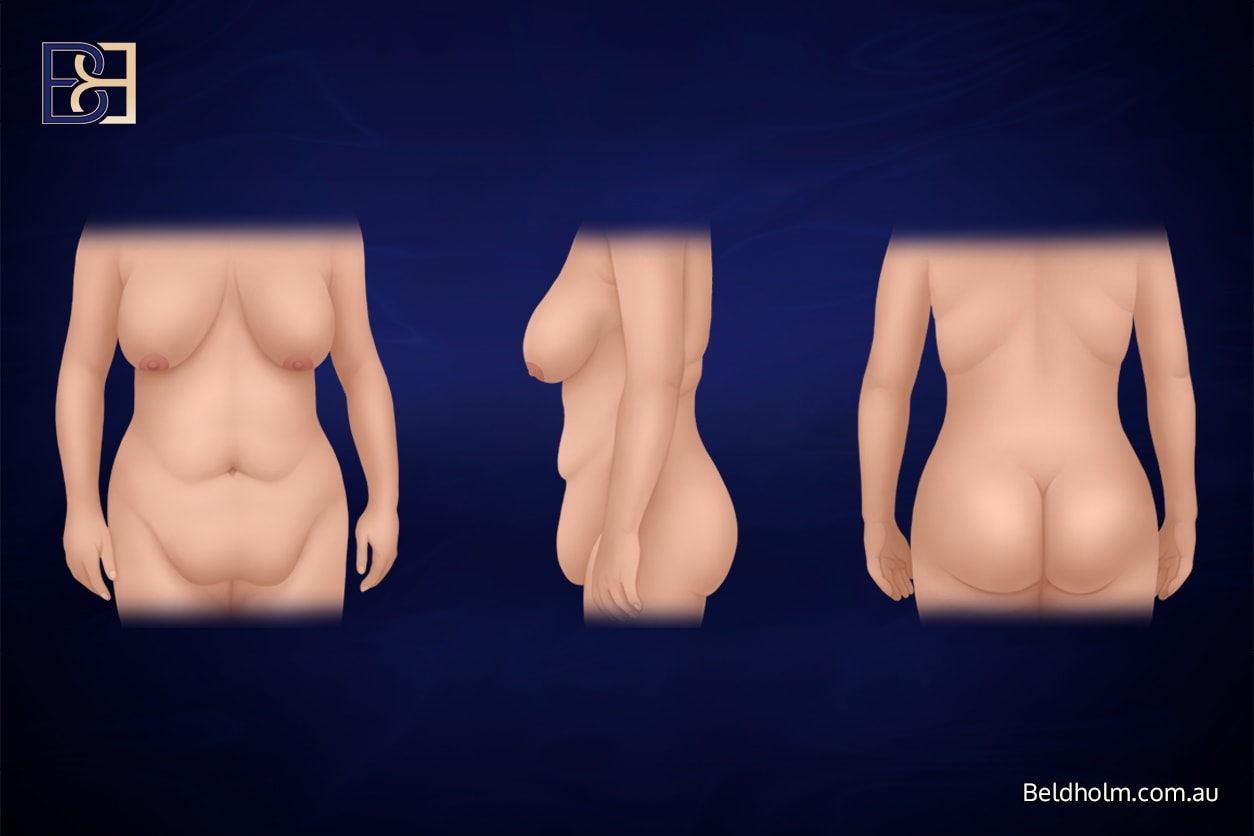
Upper and lower abdominal lipectomy performed together is an uncommon but recognised body contouring surgery option for selected post weight loss patients. It is generally considered for individuals who have experienced massive weight loss or significant weight loss, often following bariatric surgery or sustained lifestyle changes, and who are left with persistent excess skin concentrated in the upper abdomen beneath the chest and the lower abdomen below the umbilicus.
While this surgical procedure can remove excess skin without repositioning the umbilicus and with limited tissue undermining, it remains major surgery. Like all body contouring procedures performed after weight loss, it carries specific risks and potential complications. Understanding these complications is an essential part of informed consent and realistic surgical planning.
