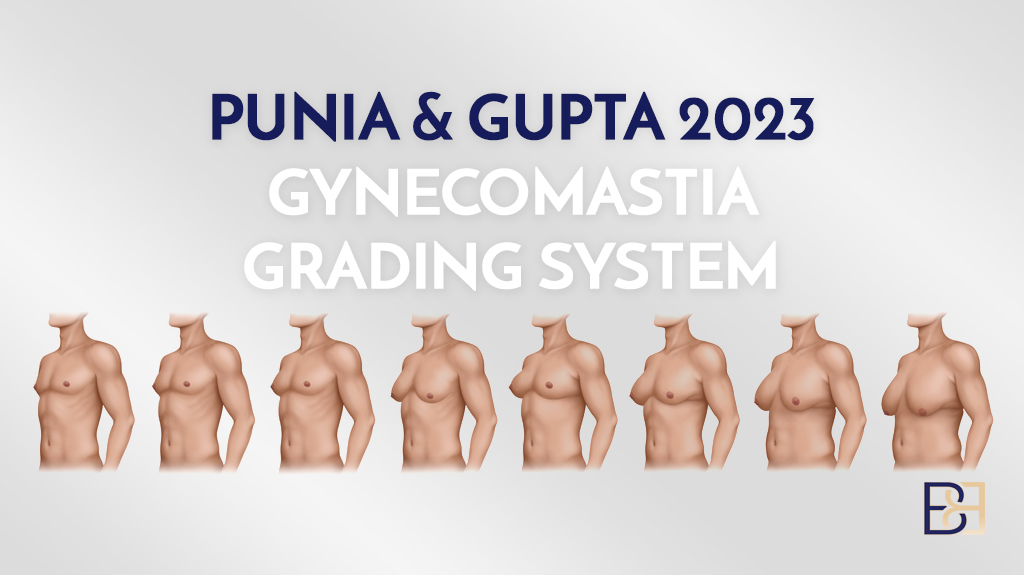
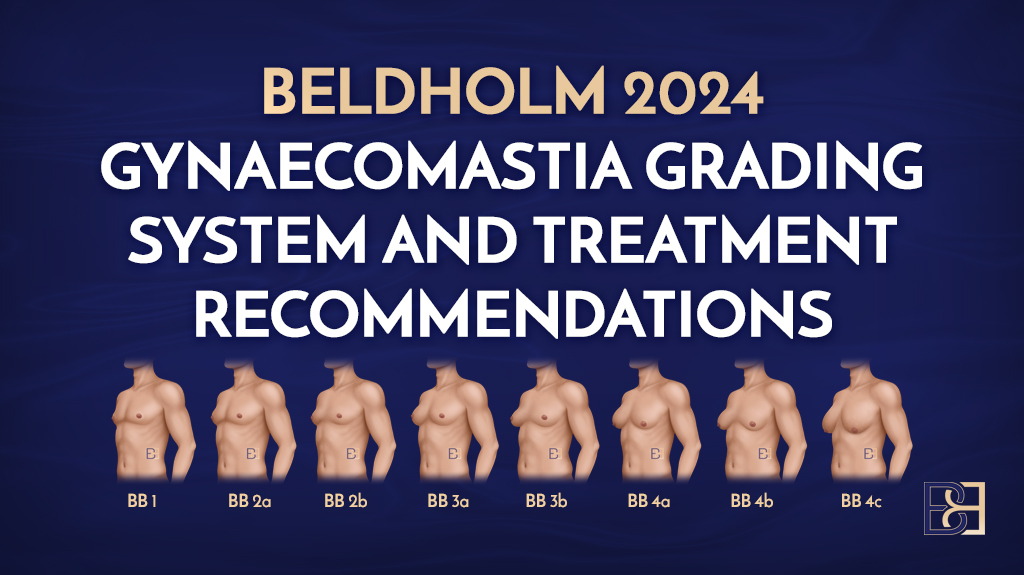
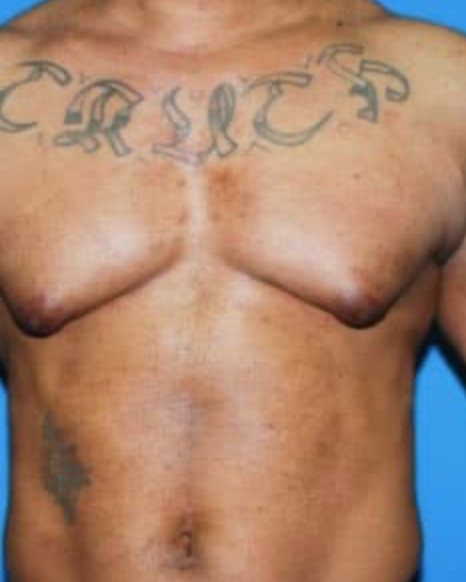
The Cohen classification system is a framework for categorising the severity and presentation of gynaecomastia, a condition characterised by the enlargement of male breast tissue. Developed by J.C. Cohen in 1987, this system built upon earlier models, offering recommendations for planning the most appropriate gynaecomastia treatment.
