Gynaecomastia surgery carries a 1-3% risk of complications. The most common complication is superficial wound infections, occurring in approximately 1.3% of patients. Serious complications, although rare, can include haematoma formation, deep vein thrombosis, and adverse reactions to anaesthesia.Dr. Beldholm will thoroughly discuss these complications as well as your expectations during your consultation.
Overview of Complications From Gynaecomastia Surgery
Reported complications from gynaecomastia surgery vary among studies. One of the largest studies on complication rates from gynaecomastia surgery involved a total of 204 pediatric and 1583 adult patients.
In this study comparing the surgical outcomes of minors and adults undergoing gynaecomastia procedures, researchers found a few key differences. Although children tended to have better overall health ratings (lower ASA scores), they were more likely to have wounds that were contaminated and to be admitted to the hospital for surgery. Most wounds in both groups were deemed “clean.” The rate of complications from surgery was low for both age groups, with minors experiencing slightly more surgical issues than adults. Interestingly, surgeries for children took about twice as long as those for adults. A history of gastrointestinal disease was linked to surgical complications, while prior cardiac issues and contaminated wounds were more likely to lead to medical complications. However, the results only show an association, not a direct cause-and-effect relationship. (Ref 1)
Overall complication rate in this study was 1.9% of adult patients
- Superficial wound complications was the most common complication at 1.3%
- Deep infections 0.2%
- Wound disruption (Dehiscence) 0.3%
- Overall medical complications 0.3%
- Sepsis (blood infection) 0.1%
- Bleeding requiring transfusion 0.1%
Complications of Gynaecomastia Surgery
Book your appointment online now
When considering gynaecomastia surgery, it’s important to be aware of potential complications of gynaecomastia. The overall complication rate for gynaecomastia surgery is reported at 1.9%, which means there are several risks to be aware of. Common complications include scarring & infections. The scars from your male breast reduction surgery can sometimes be abnormal, leading to an irregular body shape. Following your surgeon’s post-operative care instructions can minimise these risks.
In more severe cases, complications can lead to:
- The death of deep fatty tissues from impaired circulation, which can affect the overall chest shape and may necessitate more surgery to correct.
- Infections, although rare, can occur post-surgery and require close monitoring and treatment.
- Blood clots, while less common, are another potential issue that should be watched closely.
Other potential complications include skin shrinkage, which can lead to nipple retraction and irritation from sutures. Most issues, however, are minor, such as minor wound-related problems. Understanding these risks can help you make an informed decision and prepare for a smooth recovery.
Managing Scars After Surgery
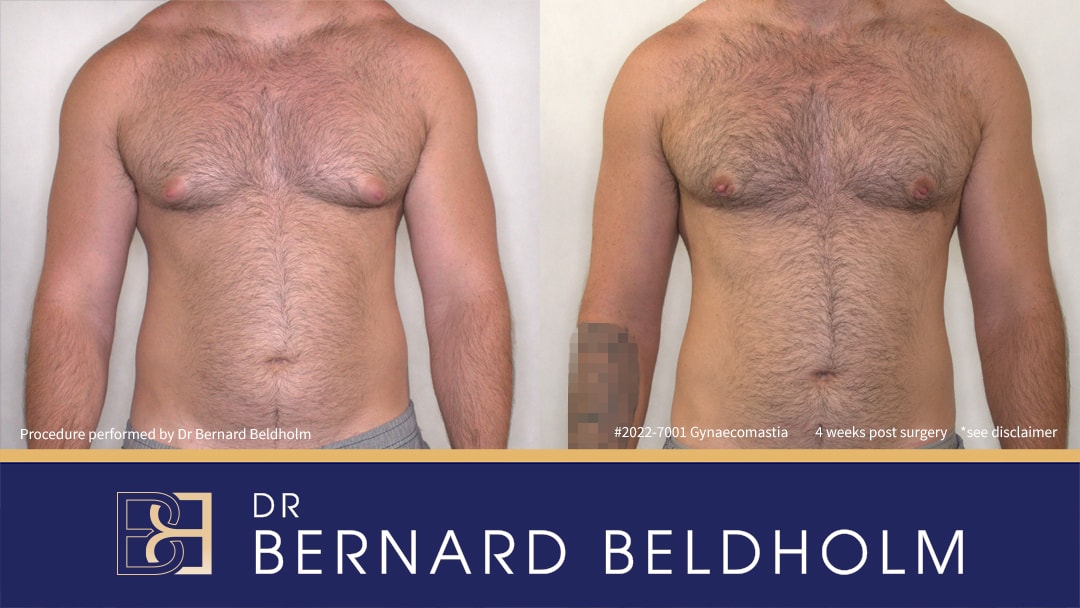
Tattoo blurred (on right forearm in after image) for privacy
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Scarring is a common concern among patients undergoing male breast reduction surgery. Scars typically start as pink but fade to become white, soft, and supple over time, though abnormal scarring can occur. Cosmetic problems, including excess skin, and unsightly scarring, including scar tissue, are common concerns reported by patients. Utilising silicone gel sheets can help the healing process by retaining moisture and regulating collagen production.