Understanding Upper and Lower Abdominal Lipectomy
An upper and lower abdominal lipectomy involves excision of excess skin and fat from two separate abdominal zones. Unlike a standard tummy tuck (abdominoplasty), the umbilicus is usually left in its original position and there is less extensive undermining of the abdominal skin flap.
This approach may be considered in a narrow group of post weight loss patients where loose skin is predominantly located above and below the umbilicus, central abdominal laxity is limited, and the patient has achieved a stable weight.
Despite these technical differences, the overall risk profile overlaps significantly with abdominoplasty surgery, belt lipectomy, and other abdominal contouring operations.
Why Complication Risk Is Higher After Weight Loss
Patients who have experienced major weight loss differ from those undergoing abdominal surgery for other reasons. Several physiological and lifestyle factors can increase the likelihood of postoperative complications.
Skin Quality and Reduced Elasticity
After massive weight loss, skin elasticity is often reduced. Prolonged stretching followed by weight reduction leaves stretched skin and lax skin with compromised blood supply. This increases the risk of poor wound healing, wound separation, and wound dehiscence.
Nutritional Deficiencies

Patients who have undergone weight loss surgery, including laparoscopic gastric banding or gastric bypass, may develop nutritional deficiencies. Low protein levels, iron deficiency, and vitamin deficiencies can negatively affect wound healing and immune response, increasing the risk of wound infections.
Medical Comorbidities
Some post bariatric patients have ongoing medical conditions such as diabetes, anaemia, or cardiovascular disease. These conditions can impair circulation and healing and increase surgical risk.
General Surgical Risks
All major surgical procedures carry baseline risks, regardless of technique.
Bleeding and Haematoma

Bleeding can occur during or after surgery. In some cases, blood collects beneath the skin, forming a haematoma. While many resolve without intervention, some require surgical drainage.
Infection

Wound infections may develop in the early postoperative period. Signs can include redness, warmth, discharge, increasing pain, or fever. Management may involve antibiotics, dressing changes, or further procedures.
Anaesthetic-Related Risks
Book your appointment online now
General anaesthesia carries its own risks, including nausea, cardiovascular instability, and respiratory complications, particularly in patients with higher body mass index or medical comorbidities.
Wound-Related Complications
Wound Separation and Dehiscence

Wound separation is one of the more common complications following abdominal contouring in massive weight loss patients. Long incisions and tension across closure lines increase this risk, particularly in the lower abdomen.