By classifying gynaecomastia into four distinct groups, the authors of the Cohen system sought to provide a structured approach to aid clinicians in diagnosing the condition and tailoring treatment plans for gynaecomastia based on the extent of tissue growth, skin excess, and chest contour.
By using a standardised methodology, Cohen attempts to standardise communication among providers, ensure consistency.
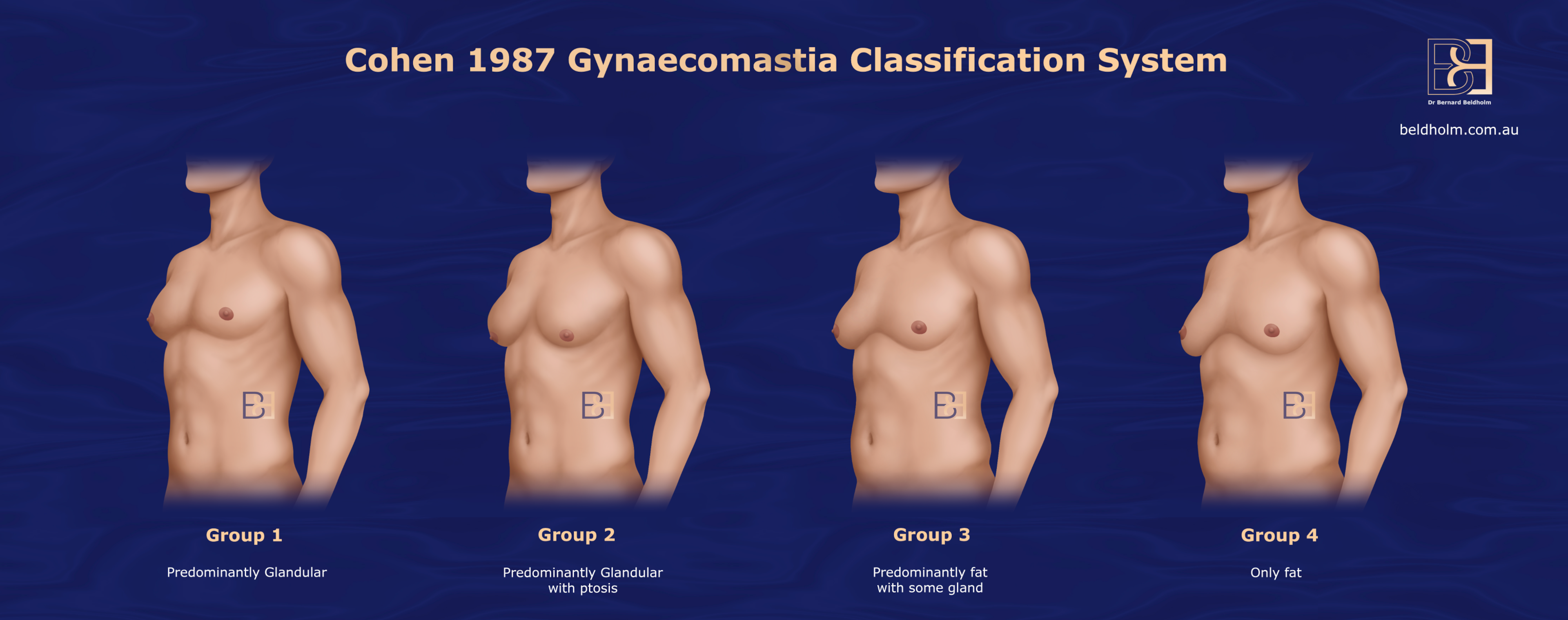