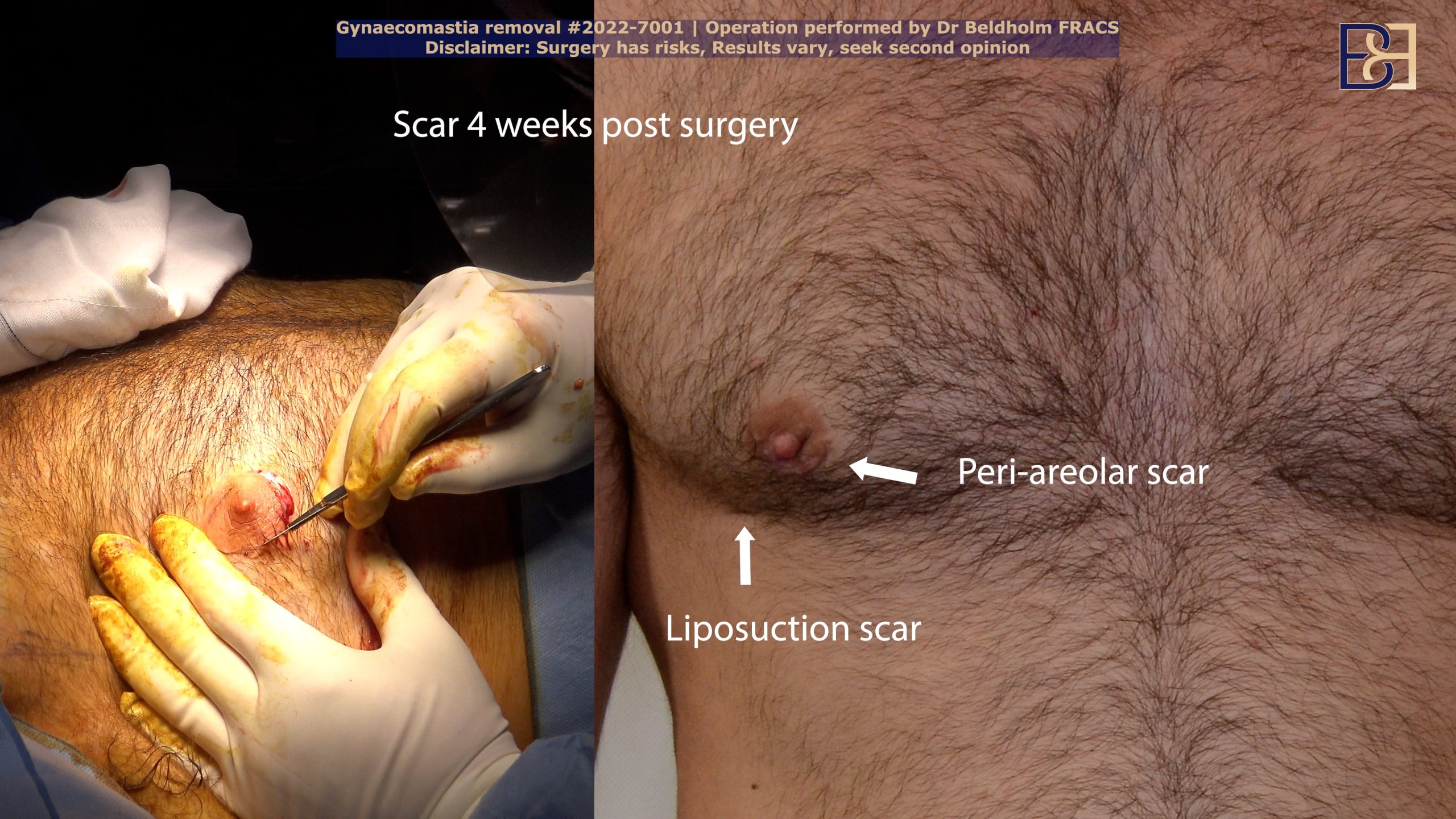
Massaging the scar area can also help prevent permanent skin irregularities after surgery. This technique can significantly reduce the appearance of scars over time. Your specialist surgeon may recommend specific products or techniques to aid in this process. Consistent care and attention to the surgical site can make a big difference in the final outcome.
Adhering to your surgeon’s post-operative care guidelines helps manage scars effectively. This may include avoiding direct sunlight on the scar, keeping the area clean, and using prescribed ointments. Proper care can help you achieve the best possible results from your male breast reduction surgery.
