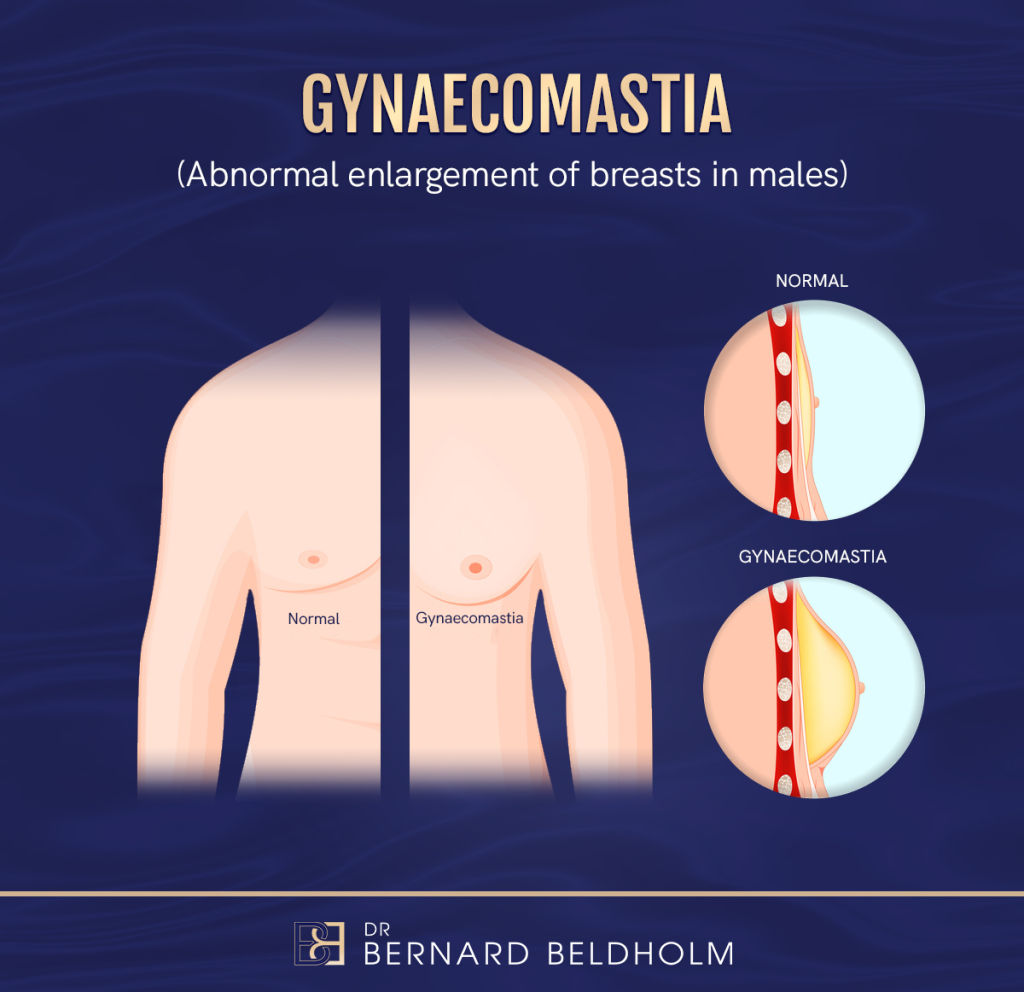
Gynaecomastia is a common aesthetic issue frequently encountered by surgeons. Most male patients with this condition undergo surgery to regain their masculine contour and flat chest with as few scars as possible.
Developed by Adriana Cordova and Francesco Moschella, a study was conducted to review the older classification methods of grading Gynaecomastia treatments and patient presentation. They developed a new classification system that included a scheme for morphological classification of gynaecomastia, which could serve as a guide for choosing the surgical technique.
Book your appointment online now
An analysis was made of 121 gynaecomastia cases over 5 years, examining the extent of the techniques employed, complications, and the need to re-operate.
On the basis of this review, the authors voiced the following opinion:
- When the nipple-areola complex is above the inframammary fold, complete flattening of the thorax can be achieved with suction or ultrasound-assisted lipectomy and skin-sparing adenectomy.