The Cohen system is divided into four groupings:
Cohen 1987 Gynaecomastia Classification System Explained
Cohen 1987 Gynaecomastia Classification System Group 1: Predominantly Glandular
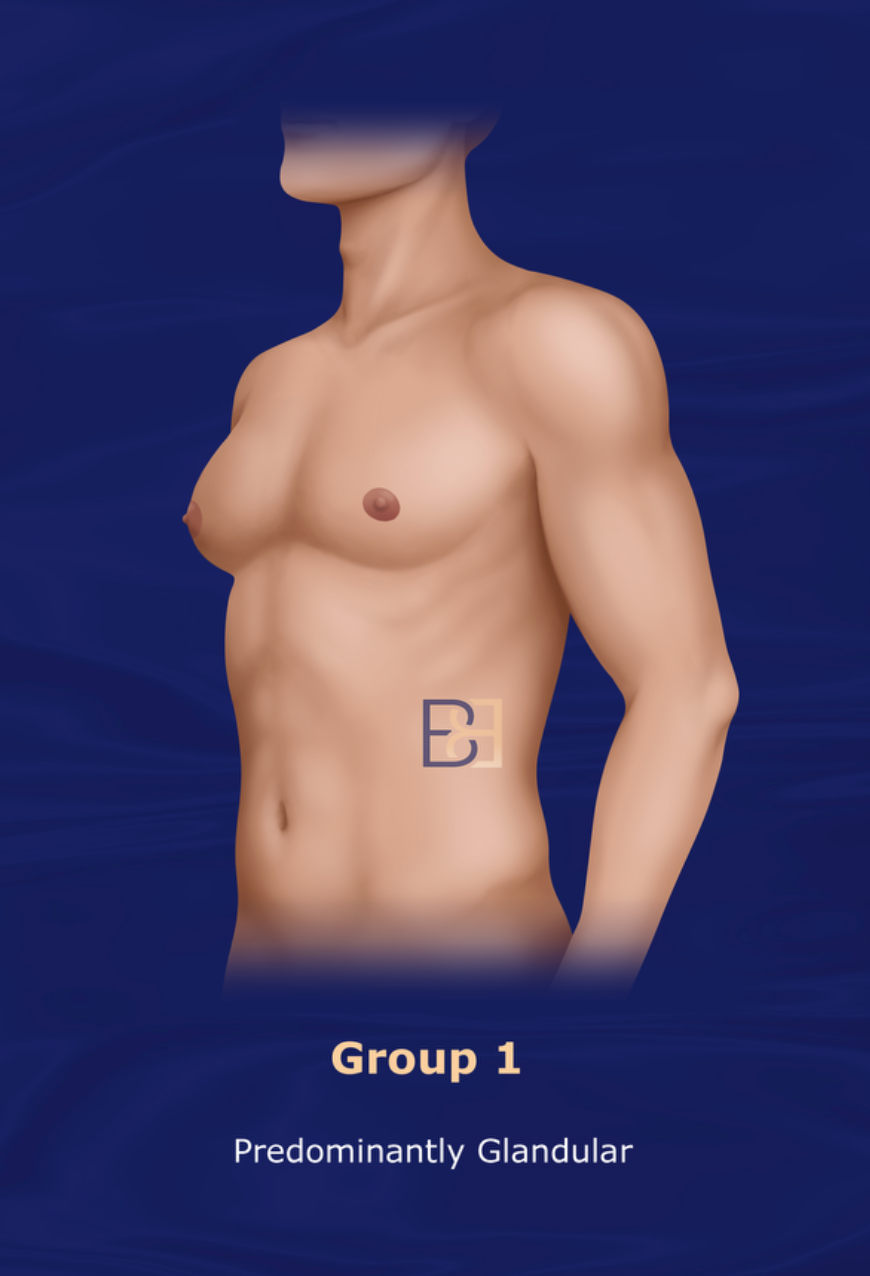
Presentation: The least severe grade, categorised by small breast enlargement, typically with no excess skin, and often with a slight localised glandular or fatty tissue presence around the nipple area.
