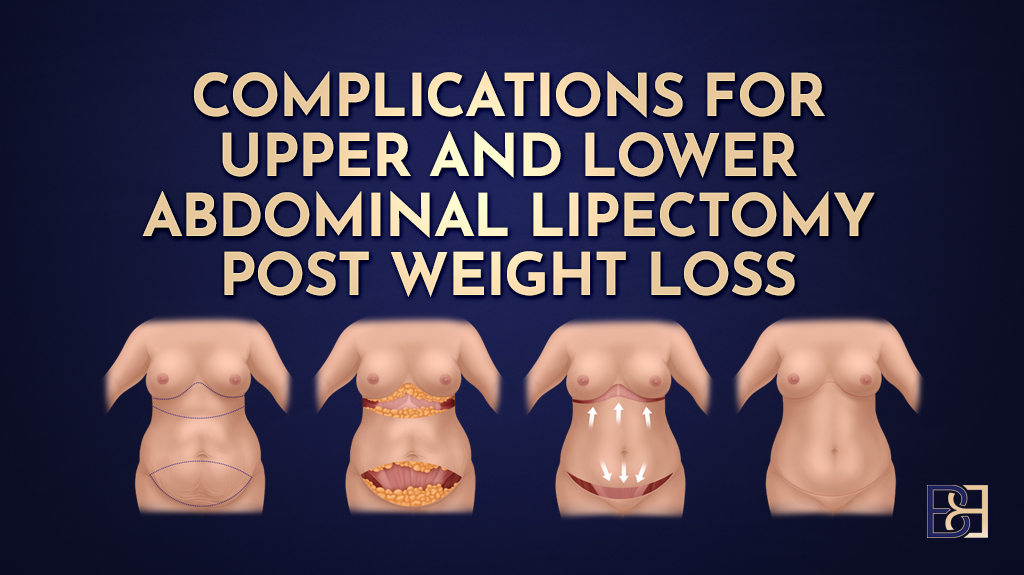
A Fleur-de-Lis abdominoplasty (also known as a Fleur-de-Lis tummy tuck) is a major surgical procedure designed to remove excess skin and tighten the abdominal wall following significant or massive weight loss or major weight loss. This type of reconstructive surgery is particularly beneficial for post-bariatric surgery patients who have undergone weight loss surgery such as gastric bypass or sleeve gastrectomy, or for those who have achieved significant weight loss through diet, exercise, or modern weight loss medications. These patients often experience substantial excess skin that drapes both vertically and horizontally.
In Maitland, Newcastle, and the Hunter Valley, Specialist Surgeon Dr Bernard Beldholm FRACS commonly performs this body contouring surgery at Maitland Private Hospital. While this surgical procedure can treat function, comfort, and body contouring outcomes, it also carries recognised surgical risks. Fleur de lis surgery carries specific risks such as bleeding, infection, and abnormal scarring, so consultation with a qualified surgeon is essential. Individual outcomes vary; appropriate preparation, planning, and risk assessment are essential for optimal healing.
This article provides an in-depth, evidence-based review of surgical complications for Fleur-de-Lis abdominoplasty post-weight loss. It compares Fleur-de-Lis abdominoplasty outcomes to other abdominoplasty surgery techniques and examines risk factors, complication rates, and treatment options. Drawing from the latest publications in plastic and reconstructive surgery and aesthetic surgery journals, including the Aesthetic Surgery Journal as a key source for clinical data, this guide also discusses ways to support healing.
Understanding the Fleur-de-Lis Abdominoplasty
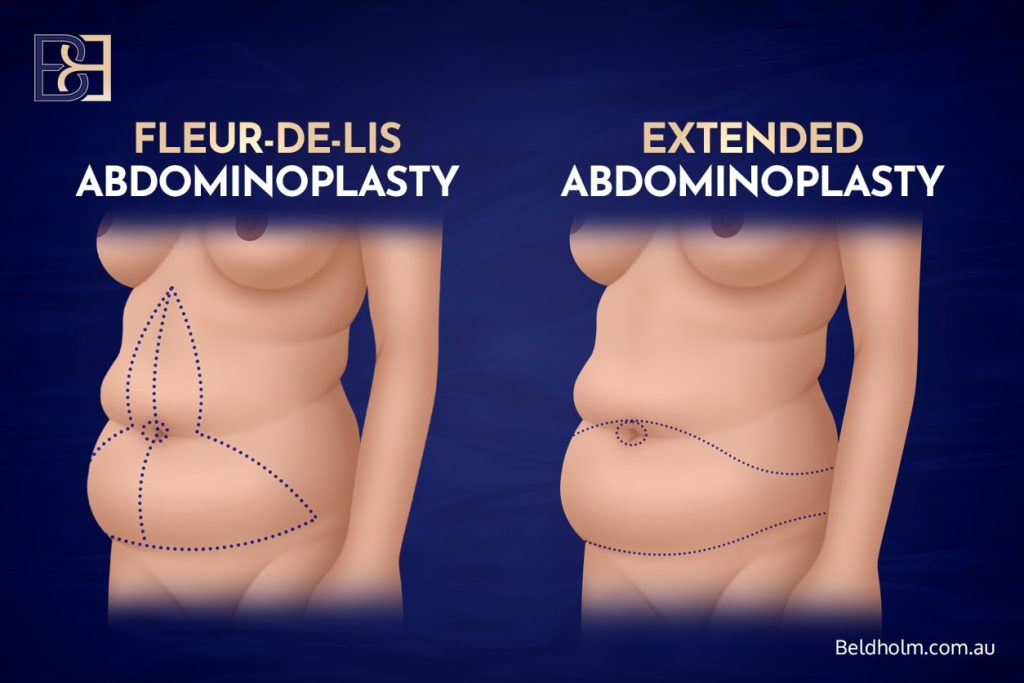
A Fleur-de-Lis abdominoplasty differs from a standard tummy tuck (abdominoplasty) or extended abdominoplasty by removing excess skin in two planes—vertical and horizontal. The surgical technique involves a horizontal incision along the lower abdomen combined with a vertical incision extending up the midline, creating an inverted “T” or fleur-de-lis pattern. This design enables the removal of significant excess skin and the tightening of the underlying abdominal muscles. Fleur de lis abdominoplasty is one of several surgical procedures available for patients with significant skin laxity after weight loss. It is particularly useful for post-bariatric patients and massive weight loss patients who have redundant abdominal skin that cannot be corrected through a single horizontal incision (3,4). Obese patients may face additional risks and healing challenges with this procedure.