- When the nipple-areola complex is at the same height as, or at most 1 cm below the fold, skin-sparing techniques are no longer sufficient to flatten the thorax, and it becomes necessary to remove the redundant skin by means of periareolar removal of epidermis.
- When significant ptosis is present and the nipple-areola complex is more than 1 cm below the fold, reduction mastoplasty becomes necessary.
In response, the authors developed a new classification system.
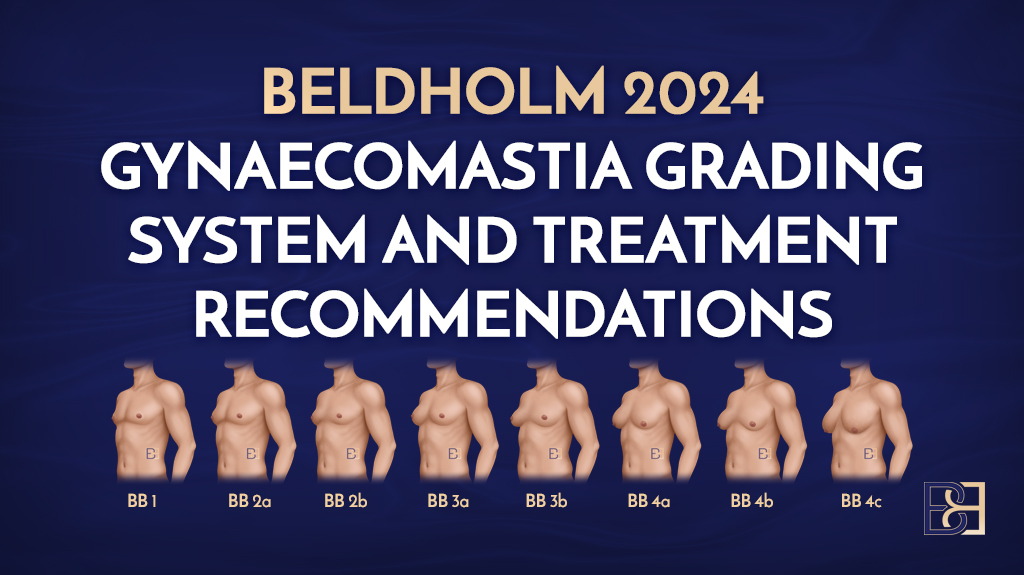
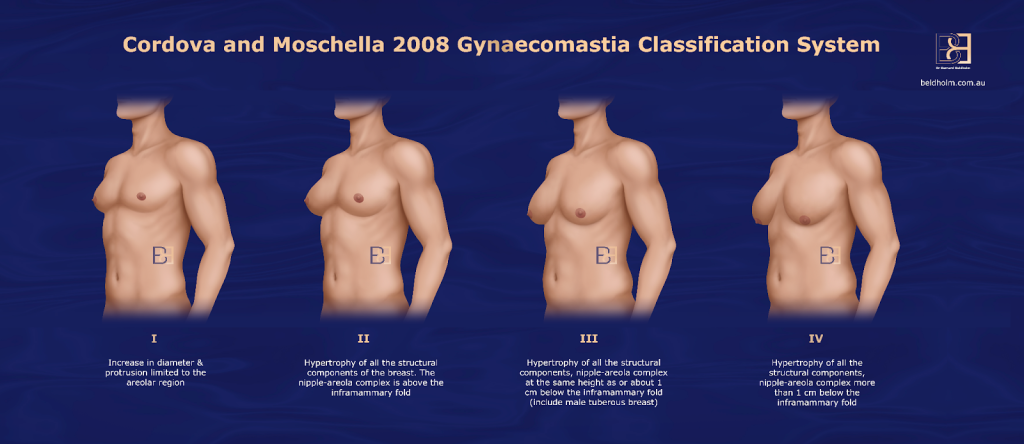
Cordova and Moschella Gynaecomastia Classification System
The Cordova and Moschella Gynaecomastia Grading System was developed to provide a more detailed classification of gynaecomastia, based on both clinical and anatomical features. This grading system arose from the need to offer a more comprehensive and practical approach to evaluate the severity and characteristics of gynaecomastia, which would help guide treatment options, particularly for surgical interventions.