Cohen’s recommended Treatment: Open Excision
Cohen 1987 Gynaecomastia Classification System Group 2: Predominantly Glandular with Ptosis
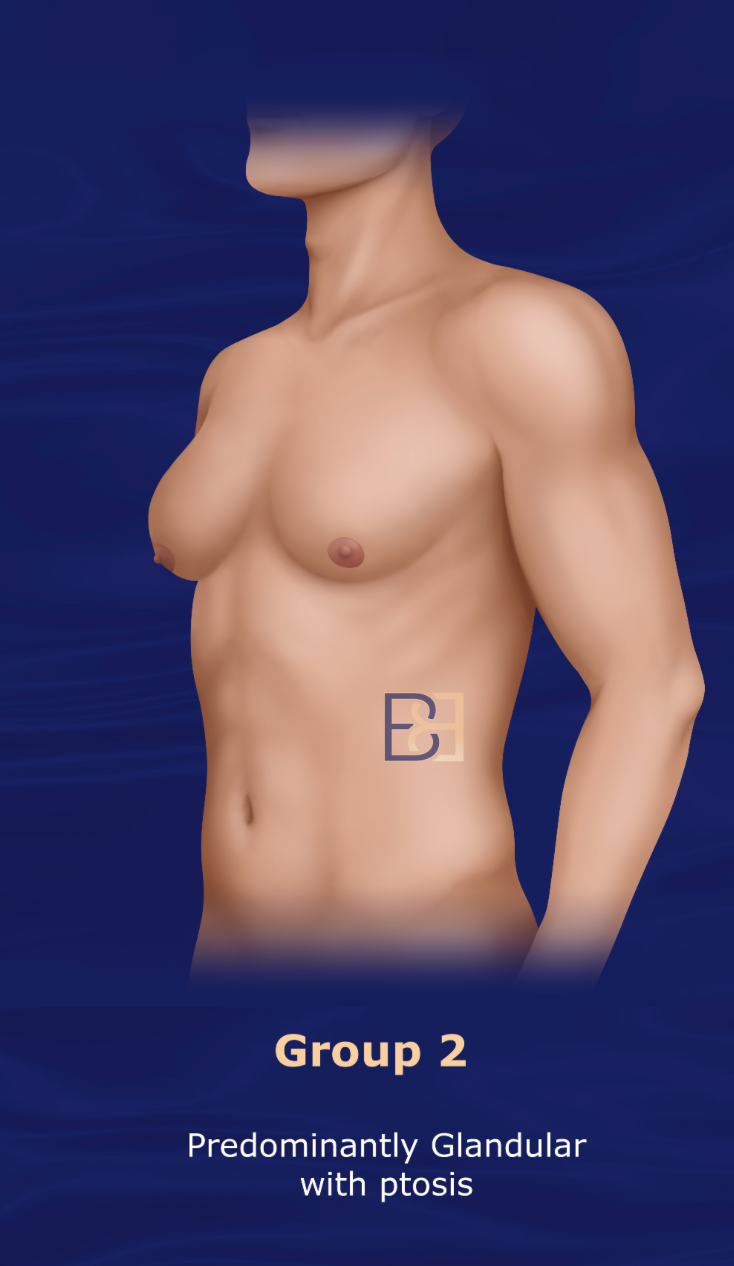
Presentation: Moderate enlargement with minimal skin excess, in Grade 2, the tissue extends beyond the areola but does not cause significant drooping of the chest contour.