Delayed Wound Healing
Delayed wound healing is common after post weight loss body contouring. Areas with reduced blood supply may take longer to heal, prolonging recovery and the need for ongoing wound care.
Scar-Related Issues
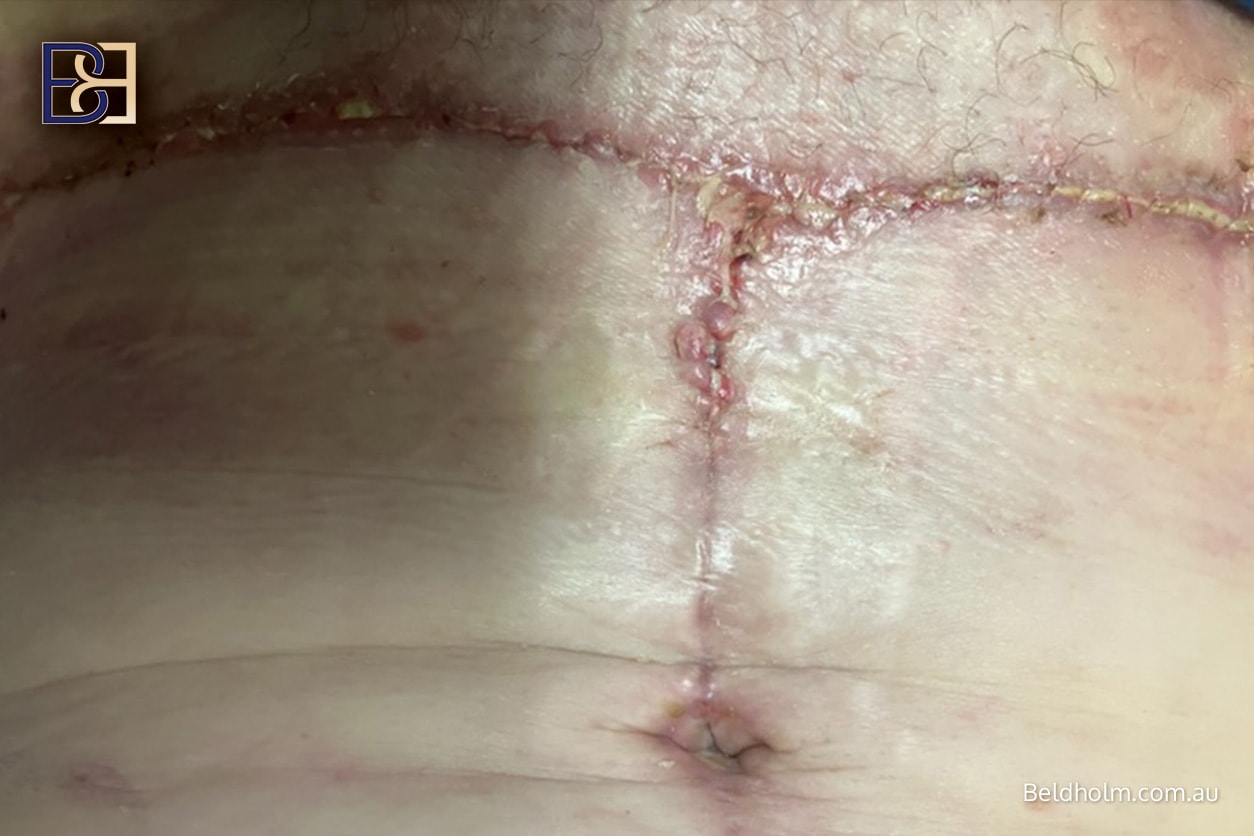
Scar tissue maturation takes many months. Thickened, widened, or uneven scars may develop, especially if wound healing is delayed or complicated by infection.
Fluid-Related Complications
Seroma Formation
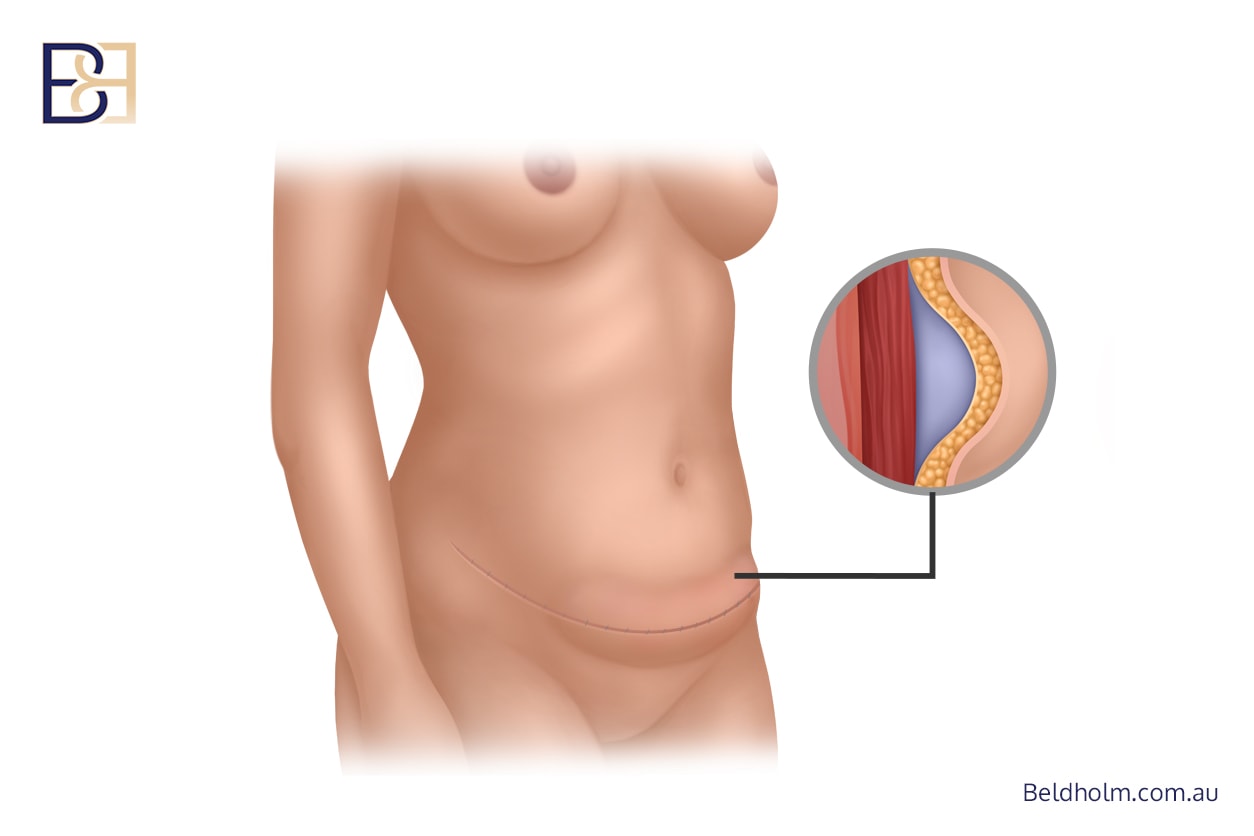
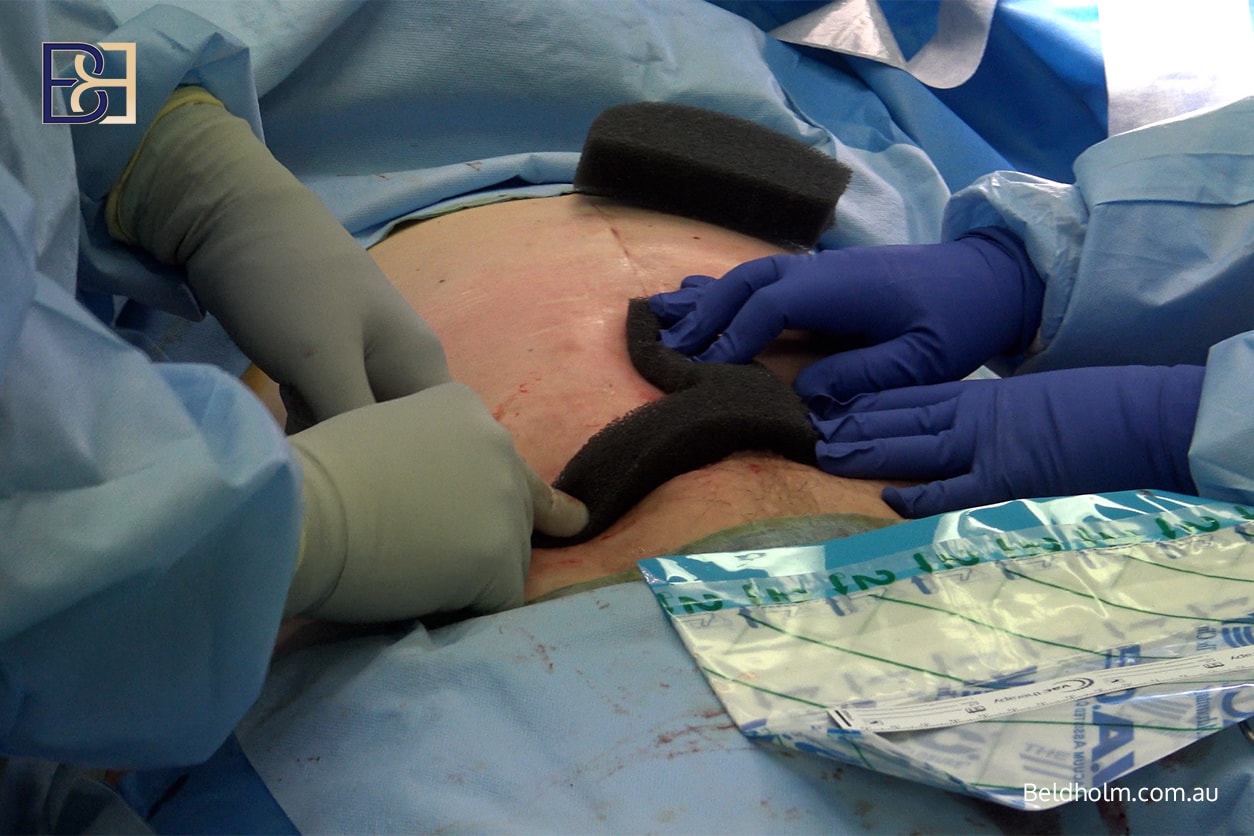
A seroma is a collection of fluid beneath the skin. Although limited undermining reduces risk, seromas can still occur after upper and lower abdominal lipectomy. Management may involve aspiration, prolonged drainage, or compression garment use.
Fat Necrosis
Fat necrosis occurs when small areas of fat lose their blood supply. This may present as firm or tender areas under the skin and can occasionally lead to inflammation or discharge.
Blood Clots and Thromboembolic Complications
Deep Vein Thrombosis
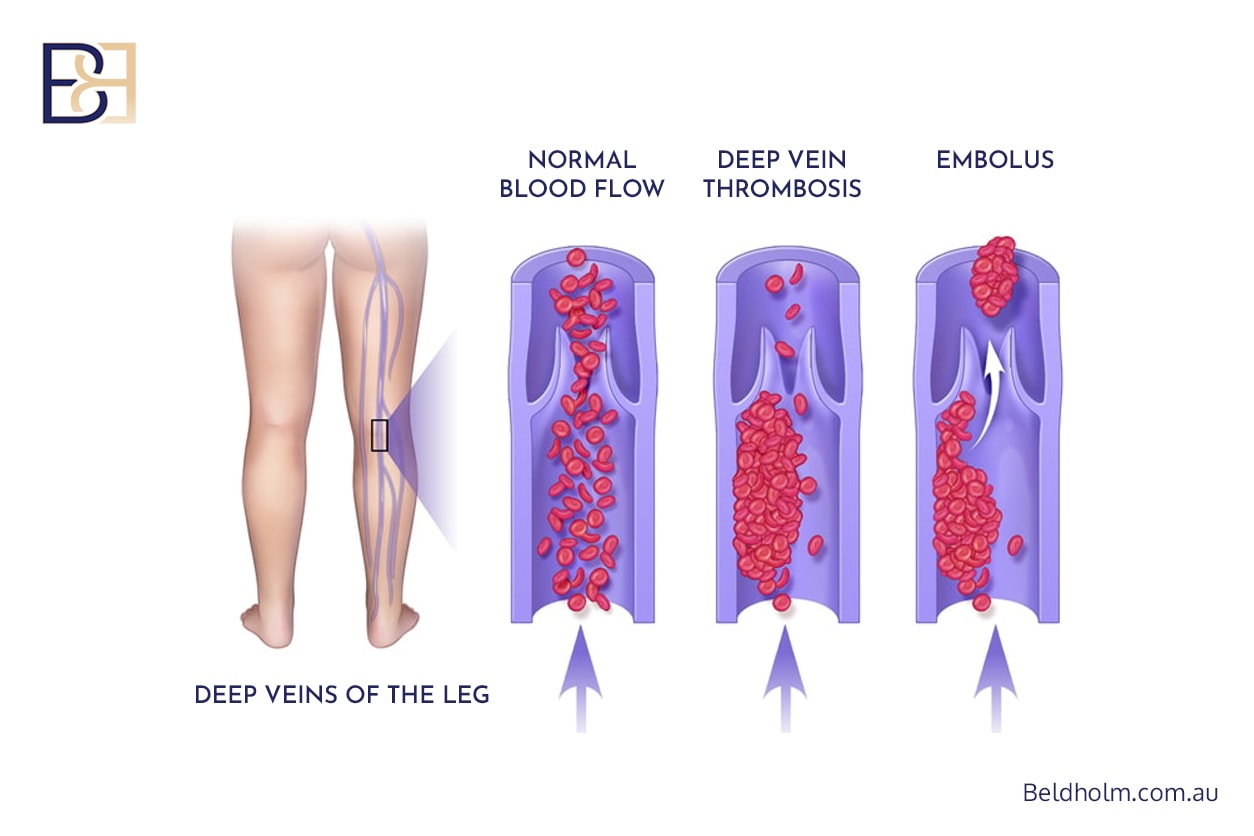
Deep vein thrombosis involves clot formation in the deep veins, usually of the legs. Risk increases with prolonged surgery, reduced mobility, and higher body mass index.
Pulmonary Embolism