Excess skin and fat are carefully excised during this surgical procedure while preserving essential blood vessels to maintain tissue health. The abdominal wall is tightened, and the remaining skin is re-draped. The surgery is performed under general anaesthesia and may be combined with other body contouring procedures such as lateral thigh lift (thighplasty), extended abdominoplasty, or liposuction (suction-assisted lipectomy). While this reconstructive surgery can help hygiene and comfort, it requires careful planning due to the risk of postoperative wound complications and delayed wound healing (5).
Why Choose Fleur-de-Lis Abdominoplasty After Significant Weight Loss Surgery
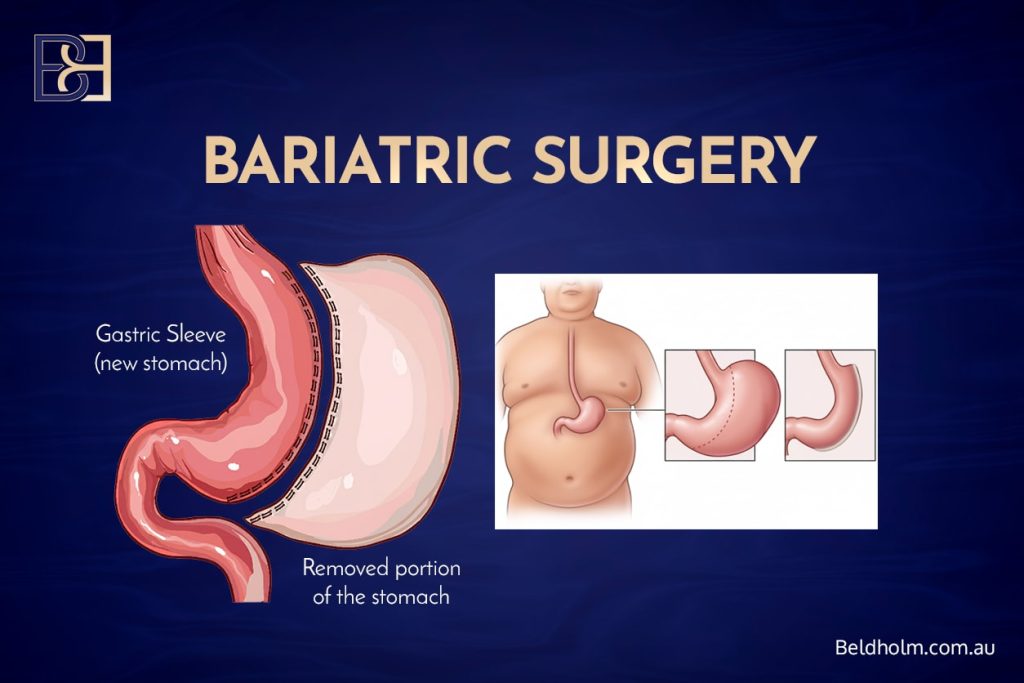
Following weight loss surgery such as gastric bypass or sleeve gastrectomy, patients often experience loose skin and significant skin laxity across the abdominal region. This can lead to rashes, discomfort, and challenges with clothing. The Fleur-de-Lis abdominoplasty is specifically designed for patients who need both vertical and horizontal excess skin removal. It provides greater tightening than a standard tummy tuck (abdominoplasty), treating both functional and aesthetic outcomes. However, the procedure’s complexity and increased incision length can result in a relatively high complication rate compared with simpler body contouring procedures (1,2,3).