Cohen’s recommended Treatment: Open Excision and Liposuction
Cohen 1987 Gynaecomastia Classification System Group 3: Predominantly Fat with Some Glandular
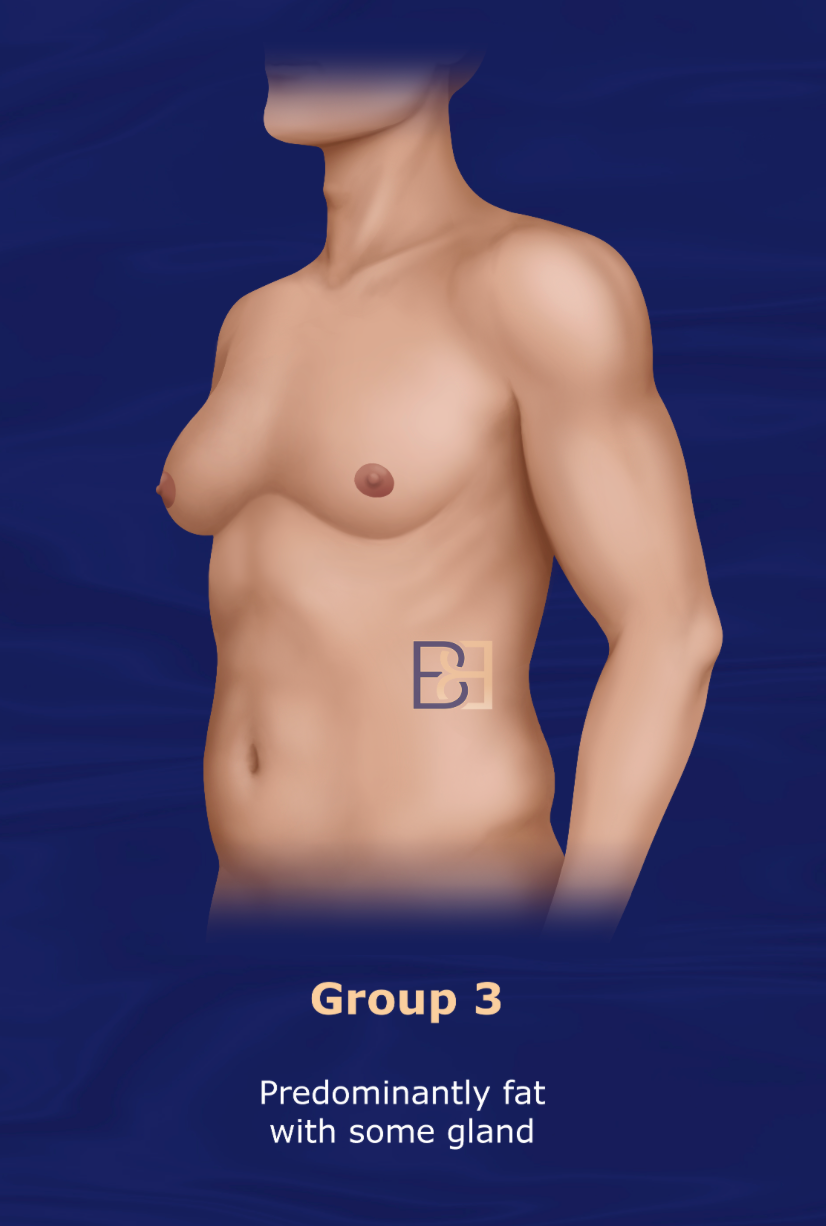
Presentation: Characterised by moderate to significant enlargement with excess skin and some ptosis, the chest contour may appear feminised. The presence of excess skin may require some degree of skin removal in addition to tissue excision.
