Gynaecomastia, the enlargement of male breast tissue, involves specific histological changes that can provide important clues for diagnosis and treatment. Understanding the histology of gynaecomastia—specifically the alterations in ductal and stromal tissues—can shed light on its development and progression. This article will delve into the normal histology of the male breast, the stages of gynaecomastia, and the histological traits distinctive to each phase, offering valuable insights into this condition.
Key Takeaways
- Understanding normal male breast histology is essential for recognizing changes in gynaecomastia, which differs significantly from female breast structure.
- Gynaecomastia evolves through stages: florid, intermediate, and fibrous, each with distinct histological characteristics crucial for diagnosis and management.
- Hormonal imbalances, particularly shifts in oestrogen and testosterone levels, play a key role in the development of gynaecomastia, necessitating careful evaluation and treatment strategies.
Normal Histology of the Male Breast
Book your appointment online now
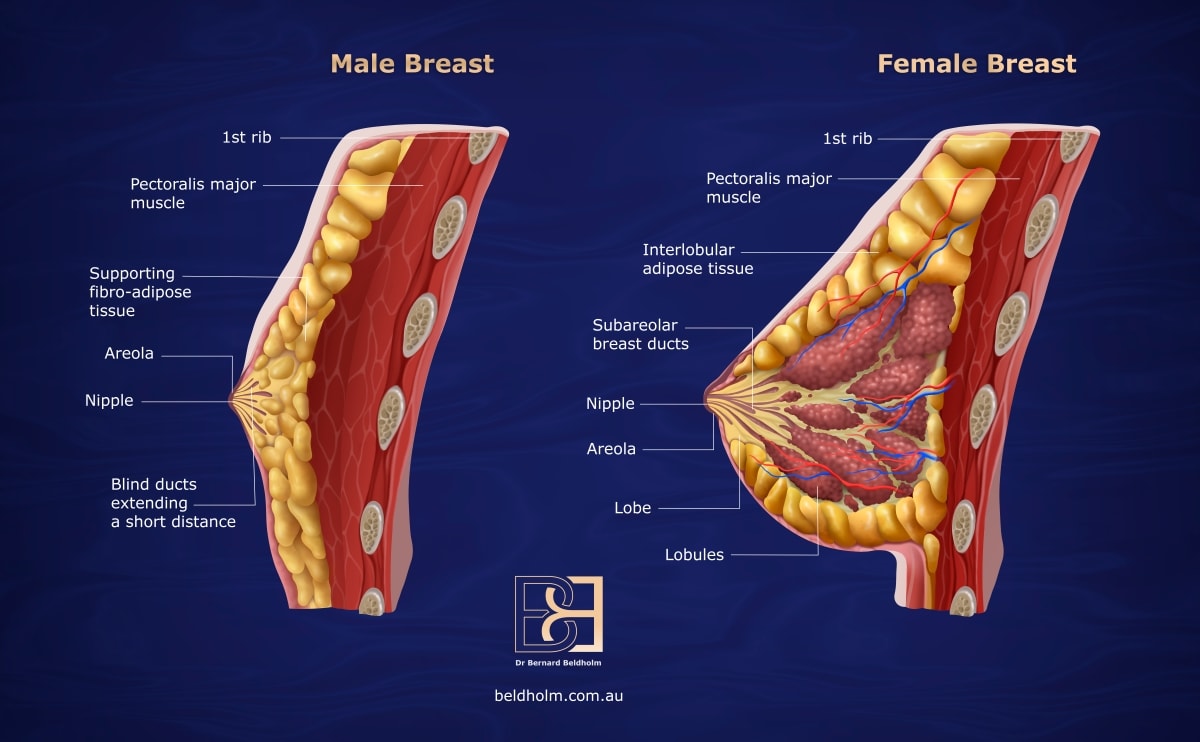
Understanding gynaecomastia begins with knowing the normal histology of the male breast. Unlike the female breast, which is highly complex and structured for functions such as lactation, the male breast remains rudimentary throughout life. It primarily consists of a basic ductal system, and stroma made up of collagen and fat, lacking the lobule structures that are present in females.
The male breast anatomy typically features fatty tissue with limited ducts and stroma, contrasting sharply with the more intricate architecture found in the female breast.
Appreciating the changes associated with gynaecomastia involves understanding the specifics of the ductal structures and stromal components in the male breast.