Pre-Surgical Requirements
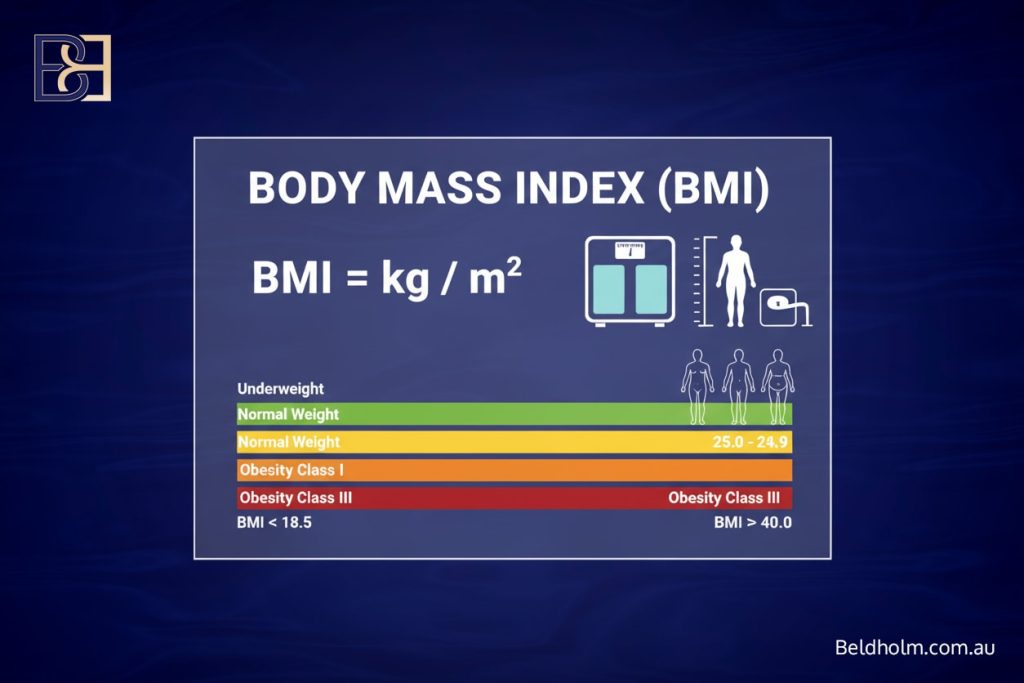
Before proceeding with body contouring surgery such as fleur de lis abdominoplasty, it is essential for patients to meet specific pre-surgical requirements to minimise the risk of postoperative complications and support optimal healing. Achieving a stable weight close to your goal is a critical first step, particularly for bariatric surgery patients and those who have experienced massive weight loss. Maintaining a stable body mass index (BMI) helps reduce the likelihood of wound complications, seroma formation, and other issues that can arise during the recovery process.
Optimising nutritional status is equally important. Nutritional deficiencies—common after bariatric surgery—can significantly impair wound healing and increase the risk of both minor complications like wound infections and major complications such as delayed wound healing. Patients are encouraged to follow a diet rich in protein, vitamins, and minerals, and may require supplements to treat any deficiencies identified during preoperative assessment.

Smoking cessation is another vital pre-surgical requirement. Smoking reduces blood flow to the surgical area, increasing the risk of wound infections, delayed healing, and other postoperative complications. Patients should stop smoking well in advance of their fleur de lis abdominoplasty to promote better outcomes.
A comprehensive medical evaluation is also necessary to identify and manage any underlying risk factors, such as diabetes, hypertension, or cardiovascular disease. These conditions can increase the risk of wound complications and deep vein thrombosis, so it is important for patients to work closely with their healthcare team.
Finally, setting realistic expectations is crucial for a positive surgical experience. While fleur de lis abdominoplasty is highly effective at removing excess skin, it may not eliminate all skin laxity or treat every concern. Patients should have open discussions with their specialist surgeon about the goals of the surgical procedure, the potential risks, and the expected recovery process. Understanding both the benefits and possible risks—including minor and major complications—helps patients make informed decisions and prepares them for a smoother recovery.
Complication Rates and Clinical Evidence
Book your appointment online now
Complication rates for Fleur-de-Lis abdominoplasty vary across studies due to patient factors and surgical techniques. A 2024 plastic and reconstructive surgery review of 55,596 abdominoplasty cases found that Fleur-de-Lis abdominoplasty had the highest major complication rate (2.1%) among seven abdominoplasty variants (1). The most common major complications were:
- Haematoma (0.7%)
- Wound infection (0.6%)
- Deep vein thrombosis (0.18%)
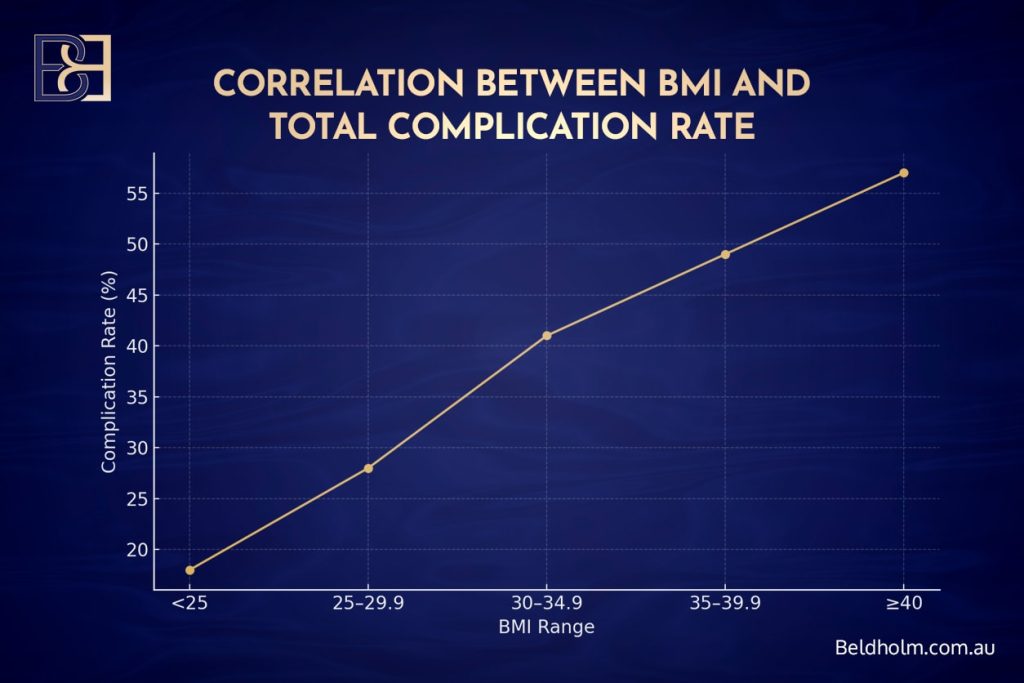
The study highlighted that diabetes, male sex, and abnormal body mass index (BMI) significantly increased complication risk.