Cohen’s recommended Treatment: Sharp dissection to destroy inframammary fold; open excision and liposuction
Cohen 1987 Gynaecomastia Classification System Group 4: Only Fat
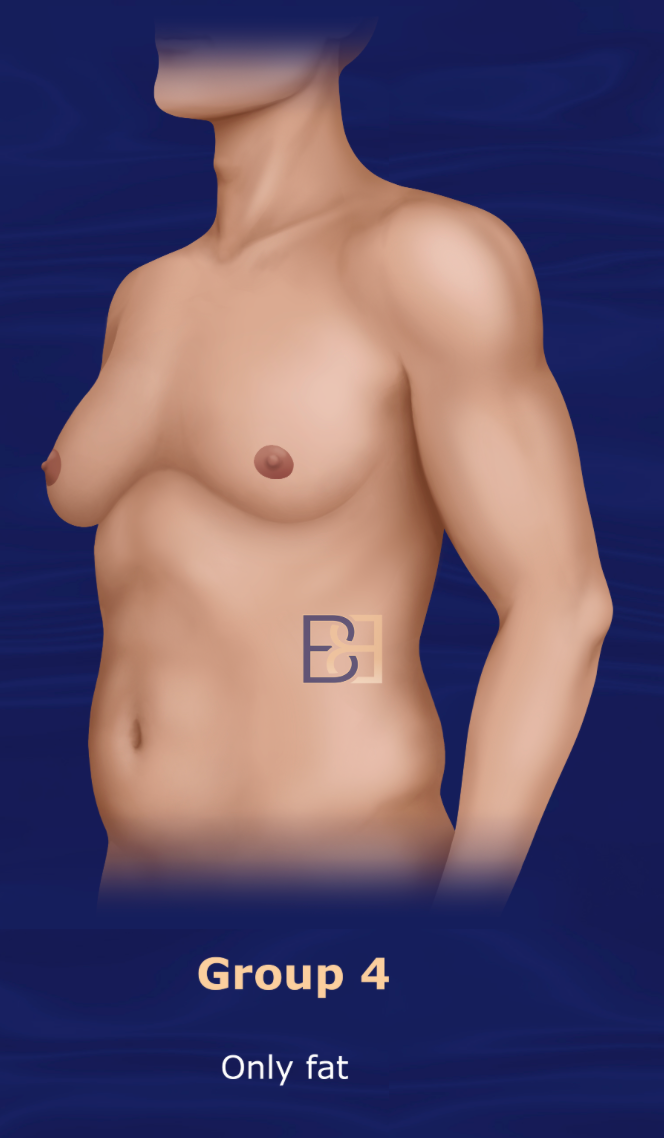
Presentation: Severe enlargement with pronounced excess skin and ptosis, resembling a female breast, this grade usually requires more extensive surgery, often combining tissue excision with skin removal and contouring.
Cohen’s recommended Treatment: Suction-assisted lipectomy (liposuction) only
Book your appointment online now
Practical Application of the Cohen’s Gynaecomastia Classification System
Offering a window into the state of gynecomastia in 1987, Cohen continues to serve as a useful historical reference. Though it is still widely referenced, vast ** in treatment methodology developed since the date of publication limit current practical uses.
Cohen Grading System Limitations
The Cohen 1987 Gynaecomastia classification system has several limitations, which may affect its applicability and effectiveness in modern clinical practice:
Limited Grading Factors
The Cohen system primarily considers tissue volume and skin excess but doesn’t account for factors such as tissue density, chest wall contour, or the presence of asymmetry, which can influence surgical approach.
Today’s approach often emphasises individualised treatment planning, which involves considering patient goals, skin quality, and the role of muscle definition. As these are increasingly relevant in modern gynecomastia correction, newer classification systems attempt to integrate these aspects.
Limited Detail on Etiology
The Cohen system primarily focuses on the physical presentation and severity of gynecomastia without considering underlying causes, such as hormonal imbalances, medications, or other health conditions. This limits its usefulness in ** treatment comprehensively since underlying causes often affect treatment choice.
Lack of Subcutaneous Fat Consideration
The Cohen classification doesn’t distinguish between glandular and fatty tissue components in the breast, which can influence the type of treatment (e.g., liposuction vs. gland excision). More modern systems provide a clearer distinction, as excess fat versus gland tissue may require different surgical approaches.
Absence of Intermediate Grading
The classification has relatively broad categories and, in many instances, may not account for the nuances in moderate cases. This can make it harder for surgeons to determine the most precise intervention for patients that may fall somewhere between these broad categories.
Lack of Focus on Individual Patient Factors
The system doesn’t consider patient-specific factors such as skin elasticity, age, and overall body type, which can significantly influence treatment outcomes and recovery.
Limited Guidance for Postoperative Expectations
While the Cohen system aids in selecting treatment, it doesn’t provide specific guidelines for postoperative care or outcome prediction. This can lead to variability in results and patient expectations, as each grade may still produce different aesthetic outcomes.
Outdated in Modern Practice
Since it was developed in 1987, it may not fully align with current surgical techniques and technology advancements, such as VASER liposuction or glandular sculpting. Modern classifications that incorporate these factors, provide a more detailed surgical roadmap.