Ductal Structures
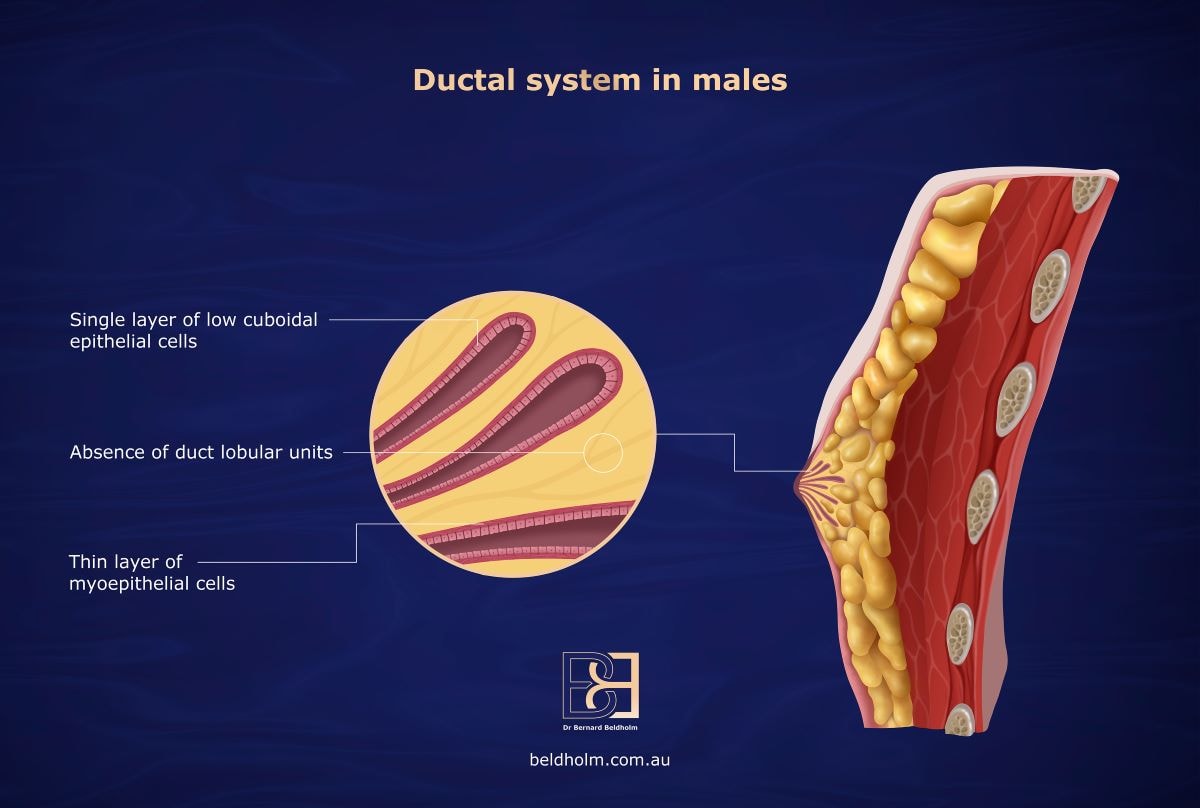
The male breast contains a rudimentary ductal system lined by a single layer of low cuboidal epithelial cells, supported by a thin layer of myoepithelial cells. This simple structure is sufficient for the minimal functional demands of the male breast and reflects its limited differentiation. Unlike the female breast, which undergoes extensive development to form terminal duct lobular units (TDLUs) essential for milk production, the male breast never progresses beyond this basic architecture. The absence of lobular structures highlights the stark contrast between the uncomplicated ductal system in men and the complex mammary gland development seen in women.
Stromal Components
The male breast stroma is primarily fibrous and adipose tissue, providing structural support for the rudimentary ductal system. Unlike female breasts, the male breast lacks Cooper’s ligaments. This difference in composition is essential in understanding gynaecomastia development.
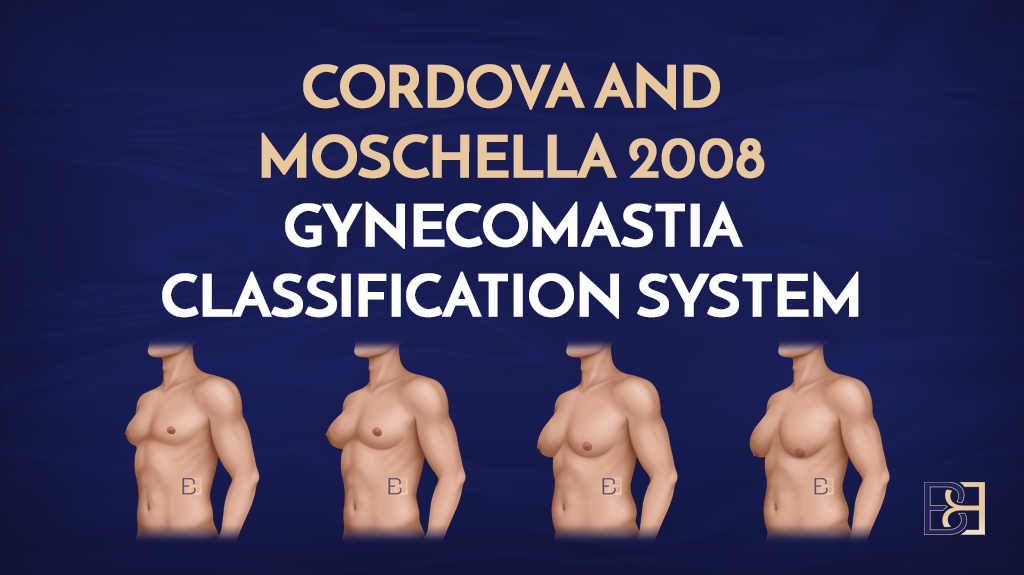
Physiological Evolution of Gynaecomastia
Gynaecomastia evolves through distinct physiological stages, each with unique histological characteristics. This progression can be broadly categorised into florid, intermediate, and fibrous phases. Recognising these stages is crucial for the effective diagnosis and treatment of gynaecomastia.
