In my experience as a specialist surgeon with expertise in body contouring surgery after massive weight loss, understanding the possible risks and outcomes is one of the most important parts of surgical planning. Patients who have experienced significant weight loss—whether through bariatric surgery, gastric bypass, or lifestyle changes—often seek an abdominoplasty (tummy tuck) to remove excess skin, tighten abdominal muscles. However, as with all surgery, this is a major surgical procedure, and understanding the complications from abdominoplasty (tummy tuck) post weight loss is vital for informed decision-making.

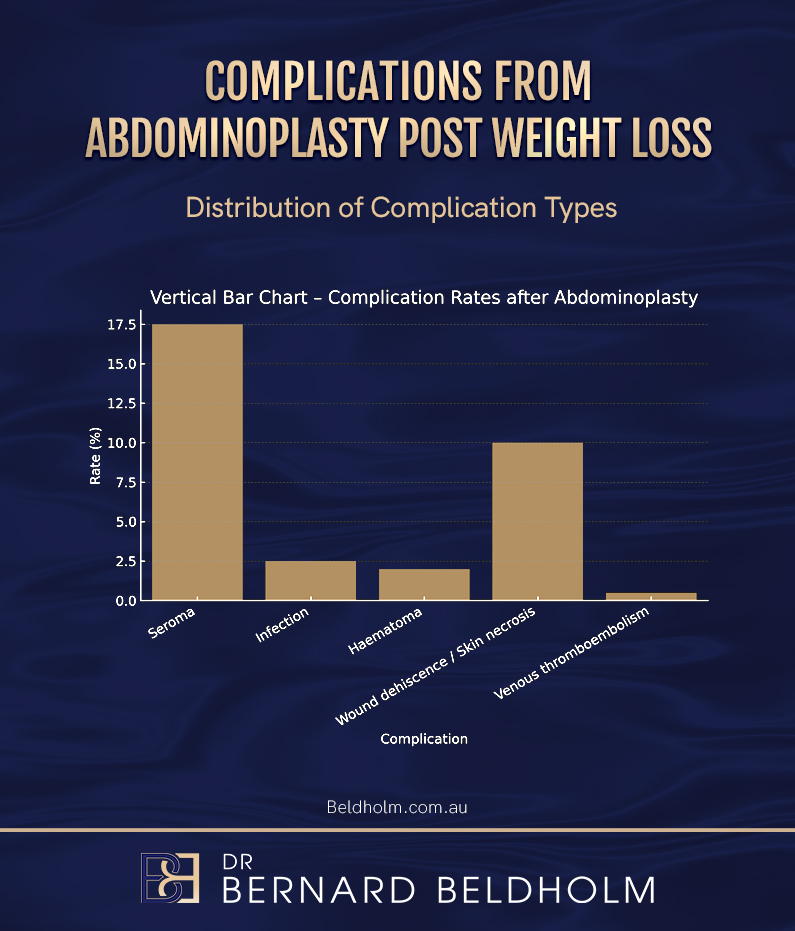
Studies show that overall complication rates after abdominoplasty following major weight loss range from 18% to 53%, depending on the patient’s health and the extent of surgery. Within this range, minor complications—such as wound healing issues, seroma, and small infections—occur in approximately 15–30% of cases. Major complications, which include events requiring hospitalisation or reoperation like bleeding or blood clots, are far less frequent at around 2–4% (Chaker 2024; Winocour 2015; Myszkowska 2025). These statistics highlight the importance of planning and patient optimisation before surgery.
This article reviews my clinical experience and scientific literature, including findings from the Aesthetic Surgery Journal and other leading plastic surgery international publications. It covers both minor complications and major complications, as well as risk factors, recovery tips, and prevention strategies to help patients feel informed before undergoing body contouring after massive weight loss.