Oversimplification
By grouping patients into just four categories, the Cohen system can oversimplify the complexity of gynecomastia cases, limiting personalised treatment plans that could lead to better, patient-specific results.
Benefits of the Cohen Gynaecomastia Grading System
The Cohen 1987 Gynaecomastia classification system offers several advantages in the clinical evaluation and treatment planning of gynecomastia. Here’s why it’s beneficial:
Standardised Assessment
By classifying gynecomastia into distinct grades, the Cohen system provides a common language for clinicians, allowing for consistent assessments, comparisons, and research across cases.
Treatment Planning
The grading scale helps guide the choice of surgical techniques. For example, minor cases (Grade I) may be treated with liposuction alone, whereas more severe cases (Grade III) might require tissue excision and skin removal. This specificity leads to more tailored and effective treatment strategies.
Predictable Outcomes
By following a classification that aligns severity with appropriate treatment, the system ** the likelihood of achieving desired aesthetic outcomes, including natural contouring and reduced scarring.
Improved Patient Communication
The Cohen system offers a way to explain the severity of gynecomastia to patients in a clear, structured manner. Patients can better understand why a particular treatment is recommended based on their grade and what results they can realistically expect.
Research and Documentation
The system supports better research and documentation, allowing for consistent case studies, outcome comparisons, and long-term studies on the efficacy of treatments for each grade.
Reduce Complications
By categorising the severity and suggesting appropriate procedures, the Cohen classification helps reduce the likelihood of overtreatment or undertreatment, thereby reducing potential complications like skin irregularities or scarring.

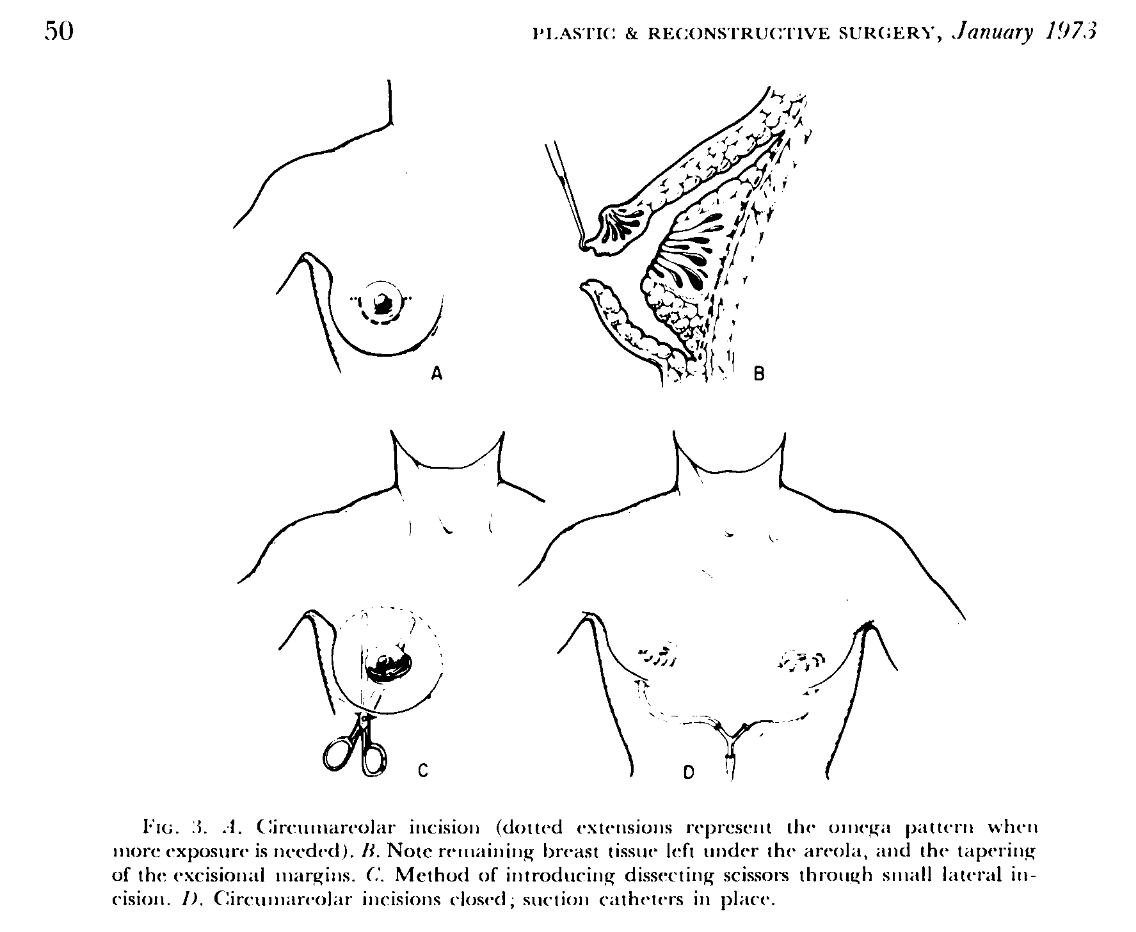
Cohen vs. Rosenberg, Suction Lipectomy-Only Dispute
In 1987, two ** surgeons, Dr. I. Kelman Cohen and Dr. Gary J. Rosenberg presented opposing views about treating gynaecomastia with suction lipectomy. Dr. Rosenberg, in his article, Gynecomastia: Suction Lipectomy as a Contemporary Solution (Ref 1), argued that a majority of gynaecomastia cases could be treated with suction lipectomy alone.
According to Rosenberg, gynecomastia can and should be corrected solely with the use of suction lipectomy, arguing that corrective techniques that require sharp dissection for removal of breast parenchyma are more physically and psychologically disturbing to the patient than the original deformity.