The initial florid stage is marked by a proliferation of ductal and stromal tissues. In contrast, the intermediate stage represents a transition period where characteristics of both florid and fibrous phases are present. Finally, the fibrous stage is characterised by significant fibrosis and reduced cellular activity.
Florid Gynaecomastia
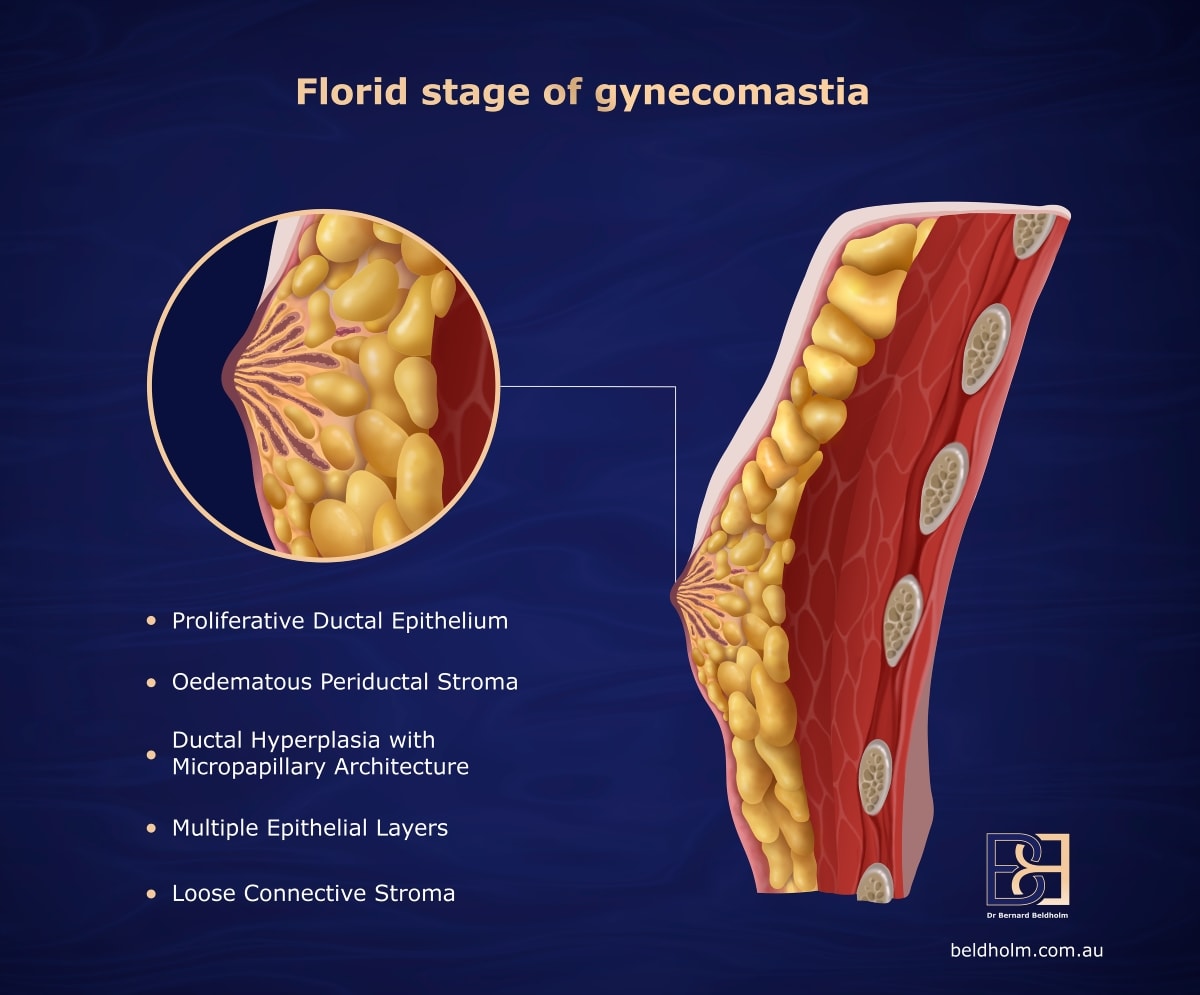
Florid gynaecomastia is typically observed in cases of recent onset, usually less than four months. This stage is characterised by a proliferative ductal epithelium with clustering ducts embedded in a variably cellular stroma containing fibroblasts and adipose tissue. Periductal stroma may also be oedematous, contributing to the breast enlargement associated with gynaecomastia.