How the System Came to be:
- Observational Basis: Cordova and Moschella based their system on a detailed clinical examination of patients with gynaecomastia. They observed that the condition manifests with various degrees of breast tissue enlargement, skin excess, and the presence of fatty tissue.
- Need for Precision: Prior to this, other systems existed but lacked precision in the variability in tissue types (glandular, fat, or both) and the presence of skin excess. The new classification aimed to categorise gynaecomastia in a way that directly influenced the choice of surgical or non-surgical treatment.
- Differentiation of Glandular and Fat Components: The Cordova and Moschella system distinguishes between the glandular and fatty components of gynaecomastia. It also factors in the degree of ptosis and skin redundancy, which previous systems did not emphasise enough.
- Comprehensive Grading: This system introduced a more detailed grading scale to better inform surgical planning, whether the patient needs suction-assisted lipectomy, excision of glandular tissue, skin reduction, or a combination of procedures.
- Influence on Treatment: By classifying gynaecomastia into different grades based on tissue composition and skin excess, the system helps surgeons select the most appropriate technique for each patient. Lower grades may involve excision or suction-assisted lipectomy, while higher grades may require more complex surgeries, including skin tightening procedures.
Cordova and Moschella Gynaecomastia Grading System
Grade I
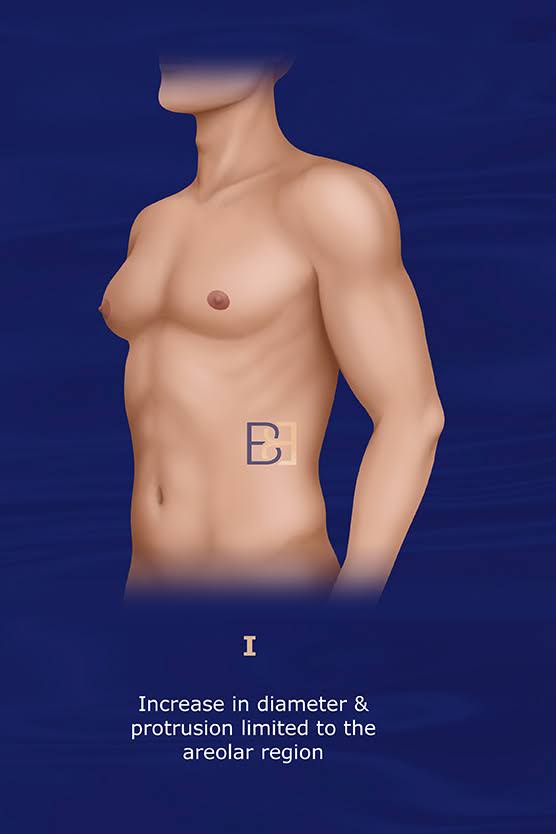
Presentation:
- Increased diameter and protrusion limited to aolar region.
Treatment:
- Subcutaneous mastectomy through an infra-areolar incision.
- Suction-assisted lipectomy not required.
Grade II

Presentation:
- Hypertrophy of all structural components of the breast.
- NAC (Nipple Areolar Complex) is above the IMF (Inframammary Fold)
Treatment:
- Ultrasound-assisted liposuction
- Subcutaneous mastectomy through an infra-areolar incision.