Understanding the Scope of Abdominoplasty after Weight Loss
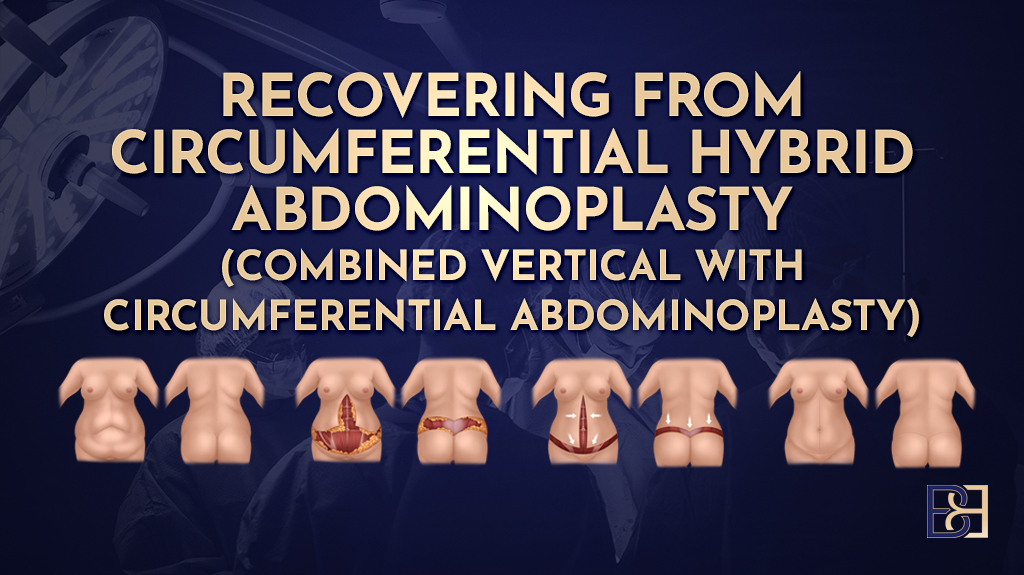
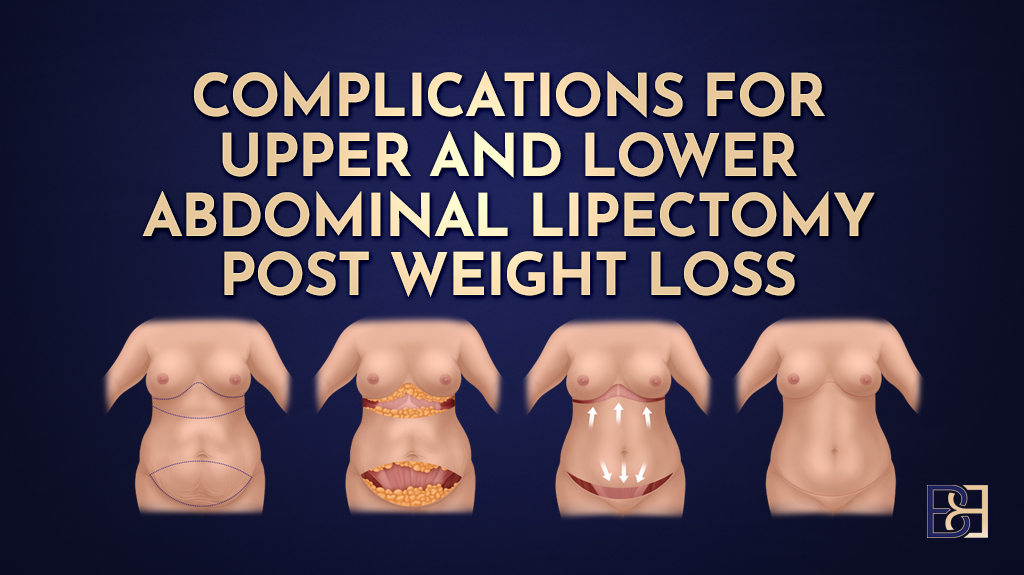
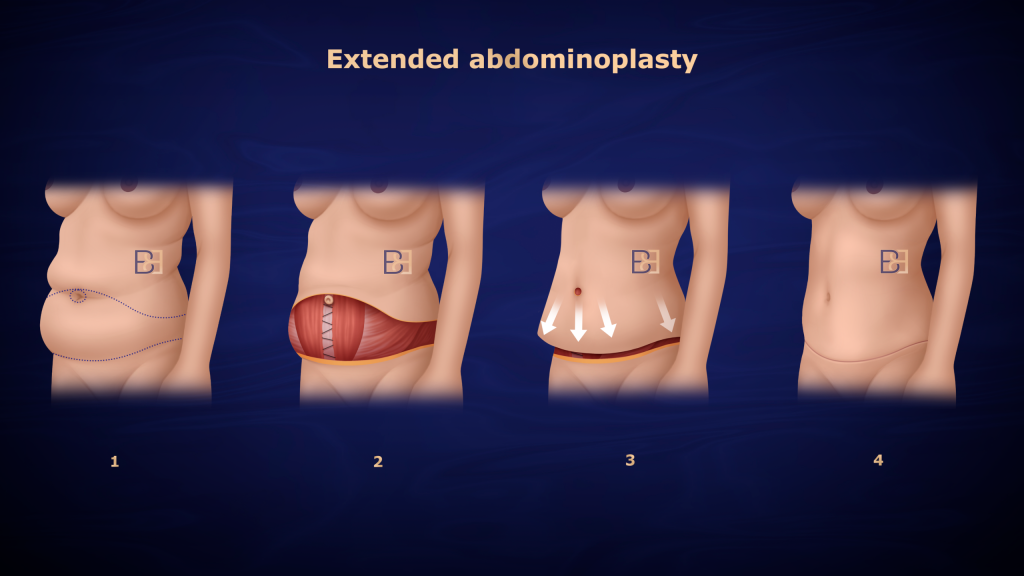
In this article, I focus on standard and extended abdominoplasty—two of the most common body contouring procedures performed following massive weight loss. These techniques are designed to remove excess skin, strengthen the underlying muscles, and provide abdominal support. Other related procedures, such as fleur-de-lis abdominoplasty, circumferential abdominoplasty, abdominal lipectomy, and apronectomy, focus on other areas; these are discussed in separate articles on my website.
What this means for patients:
If you are considering an abdominoplasty after weight loss surgery, this information will help you understand both the expected benefits and the possible risks, including postoperative complications and delayed wound healing.
Why Complications Are More Common after Major Weight Loss