During this early stage, the epithelial proliferation often exhibits usual ductal hyperplasia, sometimes with a micropapillary architecture. This growth phase underscores the dynamic changes occurring in the breast tissue.
Intermediate Gynaecomastia
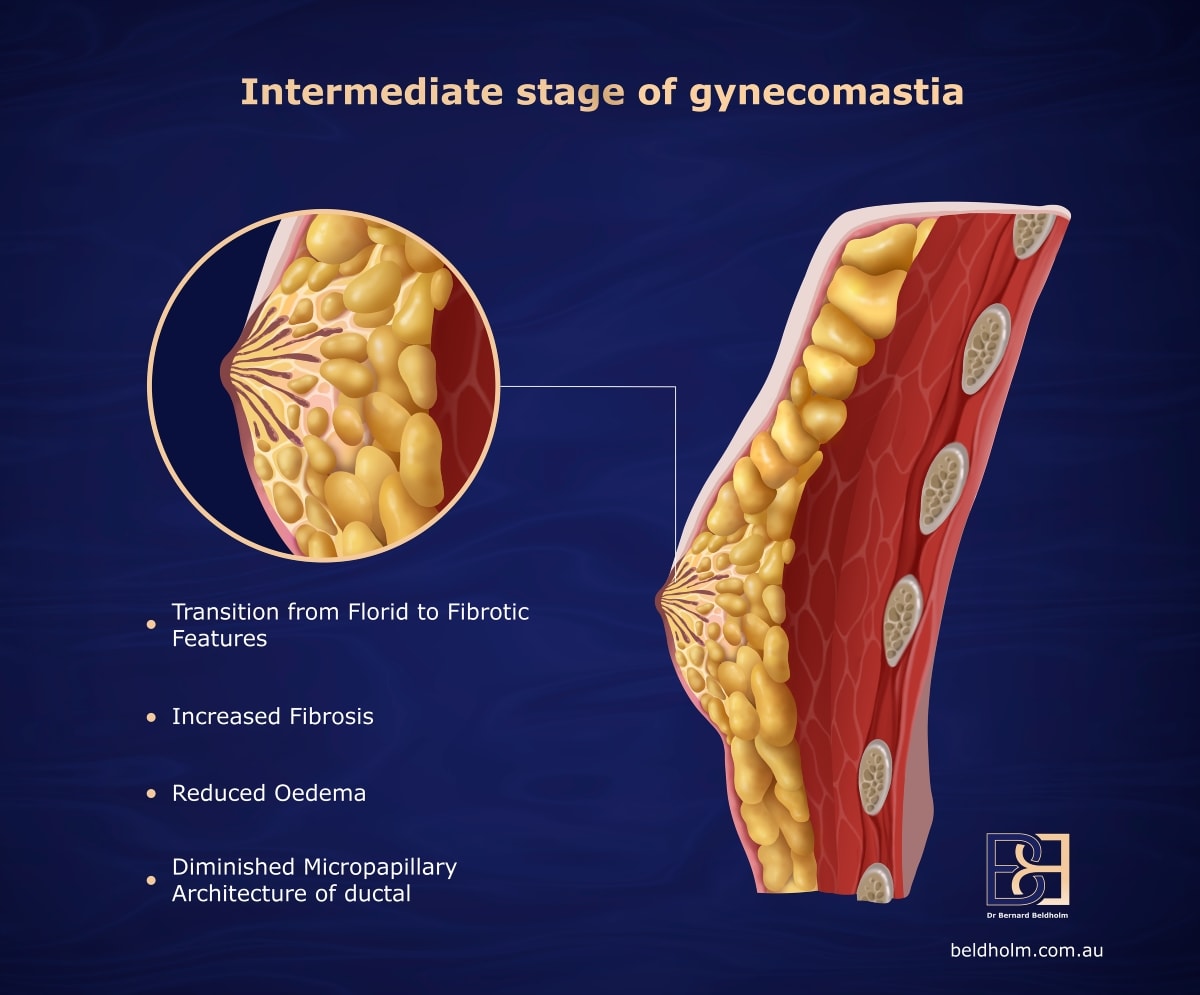
Intermediate gynaecomastia represents a transitional phase between the florid and fibrous stages. This period typically spans from four to twelve months after the initial onset of gynaecomastia. Histologically, it shows features of both the proliferative activity seen in florid gynaecomastia and the fibrosis characteristic of the later fibrous phase.
This stage is marked by a gradual decrease in cellular proliferation and an increase in stromal fibrosis, indicating the body’s attempt to stabilise the condition. This transition is crucial for understanding how long-term gynaecomastia develops and progresses.