Grade III
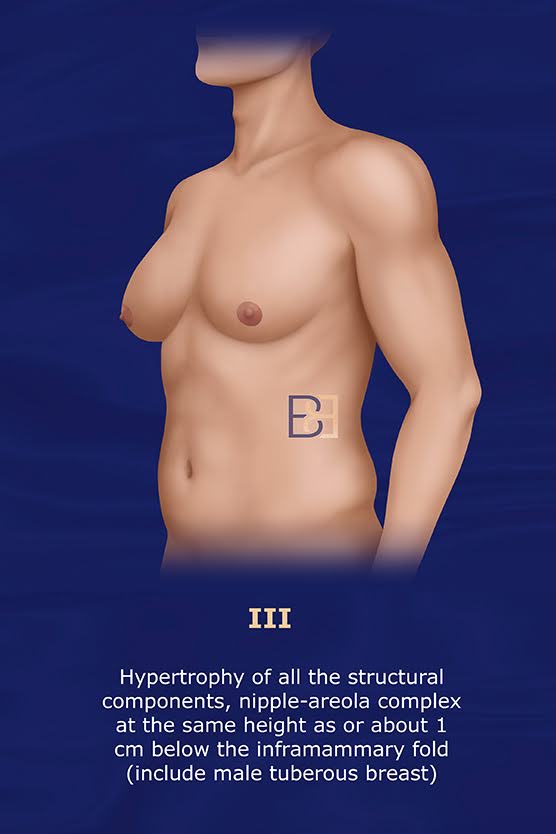
Presentation:
- Hypertrophy of all structural components of the breast.
- NAC (Nipple Areolar Complex) at the same height or 1 cm below the IMF (Inframammary Fold)
- Includes Male Tuberous Breast
Treatment:
- Ultrasound-assisted liposuction
- Subcutaneous mastectomy through an infra-areolar incision.
- Circular removal of skin around the NAC with a round block structure
Grade IV
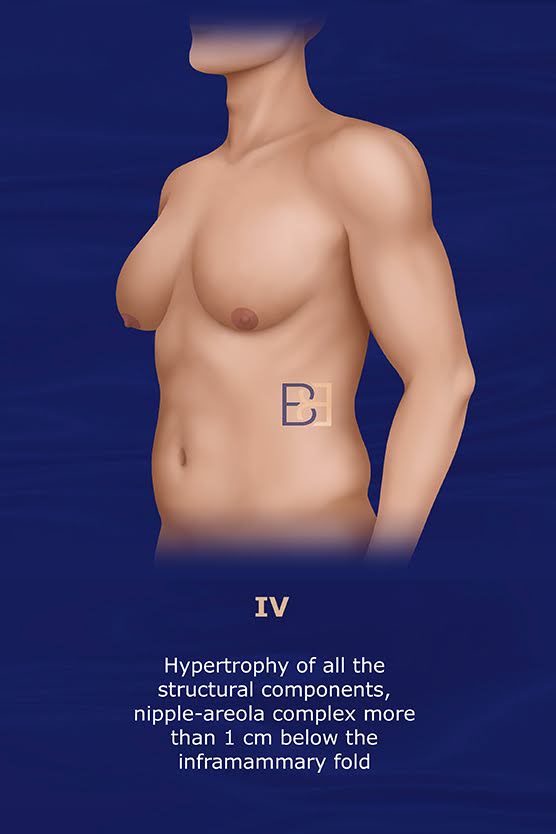
Presentation:
- Hypertrophy of all structural components of the breast.
- NAC (Nipple Areolar Complex) at the same height or 1 cm below the IMF (Inframammary Fold)
Treatment:
- Central pedicle reduction mastectomy techniques
- No liposuction required
Advantages of the Cordova and Moschella System
The Cordova and Moschella Classification System for gynaecomastia offers several advantages that have made it a valuable tool for both surgeons and patients. A precise focus on anatomical features and flexibility in guiding surgical treatments are key strengths.
These are the advantages:
Holistic, Multi-Dimensional Approach
Though the system focuses on the size of the breast tissue, it also takes factors such as skin excess, glandular and fatty tissue composition, and the degree of loose skin (ptosis) into account.
Differentiates Between Glandular and Fatty Components
By differentiating between the glandular and fatty components, the system allows for more precise diagnoses and treatment planning.
Guides Surgical Decisions
The classification helps surgeons choose the best approach for each grade. Lower grades may only require liposuction, for example, while higher grades might need excision or more extensive glandular resection.
Predicts Surgical Complexity
By categorising the severity of gynaecomastia and ptosis, the system predicts the complexity of the surgery needed. This helps with patient counselling and treatment planning.
Tailored Surgical Approaches
The system encourages personalised treatments based on individual characteristics, leading to better aesthetic outcomes. Because treatment can be more tailored, patients experience better results.