In both clinical experience and research, patients who have undergone obesity surgery or experienced major weight loss present unique anatomical and metabolic challenges that increase the likelihood of complications. Factors include:
- Excess skin and tissue laxity: The abdominal skin may have been stretched for years, reducing elasticity and blood flow, which increases the risk of wound healing problems.
- Nutritional deficiencies: Post bariatric surgery patients—especially after gastric bypass—may have reduced protein and vitamin absorption, contributing to poor wound healing.
- Comorbidities: Conditions like diabetes mellitus, anaemia, and elevated body mass index (BMI) are well-documented risk factors for complications.
- Longer surgical incision and greater resection weight: Removing large amounts of tissue increases operative time and strain on the wound.
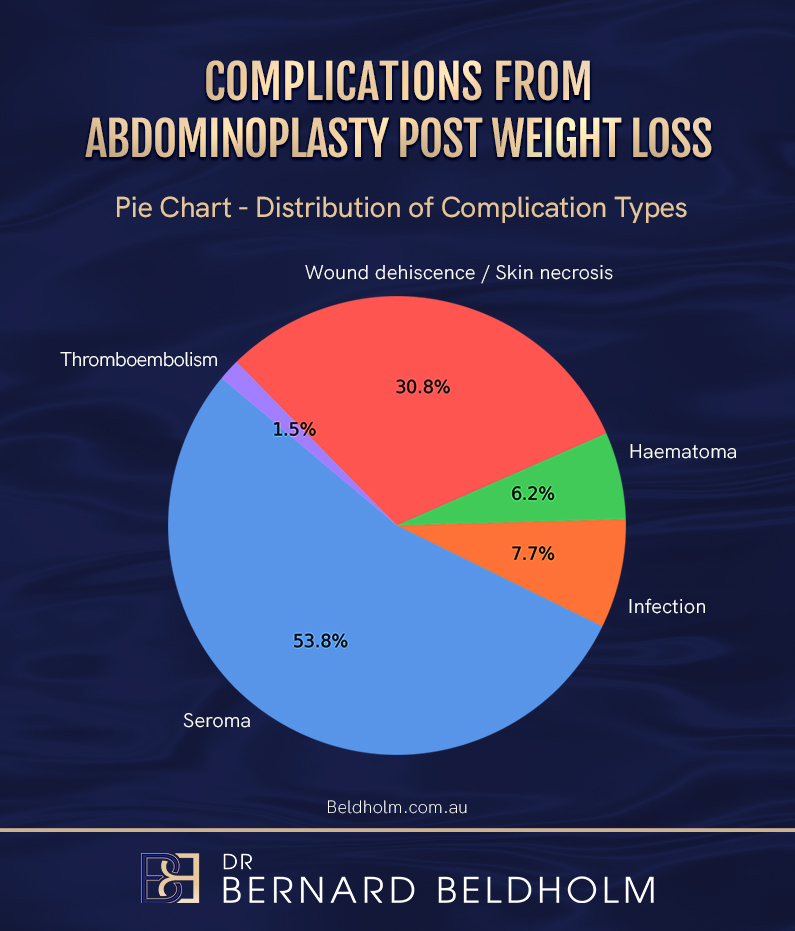
According to Myszkowska et al. (2025), complication rates among post-bariatric patients range from 18–53%, compared with 5–10% in typical cosmetic surgeries. These findings, supported by the Aesthetic Surgery Journal