Fibrous Gynaecomastia
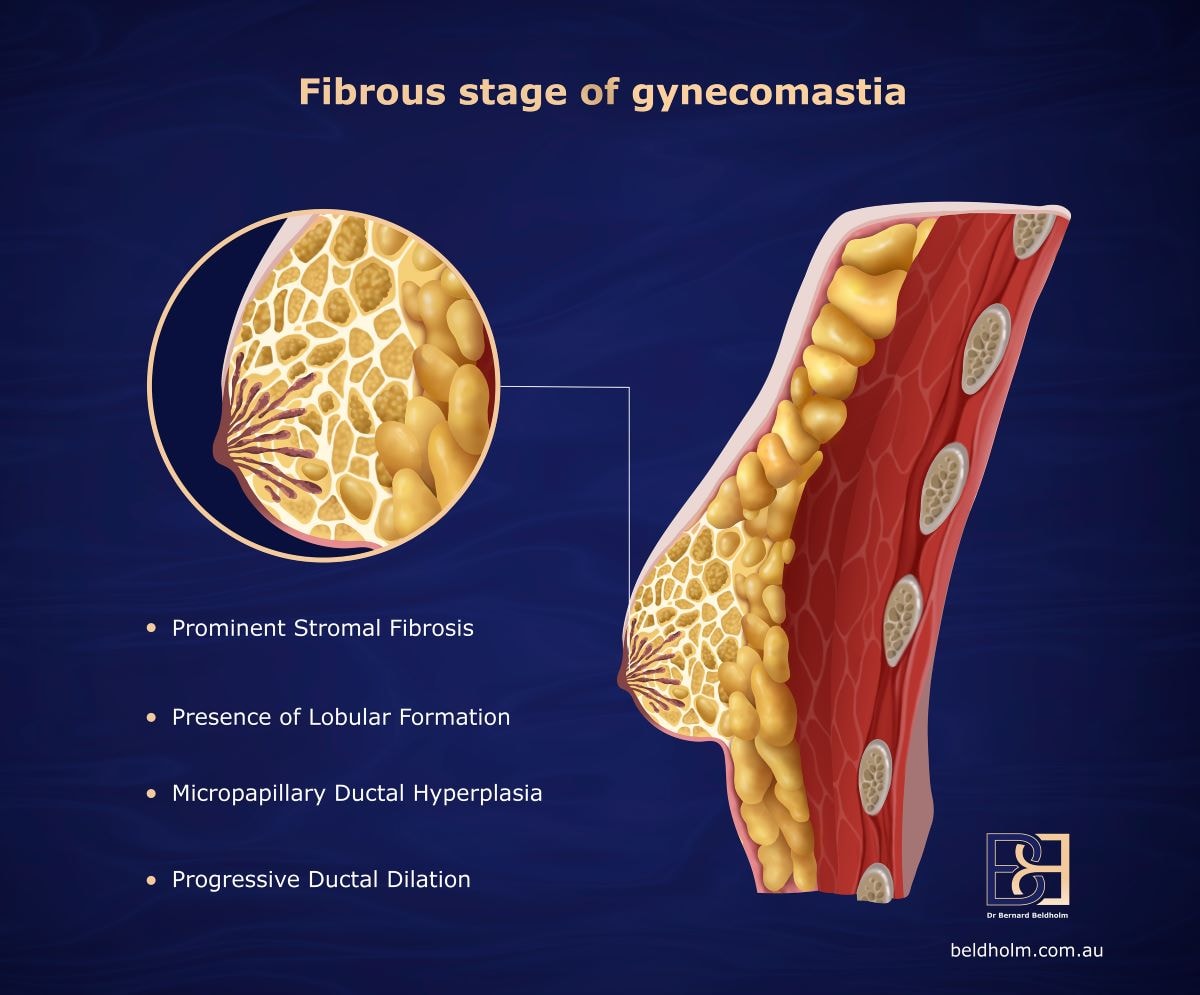
The fibrous phase of gynaecomastia generally occurs after prolonged proliferative activity, typically lasting more than a year. During this stage, epithelial proliferation decreases, and progressive ductal dilatation is observed. The stroma becomes more fibrotic, with reduced adipose tissue and vanishing periductal oedema.
Other histological findings during this phase may include pseudoangiomatous stromal hyperplasia, lobular formation, and various forms of metaplasia. This phase signifies the chronic nature of gynaecomastia and highlights the long-term changes in breast tissue.
Pathophysiology of Gynaecomastia
The pathophysiology of gynaecomastia is complex, driven by hormonal imbalances and tissue proliferation. Fundamentally, it arises from fluctuating levels of oestrogen and testosterone, which can be influenced by factors like hormonal therapy, obesity, and certain medications, including idiopathic gynaecomastia.
Comprehending hormonal dynamics is key to understanding gynaecomastia development. Two crucial factors are the oestrogen to androgen ratio and pubertal hormonal changes.
Oestrogen to Androgen Ratio

A key factor in the development of gynaecomastia is the shift in the oestrogen to androgen ratio. When oestrogen levels increase relative to androgens, it stimulates the proliferation of glandular breast tissue. This hormonal shift can occur due to various reasons, including the conversion of anabolic steroids to oestrogen in the body.
Testosterone typically counteracts the effects of oestrogen, but when this balance is disrupted, it can lead to increased breast tissue growth in men. This hormonal environment is crucial for understanding the underlying causes of gynaecomastia.