A pulmonary embolism occurs when a blood clot travels to the lungs. While uncommon, it is a serious complication requiring urgent treatment. Preventive strategies include early mobilisation, compression devices, and anticoagulation where appropriate.
Sensory Changes and Nerve Effects
Altered Skin Sensation
Temporary or permanent changes in skin sensation are common following abdominal surgery. Numbness or altered sensation often improves over time but may persist in some areas.
Prolonged Discomfort
Some patients experience prolonged tightness or discomfort related to the healing of the underlying muscles and overlying skin, particularly when returning to upright posture.
Weight Changes After Surgery

Significant changes in body weight after surgery can affect results and increase complication risk. Further weight loss may contribute to recurrent loose skin, while weight gain can place additional strain on scars and soft tissues.
Maintaining a stable weight before and after surgery is important for supporting wound healing and long‑term outcomes.
Combined Procedures and Increased Risk
Upper and lower abdominal lipectomy may be performed alone or combined with other body contouring procedures such as belt lipectomy (lower body lift), upper body lift (upper belt lipectomy), or inner thigh lift (thighplasty). Combining procedures increases operative time and may increase the risk of postoperative complications, including blood clots and delayed recovery.
Each additional procedure must be carefully assessed on an individual basis.
Less Common and Long‑Term Complications
Less frequent complications may include chronic swelling, persistent pain, asymmetry, or the need for revision surgery. These outcomes vary widely and depend on individual anatomy, healing capacity, and postoperative care.
Reducing the Risk of Complications

Although complications cannot be eliminated, risk may be reduced through careful patient selection, optimisation of nutrition, smoking cessation, appropriate use of compression garments, early mobilisation, and structured postoperative follow‑up. Open discussion of risk factors and realistic expectations is a critical part of surgical planning.
Frequently Asked Questions
What are three potential complications of weight loss surgery?
Common issues include nutritional deficiencies, wound healing problems, and blood clots.
What is the most common complication of abdominal surgery?
Delayed wound healing and minor wound separation are frequently encountered, particularly in post weight loss patients.
What is the most common complication of abdominoplasty?
Seroma formation is often cited as the most common complication after tummy tuck (abdominoplasty) procedures.
Final Considerations

Upper and lower abdominal lipectomy can be appropriate for selected patients following a weight loss journey, but it remains major body contouring surgery with recognised risks. Understanding potential complications supports informed decision‑making and realistic recovery planning.