and the Society of Plastic Surgeons, mirror what I see in practice: patients who have experienced massive weight loss require meticulous preparation, careful planning, and tailored surgical techniques.
What this means for patients:
Reaching a stable weight close to your goal before surgery and optimising your nutrition significantly reduces risk. Preoperative assessment and risk factor analysis help specialist surgeons identify and manage potential complications.
Book your appointment online now
Common Complications after Abdominoplasty
Wound-Related Complications and Seroma Formation
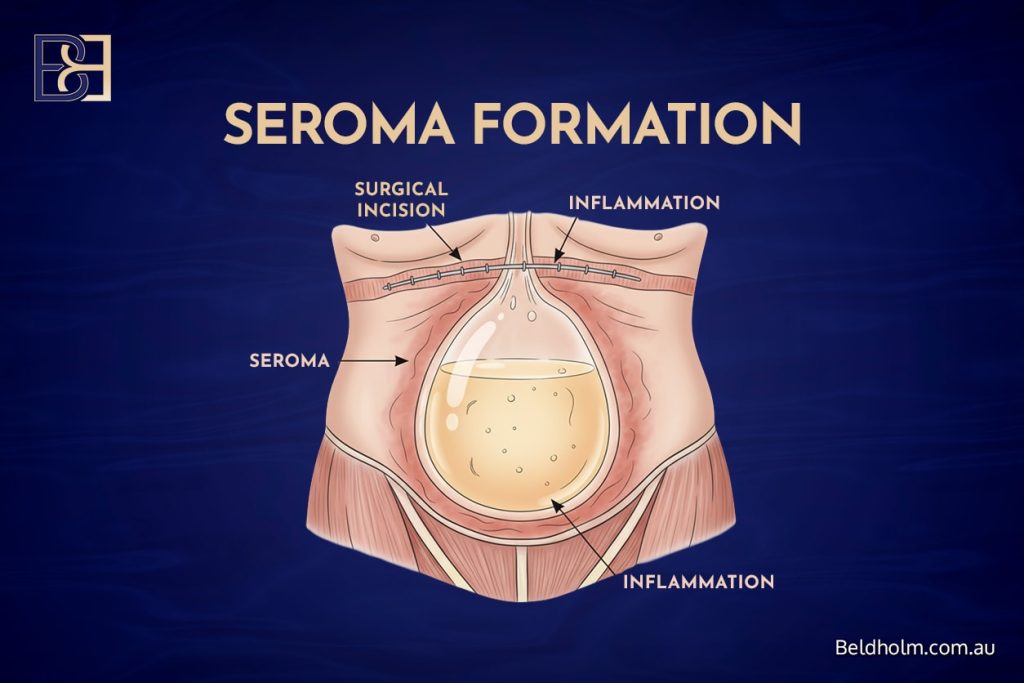
In my practice, wound infections, delayed wound healing, and seroma formation are the most frequent issues. A seroma is a pocket of fluid that forms beneath the skin after surgery. Studies such as Myszkowska et al. (2025) report a seroma rate of 23.6% in post-weight-loss abdominoplasty patients, while Liao et al. (2024) show that using progressive-tension sutures and Scarpa’s fascia preservation can lower this to under 5%.