Hormonal Changes During Puberty
During puberty, boys experience significant hormonal changes, with testosterone levels increasing up to 30 times and oestrogen levels rising by three times. Despite these changes, boys with pubertal gynaecomastia often have lower free testosterone levels compared to their peers without the condition, which may affect their oestrogen to testosterone ratio.
These hormonal shifts can lead to the development of gynaecomastia, as the increased oestrogen levels promote the proliferation of glandular tissue. Recognising these changes is crucial for diagnosing and managing gynaecomastia in adolescents.
Imaging Patterns in Gynaecomastia
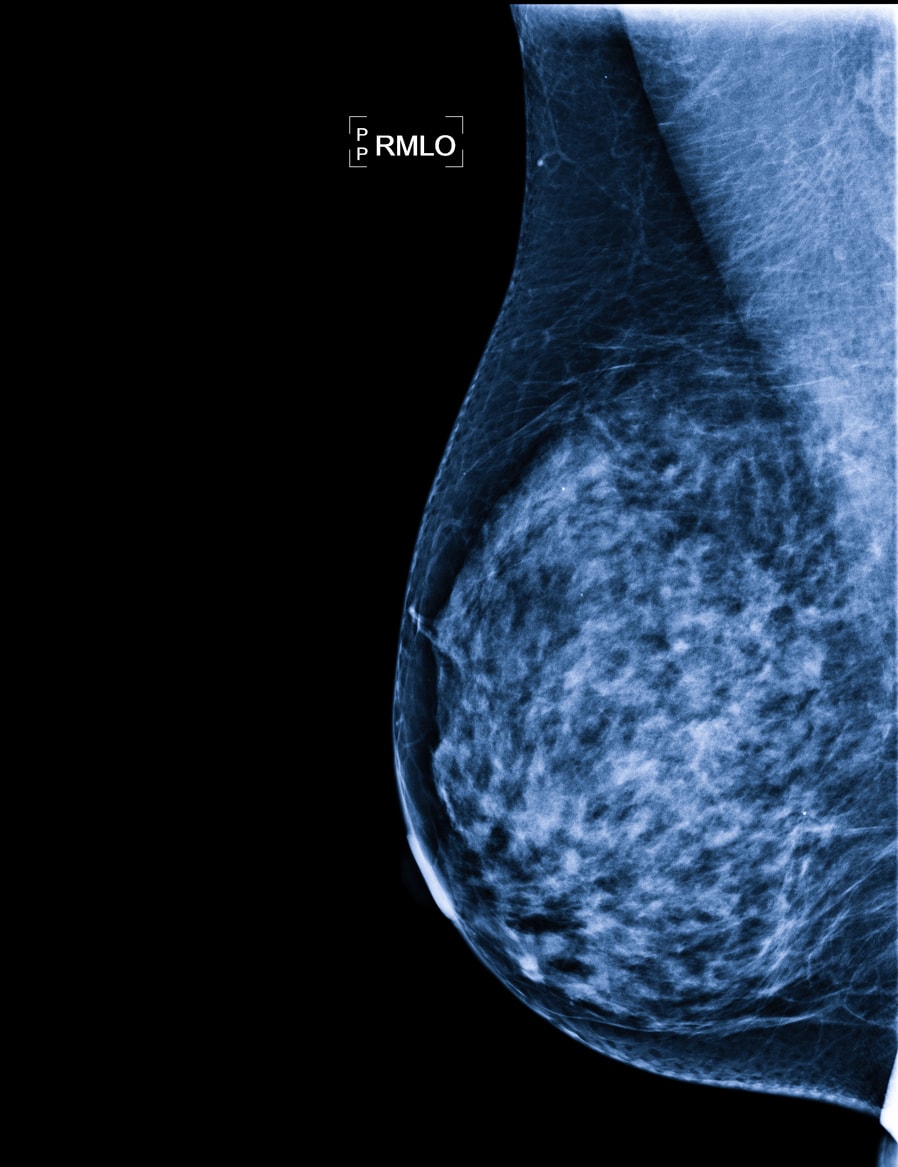
Imaging plays a crucial role in diagnosing and evaluating gynaecomastia. Various imaging techniques, such as mammography and ultrasound, reveal distinct patterns associated with the condition. These patterns include nodular, dendritic, and diffuse glandular formations, each providing unique insights into the tissue changes.