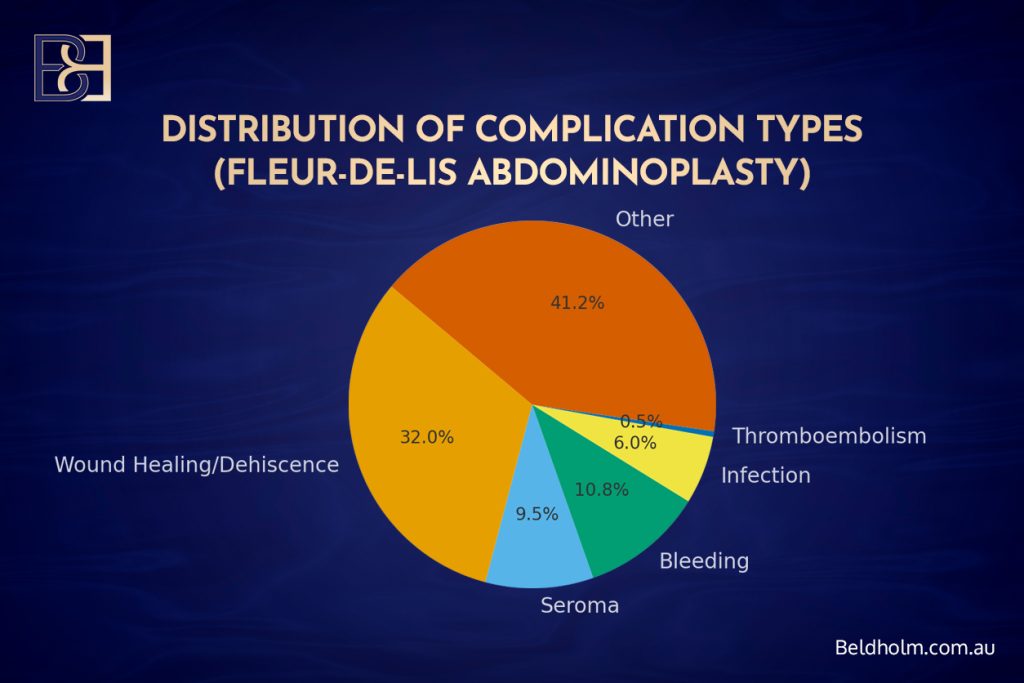
In a 2021 post-bariatric abdominoplasty study analysing 406 patients (2);
- Overall complication rates (41.9%)
- Wound healing problems (32%)
- Seroma (9.5%)
- Bleeding (10.8%)
Major complications such as thromboembolism were rare (0.5%). The researchers concluded that patient-related factors—particularly BMI, age, and resected tissue weight—had more influence on postoperative complications than the surgical technique itself.
Other studies in aesthetic surgery journals also show that while Fleur-de-Lis abdominoplasty has a higher rate of wound complications than traditional abdominoplasty, most are minor and managed with standard treatment protocols (3,4,5). These findings align with Dr Beldholm’s clinical experience in treating post bariatric surgery patients, where wound complications are typically manageable with conservative care.
Common Surgical Complications and Treatment Options
Haematoma

A haematoma is a localised collection of blood beneath the skin following abdominoplasty surgery. It may cause pain, bruising, or swelling (1,5).
Treatment Options:
- Small haematomas: Can be treated with a compression garment and observation.
- Large or expanding haematomas: Require urgent return to the operating theatre for evacuation and haemostasis.
- Haemoglobin levels are monitored postoperatively, and blood transfusion may be required in cases of significant blood loss (7).