Wound infections occur in 1–4% of patients, and wound separation (dehiscence) may appear in up to 10–15%. These postoperative complications are usually managed with wound dressings, antibiotics, or minor procedures.

What this means for patients:
Fluid collection or minor wound issues are common in plastic and reconstructive surgery, especially for obese and nonobese patients after body contouring. Regular reviews and proper care promote smoother recovery.
Haematoma and Postoperative Bleeding
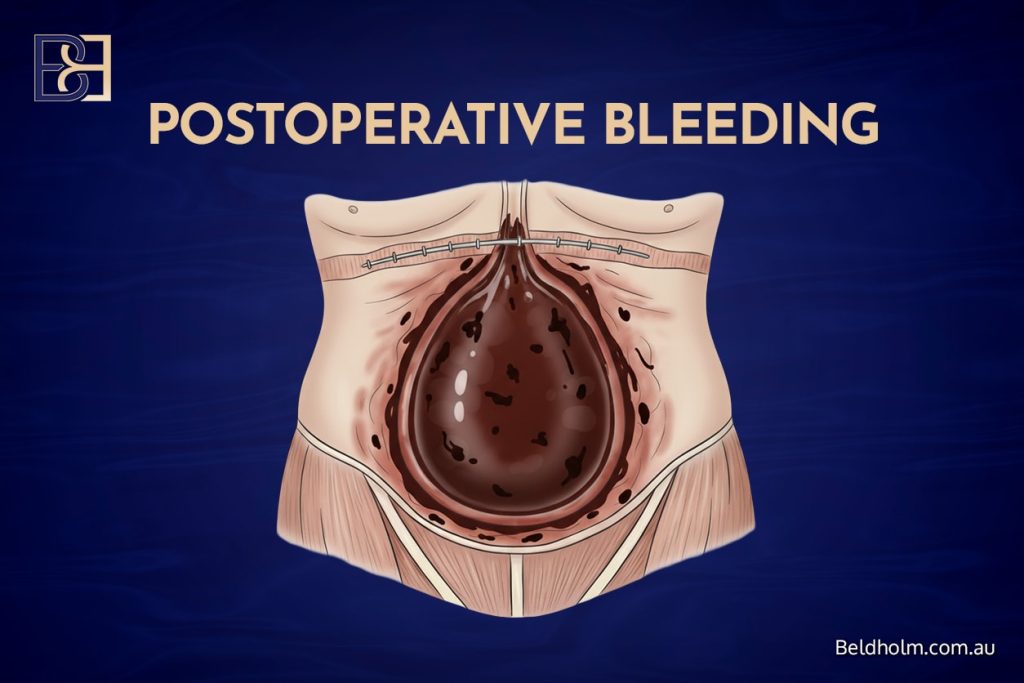
Haematoma, or internal bleeding under the skin, is less frequent but still important to recognise. It occurs in about 2–7% of cases. The large outcomes analysis by Chaker et al. (2024) reviewed 55,596 abdominoplasties and found major complications requiring hospital care in 2.1% of cases. Good surgical technique and meticulous haemostasis reduce this risk.

What this means for patients:
If you notice sudden swelling, tightness, or increased pain at the surgical site, contact your care team immediately. Early recognition prompts early treatment and better healing.