Infection Risks and Treatments
Although the risk of infection after gynaecomastia surgery is relatively low, it’s still a potential complication. One effective way to reduce infection risks is to remove body hair around the chest area before the surgical procedure. Signs of infection to watch out for include unusual swelling, redness, or discharge at the surgical site. Monitoring during follow-up appointments is crucial to ensure no unusual swelling has developed.
If an infection does occur, it can often be treated with oral antibiotics. In more severe cases, hospitalisation for intravenous antibiotics and drainage might be required. During the surgical treatment, a single dose of intra-operative intravenous antibiotics is administered to help prevent infections. This proactive approach significantly reduces the likelihood of post-surgical infections.
Stay vigilant during the healing process and report any signs of infection to your doctor promptly. Prompt treatment can prevent more severe complications and ensure a smoother recovery.
Blood Clots and Deep Vein Thrombosis
Serious complications like blood clots and deep vein thrombosis (DVT) can arise after gynaecomastia surgery. Venous thromboembolism is a life-threatening condition that underscores the importance of understanding these risks. Symptoms of DVT include swelling and pain in the calf or thigh, though some cases may present no symptoms at all, known as silent DVT.
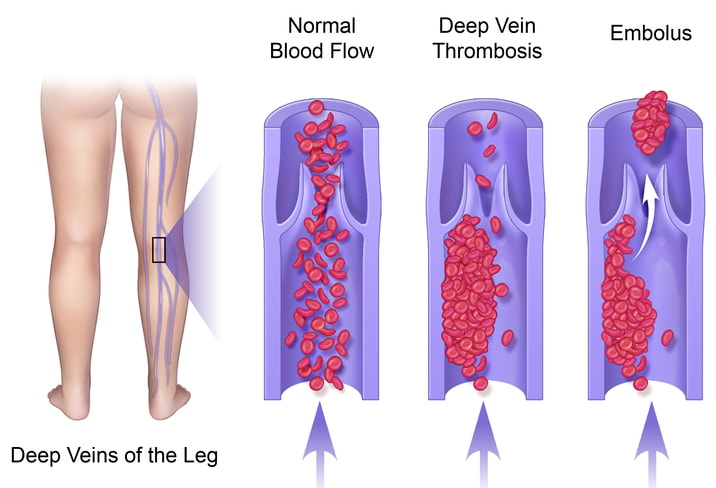
Immobility, such as long periods of sitting during travel or recovery from surgery, significantly increases the risk of developing DVT. Preventive measures include regular movement, staying hydrated, and the use of compression stockings, especially during long travels. These steps can help maintain proper circulation and reduce the risk of blood clots.
Awareness and proactive measures are key in preventing DVT. If you experience any symptoms of blood clots, contact your healthcare provider immediately for evaluation and treatment.
Seroma Formation as a Surgical Complication After Gynaecomastia Surgery
Seroma formation is a notable surgical complication that can arise after gynaecomastia surgery, affecting patient recovery and outcomes. A seroma is a collection of fluid that accumulates in the space where tissue has been removed or altered during surgery. This can lead to swelling, discomfort, and potential delays in the healing process.
Although seromas can occur in any surgical procedure involving tissue manipulation, they tend to present more frequently in surgeries involving significant dissection, such as gynaecomastia procedures. The incidence of seroma formation post-gynaecomastia surgery generally ranges from 2% to 5%.
To minimise the risk of seroma formation, surgeons often employ strategies such as meticulous dissection, meticulous hemostasis, and the application of compression garments postoperatively. If a seroma does occur, it may require drainage, and thorough follow-up is essential to monitor healing and avoid further complications.
Haematoma Formation as a Surgical Complication After Gynaecomastia Surgery

Haematoma formation is another significant complication that can occur following gynaecomastia surgery, potentially impacting patient recovery and outcomes. A haematoma is a localised collection of blood outside blood vessels, resulting from bleeding that may occur during or after the surgical procedure. This can lead to swelling, pain, and even infection.
The incidence of haematomas after gynaecomastia surgery can vary, but it is generally reported to occur in approximately 1% to 4% of cases. Several factors can contribute to the risk of haematoma formation, including the patient’s individual factors, such as coagulopathy or the use of anticoagulant medications, as well as surgical techniques employed during the procedure.
To reduce the likelihood of haematoma development, surgeons typically focus on achieving meticulous hemostasis during surgery and may advise patients to avoid certain medications that can increase bleeding risk. If a haematoma does develop, timely intervention, which may include surgical drainage or close monitoring, is essential to prevent complications and promote optimal healing. Educating patients on the signs of haematoma formation, such as significant swelling or increased pain, is crucial for early detection and management.