Standardised Language
The classification provides a standardised way for surgeons to describe gynaecomastia, which facilitates communication between patients and their surgeons.
Accommodates Various Body Types
The system accommodates a range of body types and varying degrees of severity, making it applicable to a wide range of patients.
Ptosis and Skin Laxity
Many classification systems overlook skin laxity or ptosis, but Cordova and Moschella incorporate these factors, which are essential for planning skin-tightening procedures.
Anticipates Complications
The system’s grading allows surgeons to anticipate challenges during surgery, which can minimise complications and recovery times.
Focus on Aesthetic Outcomes
Because the system classifies according to the amount of excess skin and tissue composition, surgical outcomes are not just functional but also aesthetically pleasing.
Disadvantages of the Cordova and Moschella Classification System for Gynaecomastia
While the Cordova and Moschella Classification System for gynaecomastia offers many advantages, it also has certain limitations which can affect its applicability and usefulness in clinical practice.
Complexity in Classification
Because the system incorporates multiple factors and makes it more comprehensive and complex, it is harder for less experienced surgeons to use or understand.
Time-Consuming
Accurately assessing all the factors involved (e.g., glandular tissue, fat, skin excess, ptosis) can be more time-consuming during evaluations.
Subjectivity in Application
Evaluating skin excess, ptosis, and tissue composition can be somewhat subjective, leading to surgical planning and outcomes variability.
Lack of Objective Measurement
The system relies on visual and manual assessments without the use of standardised, objective tools, which may lead to inconsistent classifications between providers.
Geared Only Towards Surgical Interventions
The system is heavily geared toward guiding surgical interventions and does not offer insight into non-surgical treatment options.
Doesn’t Account for Underlying Causes
While it is useful for surgical planning, the classification does not account for the underlying causes of gynaecomastia.
Focus on Advanced Cases
The system is useful for more advanced cases of gynaecomastia; however, it does not provide significant benefits in guiding treatment for mild or early-stage gynaecomastia.
Limited Global Use
Because the Cordova and Moschella system is not as widely adopted as some other systems, some surgeons still prefer more widely known grading systems.
Lack of Comparative Studies
Fewer comparative studies validating the superiority of this classification system over others make it difficult to determine whether it offers significant advantages.
Does Not Factor In Psychological Impact
Gynaecomastia often has psychological and emotional implications for patients. This system focuses purely on anatomical features and surgical treatment, with no guidance on psychological aspects.
Summary
The Cordova and Moschella Classification System stands out for its detailed, treatment-oriented approach, its adaptability to various body types, and its ability to guide both surgeons and patients toward the best possible outcomes in gynaecomastia treatment. Its tailored, patient-specific approach helps to improve surgical results and overall outcome.
The system has limitations in terms of complexity, subjectivity, and its focus on surgical treatment; however, this makes it less applicable for less experienced surgeons, patients with mild cases, or non-surgical management. Additionally, it does not focus on the underlying causes or psychological aspects of gynaecomastia.
Dr Bernard Beldholm’s Take

Having reviewed and referred to this classification system over the years, Dr Bernard offers these thoughts regarding this method:
- The Cordova and Moschella Gynaecomastia Grading System is a useful tool in both clinical practice and research, helping standardise treatment approaches and examining patient outcomes in the management of gynaecomastia.
- It takes the position of NAC (Nipple-areola complex) and gland excess into account.
- It is not very precise, however, as it frames the excess as “hypertrophy” and does not give a good sense of the extent of hypertrophy.
- In grade 4, I would recommend excision of the skin with NAC grafts.
References
- Nicolis GR, Modlinger RS, Gabrilove JL. A study of the histopathology of human gynaecomastia. J Clin Endocrinol Metab 1971;32:173e8.
- Mazur T, Clopper RR. Pubertal disorders. Psychology and clinical management. Endocrinol Metab Clin North Am 1991;20:211.
- Wilson JD. The pathogenesis of gynecomastia. Adv Intern Med 1980;25:1.
- Glass AR. Gynecomastia. Endocrinol Metab Clin North Am 1994;23:825.