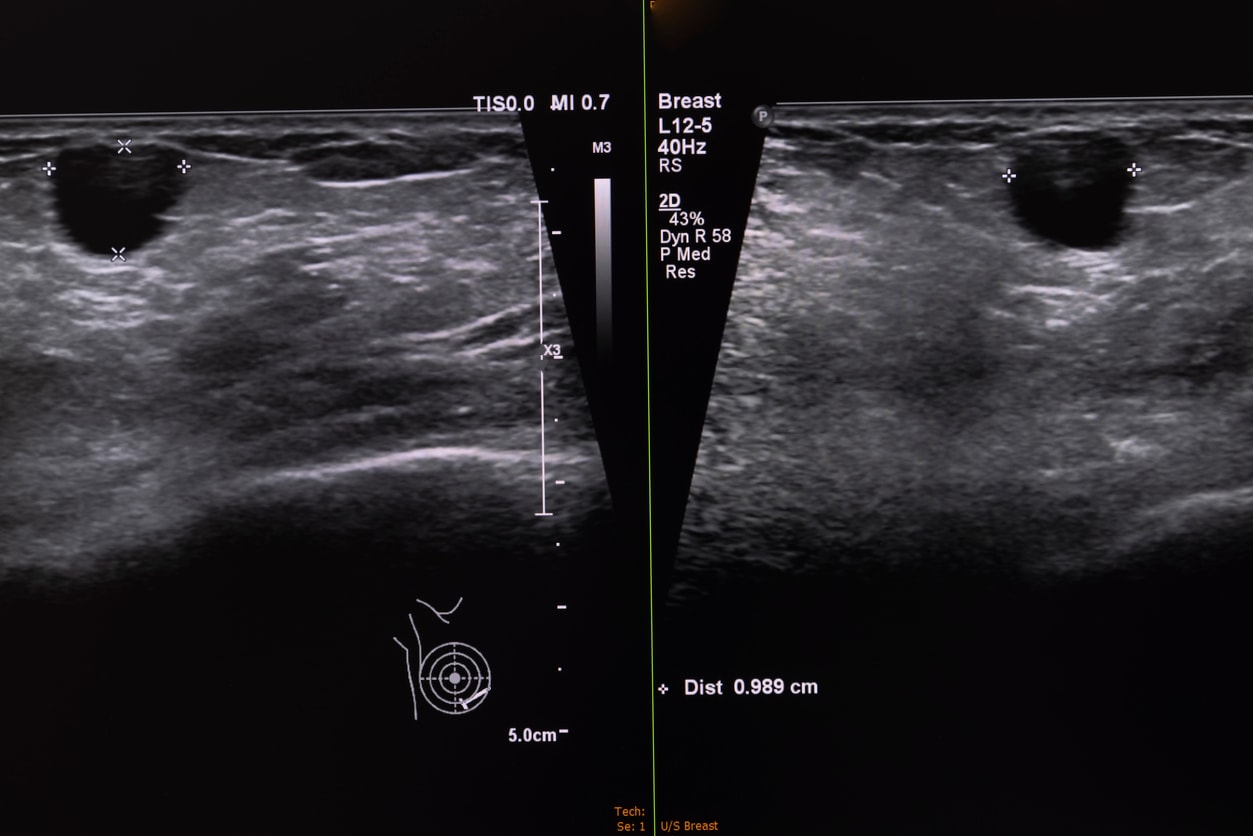
Radiological findings help differentiate gynaecomastia from other breast conditions, offering valuable information for accurate diagnosis and management.
Nodular Pattern
The nodular pattern of gynaecomastia is typically observed during the early stages. This pattern is characterised by intraductal epithelial hyperplasia, loose cellular stroma, periductal inflammation, and oedema. On mammography, nodular gynaecomastia appears as a retroareolar, fan-shaped density.
Dendritic Pattern
The dendritic pattern is characterised by a branching, tree-like appearance extending from the nipple. This radiological feature is typically seen during the intermediate stages of gynaecomastia, reflecting the complex tissue changes.
Diffuse Glandular Pattern
The diffuse glandular pattern is typically observed in advanced cases of gynaecomastia. This pattern is characterised by diffuse, dense nodular parenchyma within an enlarged breast, closely resembling female breast tissue. This extensive glandular proliferation highlights the significant histological changes occurring in chronic gynaecomastia.
Gynaecomastia in Bodybuilders
Bodybuilders often face unique challenges with gynaecomastia due to their use of anabolic steroids. The visibility of breast tissue enlargement in a sport where low body fat is essential makes gynaecomastia a significant concern.
Recognising the impact of anabolic steroids and the typical histological findings in bodybuilders is vital for managing this condition.
Impact of Anabolic Steroids
Anabolic steroids can significantly alter the balance of oestrogen and testosterone in the body, leading to increased development of glandular breast tissue and oestrogen receptors and androgen receptors. These steroids are often converted to oestrogen, disrupting the natural testosterone-to-oestrogen ratio and fostering the proliferation of breast tissue.
The hormonal imbalance caused by steroid use underscores the importance of monitoring and managing steroid intake to prevent gynaecomastia in bodybuilders.
Typical Histological Findings
Histologically, bodybuilders with gynaecomastia typically show pronounced glandular tissue with minimal adipose tissue, indicating a more pronounced breast tissue development. This configuration is characterised by minimal fatty cushioning between the gland and surrounding fascia, highlighting the significant glandular proliferation.
Differential Diagnosis
Differentiating gynaecomastia from other conditions is critical for accurate diagnosis and treatment. The differential diagnosis includes considerations of hormonal imbalances and distinguishing gynaecomastia from conditions like pseudo-gynaecomastia and male breast cancer.