Scarring and Contour Irregularities
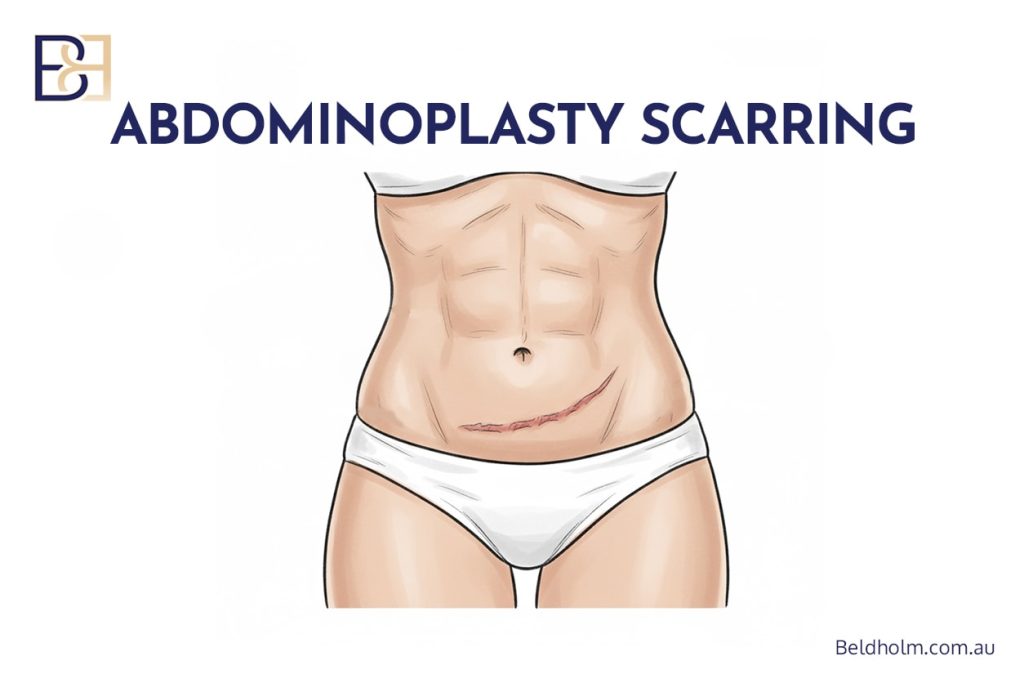
All tummy tuck (abdominoplasty) operations leave scars. These are typically positioned low on the abdomen. Extended abdominoplasty extends the scar around the flanks to remove loose skin from the sides of the waist, while only fleur-de-lis abdominoplasty involves a vertical scar to remove excess skin in the horizontal direction. There are several aspects of scarring that are important to understand. The tension on the incision plays a major role in how scars mature — too much tension can cause the scar to widen over time. Infection or wound-healing issues may contribute to raised or thickened scars, known as hypertrophic scars. The colour of scars can also vary; some may become hyperpigmented (dark) or hypopigmented (light) depending on skin type and healing response. Sun exposure during the healing phase can darken scars, and patients with darker or olive-toned skin are sometimes more prone to visible or uneven scarring. Gentle sun protection and silicone-based scar treatments can help with outcomes.
What this means for patients:
Scar visibility varies by skin type, surgical tension, and genetics. Most scars fade significantly within 6–12 months.
Nerve-Related Complications
Temporary Numbness and Sensory Changes
It is common to experience numbness in the lower abdomen after abdominoplasty. This occurs because small sensory nerves under the skin are disrupted during the procedure. The numbness usually settles over time as the nerves regenerate. Most patients notice a gradual return of sensation within the first 3 months, although complete recovery can sometimes take longer.
Nerve Pain and Discomfort
Some patients experience nerve-related pain, tingling, or shooting sensations as nerves heal. This may be temporary but can occasionally last several months. Very rarely, patients develop chronic nerve pain in the abdominal wall or along the upper thigh due to irritation or injury to small cutaneous nerves during surgery. This type of pain is uncommon and can usually be managed with medications or nerve desensitisation treatments if needed.
What this means for patients:
Temporary numbness is normal after surgery and typically improves without treatment. If persistent discomfort or nerve pain occurs, it can often be managed effectively with support from your surgical team.