Allergic Reactions and Anaesthetic Complications

Allergic reactions are another potential complication of gynaecomastia surgery. These reactions can occur from various materials used during the procedure, such as tape, suture materials, and blood products. Anesthesia also carries risks, including allergic responses and possible severe cardiovascular events. General anaesthesia is used during the operation, which is why it’s crucial to discuss any known allergies with your surgeon beforehand.
Understanding these risks can help you prepare for surgery and ensure that any potential complications are averted.
Injury to Deeper Structures
Injury to deeper structures such as nerves, blood vessels, muscles, and even lungs can occur during gynaecomastia surgery. These injuries can lead to both temporary and permanent issues, including changes in nipple sensation, such as diminished sensitivity or hypersensitivity. The specific surgical technique employed can influence the likelihood of such injuries.
Factors like the surgeon’s experience and the complexity of the surgery play a crucial role in minimising these risks. Choosing a qualified and experienced surgeon significantly reduces the risk of deeper structure injuries.
Report any unusual sensations or pain to your doctor immediately after the surgery. Early intervention can help manage these complications effectively.
Reducing Surgical Risks

Reducing surgical risks starts long before the day of the operation. Patients should complete all pre-operative tests and physical exams as required. Avoiding herbal supplements and anti-inflammatory medications two weeks before surgery is crucial. Blood-thinning agents, including Aspirin and high-dose vitamin E, should also be stopped 10-14 days prior to surgery.
On the day of the surgery, it’s important not to eat or drink anything for six hours before the procedure to ensure proper anesthesia. Thorough preparation before surgery can significantly reduce risks and contribute to a smoother recovery process.
Post-Surgery Care and Recovery
Post-surgery care and recovery are critical for achieving the best results from your gynaecomastia surgery. Patients are required to wear a compression garment for 2 to 4 weeks after the operation to help reduce swelling and support the new chest shape. Pain management is crucial in the first few days post-surgery, with options ranging from over-the-counter medications to prescription pain relief. Cold compresses can also be beneficial for reducing pain and swelling but should not be applied directly to the skin.
Sleeping on your back and using pillows for support is recommended to facilitate recovery in the initial weeks. Surgeons may provide emergency contact information for patients to reach out if they experience any unusual symptoms after surgery.
Adhering to post-operative care instructions ensures a smooth recovery and optimal results from male breast reduction surgery.
Emotional and Psychological Impact
The psychological burden of gynaecomastia can be significant, affecting overall mental health (Ref 2). Research indicates that many patients report feeling less isolated and embarrassed after undergoing surgery for gynaecomastia. Post-surgical assessments show notable differences in various psychological aspects, including emotional well-being and social functioning.
Young patients, in particular, tend to experience a more significant increase in anxiety following gynaecomastia surgery compared to older individuals. However, the overall quality of evidence regarding the psychological impact of gynaecomastia surgery is considered low, necessitating further research.
Focusing on the emotional and psychological aspects of gynaecomastia and seeking support when needed is important.
Long-term follow-up and monitoring are critical components of the recovery process. The typical recovery period after gynaecomastia surgery spans approximately 4 to 6 weeks. Dr. Beldholm’s usual follow-up schedule includes appointments at one month, 3, 6, and 12 months to ensure proper healing.
Dr Beldholm final thoughts

In summary, understanding the potential complications and how to manage them can help you navigate your gynaecomastia surgery journey more smoothly. From managing scars and preventing infections to minimising surgical risks and emotional impact, each aspect is crucial for a successful outcome.
Remember, the journey to a flatter chest is a marathon, not a sprint. Take it one step at a time and consult with your medical team whenever needed.
Frequently Asked Questions
What type of anaesthetic is used during gynaecomastia removal surgery?
During gynaecomastia removal surgery, a general anaesthetic is used. It ensures you’re completely unconscious and pain-free during the procedure.
What are the common risks associated with gynaecomastia removal surgery?
Gynaecomastia removal surgery can come with risks like scarring, infection, and complications like blood clots or heart issues. It’s important to weigh these risks against the benefits before going under the knife.
What happens to scars after gynaecomastia surgery?
Scars from gynaecomastia surgery usually begin as pink but gradually fade to white and become softer. Just keep an eye out for any unusual scarring.
What complications can arise from infections after surgery?
Infections after surgery can lead to complications like prolonged recovery, the need for IV antibiotics, or even hospitalisation for drainage. It’s important to keep an eye out for signs of infection to avoid these issues.
References
- Zavlin D, et al. “Complications and Outcomes After Gynecomastia Surgery: Analysis of 204 Pediatric and 1583 Adult Cases from a National Multi-center Database.” Aesthetic Plastic Surgery. 41(4):761-767, 2017 Aug.
- Nuzzi LC et al. “Psychosocial impact of adolescent gynecomastia: a prospective case-control study.”, Plastic & Reconstructive Surgery. 131(4):890-896, 2013 Apr.