Seroma
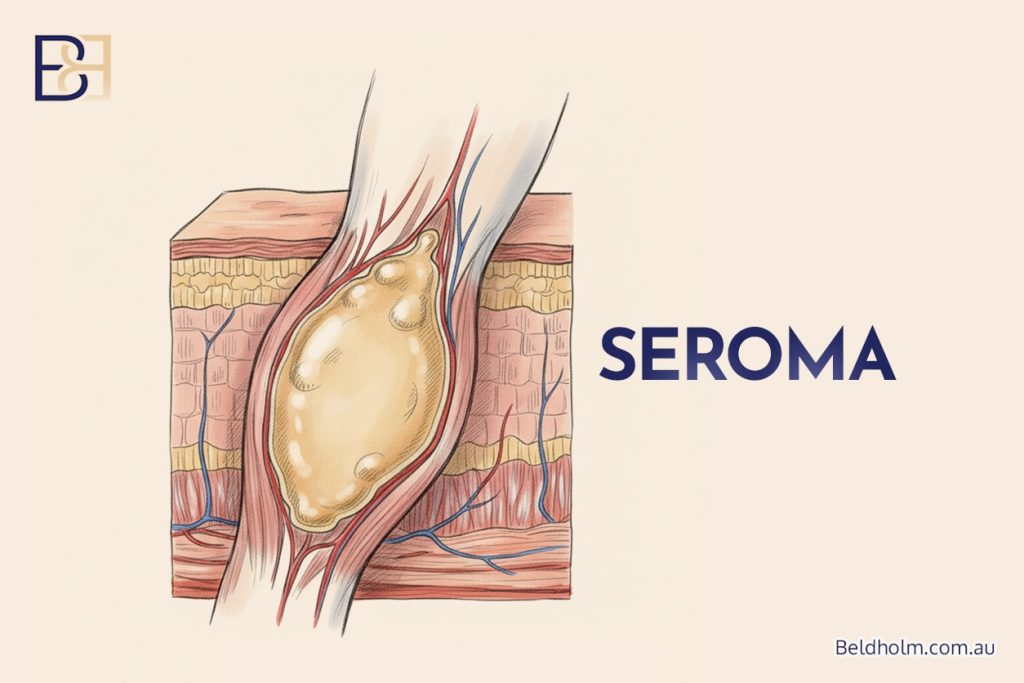
A seroma is an accumulation of clear fluid beneath the skin flap and is one of the most common postoperative Surgical complications (2,3).
Treatment Options:
- Small seromas: Managed conservatively with compression and drainage.
- Larger seromas: Treated through aspiration under sterile conditions in the clinic.
- Most resolve after 1–2 weeks of repeat aspiration and compression therapy.
- Persistent seromas may require ultrasound-guided aspiration or reinsertion of a drain.
Wound Healing Issues and T-Junction Dehiscence

Delayed wound healing is a recognised postoperative complication in Fleur-de-Lis abdominoplasty due to the tension at the T-junction where the vertical incision and horizontal incision meet (4,6).
Treatment Options:
- Small separations: Managed with local wound care and dressings.
- Delayed wound healing: Supported by LED light therapy and topical wound-healing agents.
- Non-healing or infected wounds: May require minor debridement or re-suturing.
Wound Infection
Wound infections occur in 2–6% of Fleur-de-Lis abdominoplasty cases (2,4,6).
Treatment Options:
- Superficial infections: Treated with oral antibiotics and wound cleaning.
- Deep infections or abscesses: Require hospital care, intravenous antibiotics, and sometimes surgical drainage.
- Preventive measures include perioperative antibiotics, sterile technique, and ongoing wound monitoring.
Bleeding and Postoperative Bleeding
Bleeding can occur intraoperatively or within 24–48 hours postoperatively (7). Post operative bleeding is a recognised risk that may require prompt intervention to prevent further complications.
Treatment Options:
- Minor bleeding: Managed with rest, compression, and observation.
- Significant bleeding: May require surgical exploration and haemostasis.
- Tranexamic acid (TXA): Reduces postoperative bleeding and drain output (7).
Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
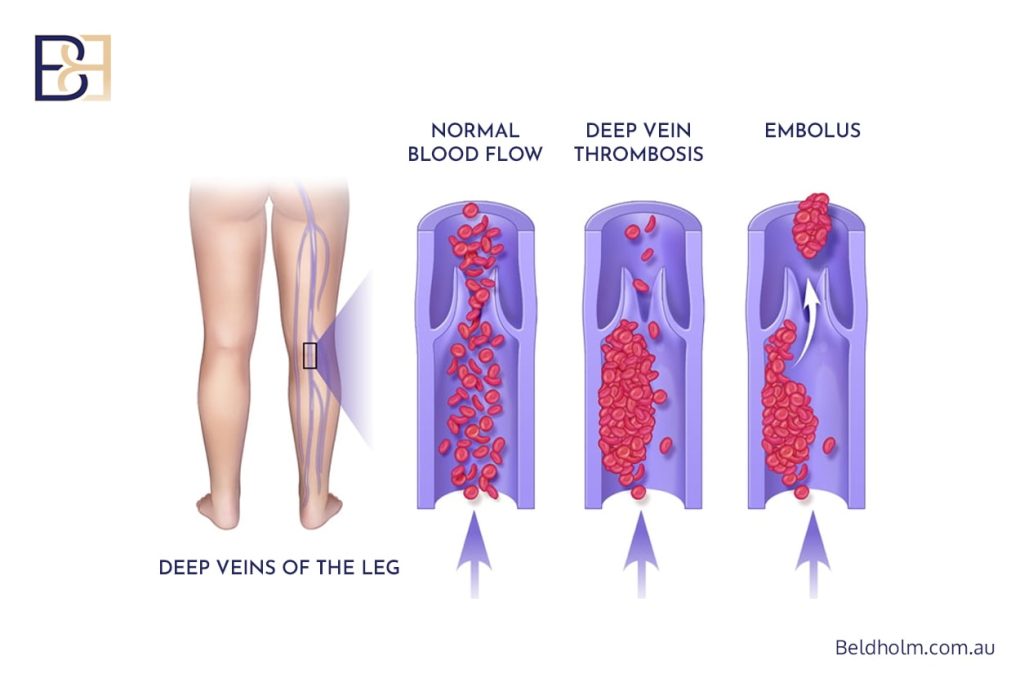
These are rare but serious complications (1,2).