Less Common Complications
Skin or Umbilical Necrosis
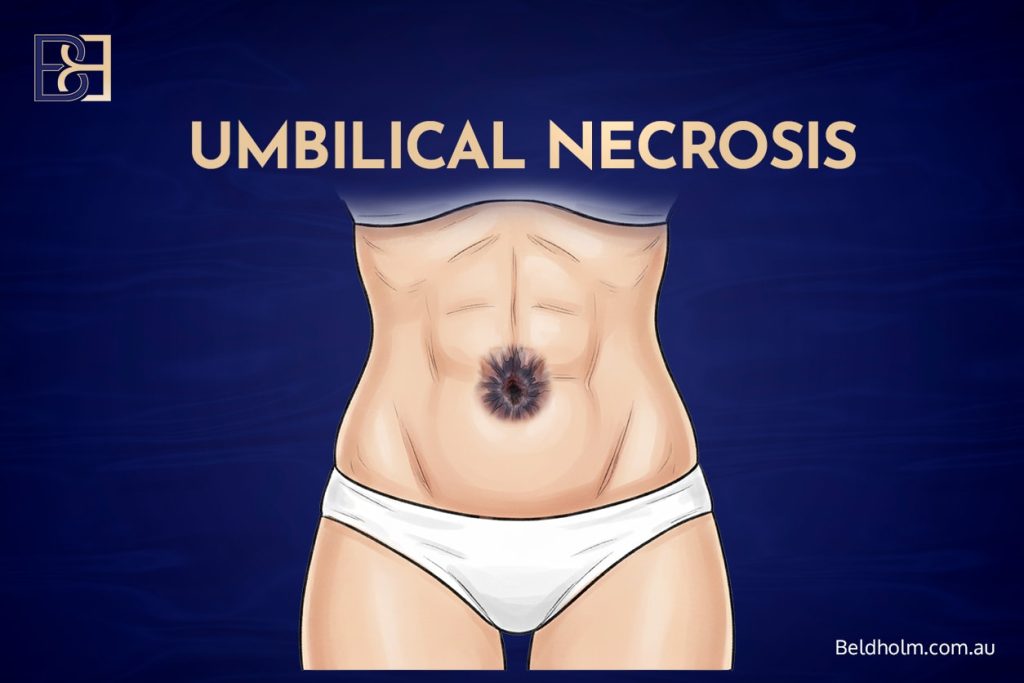
Reduced blood flow may occasionally cause skin necrosis or belly button loss (umbilical necrosis). Rates are low—usually under 3%—and often related to smoking or pre-existing vascular disease. Cannizzaro et al. (2024) reported skin necrosis in just 0.6% of 500 post-bariatric surgery patients.
What this means for patients:
Small areas heal over several weeks with dressings, but avoiding smoking is one of the best ways to minimise this risk.
Fat Necrosis
Fat necrosis occurs when small fat deposits lose blood supply, creating firm lumps under the skin. Reported in up to 3% of cases, it is a minor complication that typically resolves on its own.
Wound Dehiscence
Large wound separations are uncommon but may appear in 3–10% of post-bariatric patients (Sadeghi et al., 2022). These are managed conservatively with dressings or, rarely, minor closure procedures.
What this means for patients:
Wound separations usually heal over time and do not affect long-term results.
Serious but Uncommon Complications
Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
Deep vein thrombosis and pulmonary embolism are rare but serious major complications. Research shows an incidence of 0.5–2% in abdominoplasty patients (Myszkowska et al., 2025; Sadeghi et al., 2022). Preventive steps include low molecular weight heparin, compression boots, and early ambulation after surgery.
What this means for patients:
Blood clots are among the most serious postoperative complications in surgery. Early movement and hydration during the immediate postoperative period help reduce the risk.
Major Bleeding and Reoperation
Significant bleeding that requires surgical treatment or transfusion occurs in about 1% of cases. Large database reviews published in the Aesthetic Surgery Journal confirm that proper technique and monitoring help reduce these risks.
Anaesthetic and Systemic Complications
Anaesthetic complications occur in fewer than 1% of healthy patients. Preoperative assessment by a qualified anaesthetist is essential for planning surgery.
Very Rare Complications
Extremely rare risks (<0.1%) include severe infection, organ injury, and postoperative mortality. Matarasso (2006) and Winocour (2015) both report that mortality rates for abdominoplasty remain under 0.1%. These events are discussed in academic contexts within aesthetic surgery and reconstructive surgery literature to support transparency and awareness.
Risk Factors That Influence Outcomes

Multiple studies confirm that patient-specific and operative factors contribute to outcomes and complications.