Recognising these distinctions aids in providing appropriate care and lessens the psychological distress often associated with gynaecomastia.
Pseudo-gynaecomastia
Pseudo-gynaecomastia is characterised by the proliferation of adipose tissue without the presence of epithelial cells, making it distinct from true gynaecomastia. This condition is common in obese men and can present as unilateral breast enlargement.
Unlike gynaecomastia, which involves glandular proliferation due to hormonal changes, pseudo-gynaecomastia results from adipose tissue hypertrophy.
Male Breast Cancer
Although gynaecomastia and breast pain are generally benign, it is crucial to distinguish these conditions from male breast cancer. Clinical signs that may suggest breast cancer include unilateral, firm, and tender masses located away from the nipple-areolar complex, often accompanied by discharge. Primary breast cancers found in men, such as intracystic papillary carcinomas, resemble those that occur in women. It is also important to consider tumours that have metastasised to the male breast, including those from lung cancer, prostate cancer, and lymphoma.
Male breast cancer, while rare, is a significant health concern that warrants greater awareness and understanding. This cancer arises when malignant cells develop in the breast tissue and may manifest through symptoms like lumps, alterations in breast shape or size, and skin dimpling. Key risk factors include genetic mutations (such as BRCA2), a family history of breast cancer, exposure to radiation, and certain hormonal imbalances. Early detection is vital, as it can be accomplished through self-exams and regular health screenings. Treatment options vary based on the cancer’s stage and characteristics and may include surgery, radiation therapy, hormone therapy, and chemotherapy. Raising awareness and advancing research are essential to educate both men and healthcare providers about this condition, helping to dispel the stigma often associated with breast cancer.
Clinical Management and Prognosis

Gynaecomastia is a benign condition with a generally favourable prognosis. The first step in management involves a thorough history and physical examination to rule out potential systemic diseases. Treatment options include pharmacological and surgical interventions to develop gynaaecomastia, depending on the severity and duration of the condition.
Monitoring and reassurance, pharmacological treatments, and surgical interventions are key components of managing gynaecomastia effectively.
Monitoring and Reassurance
Most cases of gynaecomastia are benign and self-limited, requiring only regular follow-ups to monitor the condition. Reassuring patients that gynaecomastia is generally not indicative of serious underlying health issues is essential.
Regular monitoring helps in early detection of any changes that might require further intervention, providing peace of mind to the patients.
Pharmacological Treatments
Pharmacological treatments are often the first line of intervention for gynaecomastia. Medications like tamoxifen and raloxifene, which are selective oestrogen receptor modulators (SERMs), can reduce breast size and manage hormonal imbalances. Tamoxifen is especially effective during the acute phase of gynaecomastia, although it may not completely resolve associated breast pain.
These treatments are recommended for both idiopathic and treatment of pubertal gynaecomastia.
Surgical Interventions
Surgical treatment, such as subcutaneous mastectomy, is considered the most effective intervention for persistent gynaecomastia. Surgery is often the treatment of choice for extensive cases, providing immediate and noticeable results.
Summary
In summary, gynaecomastia is a condition characterised by the benign proliferation of both ductal and stromal tissues in the male breast, primarily driven by hormonal imbalances. Understanding the normal histology of the male breast, the physiological evolution of gynaecomastia, and its histological features are crucial for accurate diagnosis and treatment.
Imaging patterns play a vital role in differentiating gynaecomastia from other conditions, while the impact of anabolic steroids on bodybuilders highlights the need for targeted interventions. Differential diagnosis, including distinguishing pseudogynaecomastia and male breast cancer, is essential for appropriate care.
Effective management of gynaecomastia involves a combination of monitoring, pharmacological treatments, and surgical interventions. By understanding the intricacies of this condition, individuals can make informed decisions about their health and treatment options, paving the way for better outcomes.
Book your appointment online now
Frequently Asked Questions
What are the primary causes of gynaecomastia?
Gynaecomastia mainly stems from a hormonal imbalance between estrogen and testosterone. Stuff like obesity, certain meds, and anabolic steroids can also play a role in causing this condition.
How can gynaecomastia be distinguished from male breast cancer?
You can distinguish gynaecomastia from male breast cancer by noting that gynaecomastia is usually just a benign enlargement of breast tissue, while male breast cancer often shows up as a hard, painful lump that’s typically one-sided and not near the nipple. If you notice any unusual changes, it’s always good to check with a doctor.
What are the common imaging patterns observed in gynaecomastia?
Gynaecomastia usually shows up as nodular, dendritic, or diffuse glandular patterns on imaging. Recognising these can really help in figuring out what’s going on and distinguishing it from other issues.
Can gynaecomastia resolve on its own?
Yes, gynaecomastia can often sort itself out, especially in teens going through puberty. Just keep an eye on it, and usually, there’s no need for major interventions.
What are the treatment options for gynaecomastia?
You can tackle gynaecomastia with medications like tamoxifen or raloxifene, or if needed, surgical options like subcutaneous mastectomy. The best choice really depends on how severe and long-lasting your condition is.