Treatment Options:
- Prevention through early mobilisation, calf compression devices, and pharmacologic anticoagulation.
- Confirmed DVT or PE requires hospital admission and anticoagulant therapy.
Hypertrophic Scars and Skin Irregularities
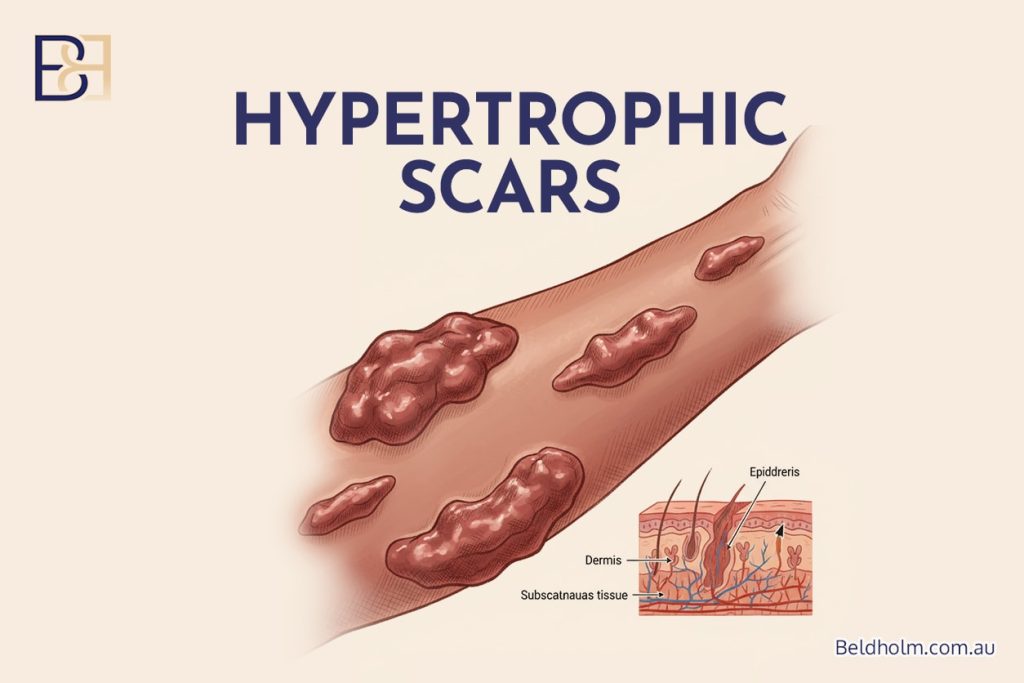
Due to incision length, hypertrophic or widened scars can occur (5).
Treatment Options:
- Silicone gel and scar massage.
- Laser therapy or microneedling for scar refinement.
- Revision abdominal surgery for persistent or bothersome scars.
Nerve-Related Complications
Nerve-related complications can occur after Fleur-de-Lis abdominoplasty due to the extensive dissection required in this surgical procedure. Patients may experience numbness, tingling, or nerve pain in the surgical area. These are usually temporary but can occasionally persist long-term.
Treatment Options:
- Numbness: Numbness in the abdominal or thigh area is common after abdominoplasty. This typically resolves over several months as nerves regenerate. In some patients, sensation changes can be long-term.
- Nerve Pain: Nerve pain may result from cut or stretched sensory nerves. It can present as shooting pains or burning sensations. Pain management strategies include oral medication, nerve desensitisation techniques, and time for nerve recovery.
- Cutaneous Nerve Damage: Damage to the cutaneous nerves supplying the upper thigh can cause numbness or hypersensitivity on the anterior thighs.
Liposuction (Suction-Assisted Lipectomy) Complications
When liposuction (suction-assisted lipectomy) is performed in conjunction with Fleur-de-Lis abdominoplasty, it introduces additional potential complications. These may affect both internal and superficial structures of the abdomen and surrounding regions.
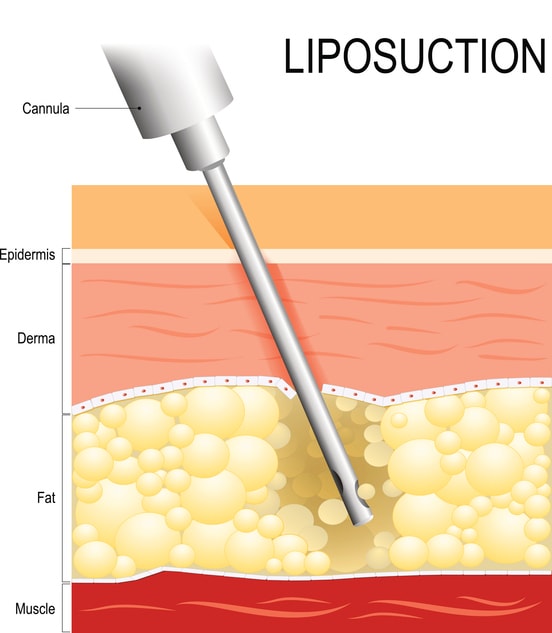
Common Complications and Management:
- Nerve and Structural Damage: The liposuction probe can inadvertently damage small nerves or internal structures in the abdominal wall. Controlled technique, limited depth, and proper cannula placement reduce this risk.