Risk Factor | Influence on Complications |
|---|---|
High BMI (≥30 kg/m²) | Doubles the likelihood of wound and seroma formation |
Smoking | Reduces blood flow and delays wound healing |
Diabetes / poor nutrition | Increases infection and delayed recovery |
Large tissue resection | Higher chance of bleeding and fluid accumulation |
Prolonged surgery time | Slightly increases infection and clot risks |
What this means for patients:
Maintaining a stable weight, good diet, and avoiding smoking before surgery all contribute to lower complication rates.
Preventing Complications
Reducing potential complications involves collaboration between patient and surgeon. Evidence-based strategies in surgery include:
- Preoperative optimisation: Correcting nutritional deficiencies and treating comorbidities.
- Precise surgical incision planning: Preserving blood supply and limiting tissue strain.
- Use of drains and progressive-tension sutures: Reducing seroma and haematoma.
- Compression garments: Supporting healing and reducing swelling.
- Early mobility: Minimising risk of deep vein thrombosis and pulmonary embolism.
What this means for patients:
Adhering to medical advice, attending scheduled reviews, and reporting any symptoms that are concerning early will help with recovery outcomes.
Frequently Asked Questions
What is the most common complication after abdominoplasty?
The most common complications are wound-healing problems and seroma formation. These are generally mild and treatable with conservative care.
Are complications more common after weight loss surgery?
Yes. Post bariatric patients have a higher likelihood of wound complications and fluid collection due to altered skin quality and blood flow.
What happens if you lose weight after abdominoplasty?
If you continue to lose weight after surgery, you may develop new areas of excess skin. It’s best to reach a stable weight close to your goal before surgery for predictable results.
How long does it take to fully recover from a tummy tuck (abdominoplasty)?
Most people return to light activity within 2–4 weeks. Full recovery, including softening of the abdominal area and scar maturation, may take up to 12 months.
Why is my stomach rock hard after a tummy tuck (abdominoplasty)?
This firmness is part of the natural healing process. The surgical area usually softens within several months as swelling subsides and the tissue relaxes.
Conclusion

In my experience treating obese patients and those who have experienced massive weight loss, abdominoplasty (tummy tuck) procedures can help with function, though outcomes vary. Common abdominoplasty complications such as seroma, wound infections, and wound healing issues are generally manageable, while deep vein thrombosis, pulmonary embolism, and major complications are rare. Performing surgery in accredited facilities under qualified specialist surgeons is important for your safety.
For patients:
Learning about possible complications of abdominoplasty, preparing your health in advance, and following post-operative guidance will support healing and help you feel informed throughout your body contouring journey.
References (Vancouver Style)
- Myszkowska B, Zawada-Wiśniewska P, Handzlik I, Krakowiak M. Complications following abdominoplasty in post-weight loss patients: a systematic review and meta-analysis. South Asian Res J Bus Manag. 2025;7(5):413-9.
- Cannizzaro Hospital Group. Experience in post-bariatric abdominoplasty for patients with significant weight loss: a prospective study. J Pers Med. 2024;14(7):681.
- Chaker SC, Hung YC, Saad M, Perdikis G, Grotting JC, Higdon KK. Complications and risks associated with the different types of abdominoplasties: an analysis of 55,596 patients. Aesthet Surg J. 2024;44(9):965-75.
- Liao CD, Zhao K, Nikkhahmanesh N, Bui DT. Decreasing seroma incidence following abdominoplasty: a systematic review and meta-analysis of high-quality evidence. Aesthet Surg J Open Forum. 2024;6:o-jae016.
- Sadeghi P, Duarte-Bateman D, Ma W, Khalaf R, Fodor R, Pieretti G, et al. Post-bariatric plastic surgery: abdominoplasty, the state of the art in body contouring. J Clin Med. 2022;11(15):4315.
- Stein MJ, Karaev S, Matarasso A. A primer on abdominoplasty safety. Plast Surg (Oakv). 2024;32:e1-14.
- Winocour JN, Grotting JC, Higdon KK. The safety profile of abdominoplasty: analysis of 25,478 cases from the CosmetAssure database. Plast Surg (Oakv). 2024;32:e1-14.
- Matarasso A, Wallach SG, Rankin M, Galiano RD, Zienowicz R. Abdominoplasty survey: current practices and complications. Plast Reconstr Surg. 2006;117(6):1797-808.