- Rohrich R, Ha R, Kenkel J, et al. Classifications and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plast Reconstr Surg 2003;111:909e23.
- Bannayan GA, Haidu SI. Gynecomastia: clinicopathologic study of 351 cases. Am J Clin Pathol 1972;57:431e7.
- Andersen JA, Gram JB. Gynecomasty: Histological aspects in a surgical material. Acta Pathol Microbiol Immunol Scand [A] 1982;90:185e90.
- Nydick M, Bustos J. Gynecomastia in adolescent boys. JAMA 1961;178:449e54.
- Croce P, Montanari G, Zinzalini G, et al. Gynecomastia. Minerva Med 1992;83:609e14.
- Simon BE, Hoffman S, Kahn S. Classification of gynecomastia. Plast Reconstr Surg 1973;51:48e52.
- Deutinger M, Freilinger G. Gynecomastia: attempt at a classification and surgical results. Handchir Mikrochir Plast Chir 1986;18:239e41.
- Cohen KI. Gynecomastia: suction lipectomy as a contemporary solution. Plast Reconstr Surg 1987;80:386.
- Lejour M. Evaluation of fat in breast tissue removed by vertical mammoplasty. Plast Reconstr Surg 1997;99:386e93.
- Gasperoni G, Salgarello M, Gasperoni P. Technical refinements in the surgical treatment of gynecomastia. Ann Plast Surg 2000;44:455e8.
- Benelli L. A new periareolar mammoplasty: round block technique. Aesthetic Plast Surg 1990;14:99.
- Ohyama T, Takada A, Fujikawa M, et al. Endoscope assisted transaxillary removal of glandular tissue in gynecomastia. Ann Plast Surg 1998;40:62.
- Hammond D, Arnold JA, Simon AM, et al. Combined use of ultrasonic liposuction with the pull-through technique for the treatment of gynecomastia. Plast Reconstr Surg 2003;112:891. Discussion by Rorich R., Ha R.Y.
- Hemsell D, Edman C, Marks J, et al. Massive extraglandular aromatization of plasma androstenedione resulting in feminization of a prepubertal boy. J Clin Invest 1977;60:455e64.
- Bulard J, Mowskowicz I, Schaison G. Increased aromatase activity in pubic skin fibroblast from patients with isolated gynecomastia. Clin Endocrinol Metab 1987;64:618e23.
- Webster JP. Mastectomy for gynecomastia through a semicircular intraareolar incision. Ann Surg 1946;124:557.
- Morselli PG. ‘‘Pull-through’’: a new technique for breast reduction in gynecomastia. Plast Reconstr Surg 1996;97:450e4.
- Murphy TP, Ehrlichman RJ, Seckel BR. Nipple placement in simple mastectomy with free nipple grafting for severe gynecomastia. Plast Reconstr Surg 1993;94:818.
- Davidson BA. Concentric circle operation for massive gynecomastia to excise redundant skin. Plast Reconstr Surg 1979;65:350.
- Huang TD, Hidalgo JE, Lewis SR. A circumareolar approach insurgical management of gynecomastia. Plast Reconstr Surg 1982;69:35.
- Smoot EC. Eccentric skin resection and purse string closure for skin reduction with mastectomy for gynecomastia. Ann Plast Surg 1998;41:378.
- Persichetti P, Berloco M, Casadei RM, et al. Gynecomastia and the complete circumareolar approach in surgical management of gynecomstia. Plast Reconstr Surg 2001;107:948e54.
- Tashkandi M, Al-Qattan MM, Hassanain JM. The surgical management of high-grade gynecomastia. Discussion of Sadove A.M. Ann Plast Surg 2004;53:17e21
- Wiesman IM, Lehan JA, Parker MG, et al. Gynecomastia. An outcome analysis. Ann Plast Surg 2004;53:97e101.
- Fruhstorfer BH, Malata CM. A systematic approach to the surgical treatment of gynecomastia. Br J Plast Surg 2003;56:237e46.
- Hamilton S, Gault D. The tuberous male breast. Br J Plast Surg 2003;56:295e300.
- Wuringer E. Refinement of the central pedicle breast reduction by application of the ligamentous suspension. Plast Reconstr