- Contour Irregularities and Skin Discolouration: Liposuction can cause minor grooves, contour irregularities, or temporary skin discolouration. These usually change over time with massage, lymphatic drainage, or, in rare cases, minor revision surgery.
- Fat Necrosis (Minor Complication): Fat necrosis is a minor complication that can occur after liposuction, especially in areas with significant fat deposits. It typically resolves on its own without intervention.
- Seroma and Haematoma Formation: Combining liposuction with abdominoplasty can increase fluid accumulation risk. Compression garments and drains are used to minimise this.
- Internal Injury: Although rare, aggressive liposuction can cause internal organ damage. Using small, blunt cannulas and remaining within the correct surgical plane minimises this risk.
Anaesthetic Complications
Anaesthetic complications can occur during or after any major surgical procedure, including Fleur-de-Lis abdominoplasty. These risks are minimised by performing surgery in an accredited hospital under the care of a specialist anaesthetist. However, patients should be aware of potential issues that can arise.
Possible Complications and Management:
- Nausea and Vomiting: These are the most common side effects after general anaesthesia and are usually managed with anti-nausea medication.
- Sore Throat or Hoarseness: Caused by the breathing tube used during anaesthesia; generally temporary and resolves within days.
- Allergic Reactions: Rare reactions to anaesthetic drugs can occur; anaesthetists are trained to recognise and manage these promptly.
- Respiratory Complications: Shortness of breath or temporary breathing difficulties can occur; oxygen and monitoring are provided postoperatively.
- Cardiovascular Events: Blood pressure fluctuations or cardiac issues are rare but are managed immediately by the anaesthetic team.
Patients are carefully assessed before surgery for medical suitability for anaesthesia, and risk reduction strategies are implemented throughout the procedure.
Risk Factors and Risk Factor Analysis
Understanding risk factors helps surgeons anticipate postoperative wound complications and optimise outcomes. Common risk factors include (2,3,4,6):
- High BMI: Increased wound tension and impaired perfusion lead to higher wound healing issues and delayed recovery process.
- Diabetes: Impaired microvascular circulation contributes to delayed wound healing.
- Smoking: Nicotine reduces oxygenation and increases wound complications.
- Nutritional Deficiencies: Common in bariatric surgery patients, deficiencies in protein, zinc, and vitamins A and C impair healing.
- Age and Resection body Weight: Older patients and those with large resected tissue have higher complication rates.
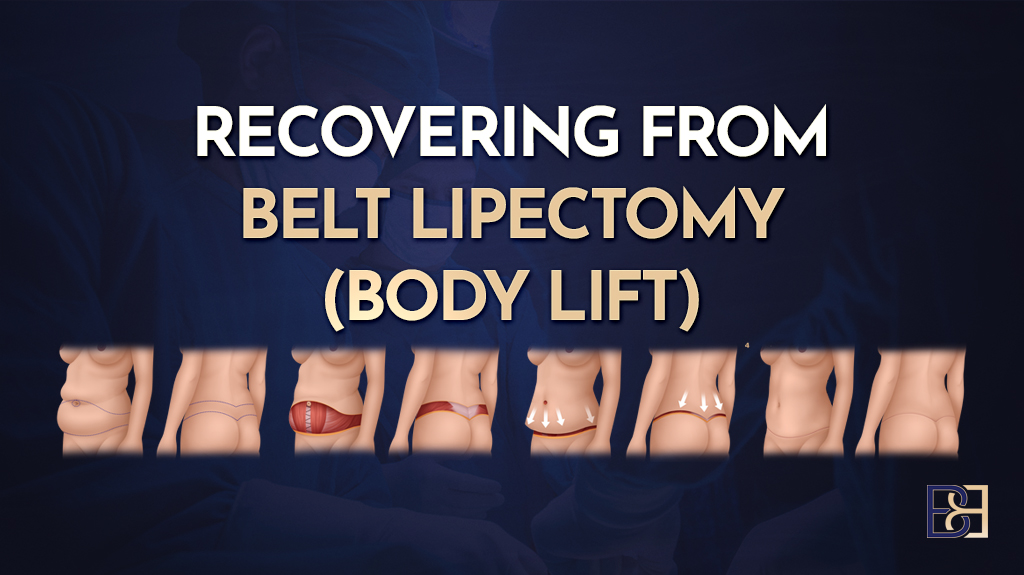
Minimising Risk and Supporting Healing
Dr Beldholm’s team focuses on preoperative optimisation, meticulous surgical technique, and structured postoperative care to support healing. Key strategies include (5,7):
- Preoperative Optimisation: Achieve stable weight, treat nutritional deficiencies, and correct any vitamin or iron deficiencies.