He noted that all classifications of the condition as highlighted in Simon, et al, which classify the grade of severity based on breast size and skin redundancy, can be treated with suction lipectomy alone.
Rosenberg comments that surgery that involves sharp dissection shares a common element of risk and associated complications, including seroma, loss of sensation, hematoma, infection, saucer and contour deformity, and excessive scarring, among others. He argues that the same technique can be used regardless of proportions of adipose and parenchymal tissue with advantages including (1) ease and speed of recovery, (2) completeness of adipose and parenchymal tissue removed, (3) more control of contour, (4) less scarring and surgically created deformity, (5) fewer complications, and (6) patients are able to return to their normal lifestyle after a very brief convalescence.
Dr. Cohen, in an article published in 1987, sharply disagreed with the Rosenberg hypothesis, arguing that surgical correction of gynaecomastia cannot be accomplished with suction alone, as “significant breast parenchyma cannot be aspirated through standard cannulas regardless of their size.” (Ref 2)
Cohen tested the Rosenberg theory and attempted to perform the procedure using suction alone, however, “The method failed.” Challenging others to validate the Rosenberg hypothesis, Cohen warned that one should proceed with caution, and “operate on principles, not on fancy.”

Dr Beldholm’s Final Thoughts
Overall, while the Cohen system, recognized for its achievements in 1987, provides a foundational approach to classifying gynecomastia, it does not capture the full spectrum of treatment options and outcomes achievable with today’s surgical advances.
Dr Beldholm offers the following comments of the Cohen system:
- Overly simplistic: While the Cohen classification provides a helpful baseline, it lacks the depth and adaptability of newer systems that offer more precise categorization and guidance for current treatment options.
- Subjective: As there is no definition of what “predominantly glandular” means, the article is very subjective, which may be why Rosenberg developed his own take on a less invasive treatment for gynaecomastia.
- Vague: There is also no obvious definition of what “ptotic” means.
- No severity grading: There is no gradation of the severity of gynaecomastia.
- Antiquated: This grading system is quite old and not very useful in current applications.
Resources
- Gynecomastia: Suction Lipectomy as a Contemporary Solution, Rosenberg, Gary J., Division of Plastic Surgery, University of Miami, July 7, 1986; revised November 20, 1986. Presented at the Annual Meeting of Southeastern Society of Plastic and Reconstructive Surgeons, May 1986, Boca Raton, Florida.
- Kelman Cohen, M.D., Department of Plastic Surgery, Medical College of Virginia Richmond, Va. 23298