- Surgical Technique: Limited undermining, tension-reducing sutures, and use of advanced dressings such as Pico systems.
- Postoperative Care: LED light therapy, compression garments, and early wound checks help reduce delayed wound healing and postoperative complications.
Patients are encouraged to maintain realistic expectations and understand that recovery varies. While Fleur-de-Lis abdominoplasty carries possible risks, most patients recover (3,4).
Summary of Complication Data
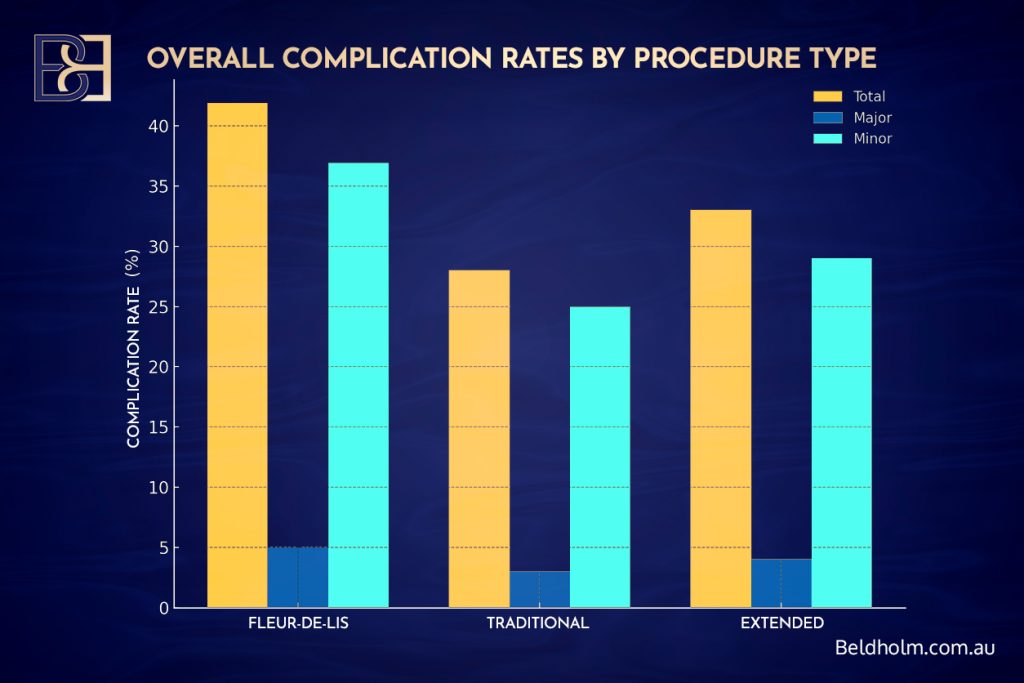
Complication | Fleur-de-Lis (%) | Traditional (%) | Extended (%) |
|---|---|---|---|
Total Complications | 41.9 | 28.0 | 33.0 |
Major Complications | 5.0 | 3.0 | 4.0 |
Wound Healing Problems | 32 | 18 | 25 |
Seroma | 9.5 | 7.0 | 8.0 |
Bleeding | 10.8 | 6.0 | 7.5 |
Deep Vein Thrombosis | 0.5 | 0.3 | 0.4 |
Conclusion by Dr Beldholm

Fleur-de-Lis abdominoplasty is an important reconstructive surgery option for post-bariatric patients and those with massive weight loss who present with significant skin laxity. Although the operation carries a relatively high complication rate compared to standard abdominoplasty, most complications are minor and managed effectively with early intervention. Preoperative optimisation, awareness of risk factors, and a tailored postoperative plan are critical to reducing postoperative complications and supporting healing (1,2,4,6).
References
- Parsa AA, McKnight CL, Macias LH, et al. Complications and Risks Associated With the Different Types of Abdominoplasties. Plast Reconstr Surg Glob Open. 2024;12(3):e5001–e5009.
- Sommer B, Westphal F, Strauss B, et al. Post-bariatric abdominoplasty: Analysis of 406 cases with focus on risk factors and complications. Aesthetic Surg J. 2021;41(5):NP450–NP462.
- Hester TR, Baird W, Nahai F, et al. Fleur-de-Lis abdominoplasty: A safe alternative to traditional abdominoplasty for the massive weight loss patient. Plast Reconstr Surg. 2010;125(1):45–55.
- Mistry RM, Tanna N, Morrison CM, et al. Fleur-de-Lys abdominal body contouring surgery following massive weight loss. J Plast Reconstr Aesthet Surg. 2021;74(3):613–620.
- Hurwitz DJ, Holland SW. The Fleur-de-Lis Abdominoplasty. Aesthetic Surg J. 2014;34(3):432–443.
- Saad A, Almutairi K, Shakir S, et al. Complications Following Abdominoplasty in Post-Weight Loss Patients: A Systematic Review and Meta-Analysis. J Plast Reconstr Aesthet Surg. 2025;78(1):11–22.
- Johnstone DJ, Parker ML, Zhen C, et al. Systemic Tranexamic Acid for Reduced Postoperative Blood Loss and Less Bleeding. Plast Reconstr Surg Glob Open. 2024;12(2):e4808–e4815.