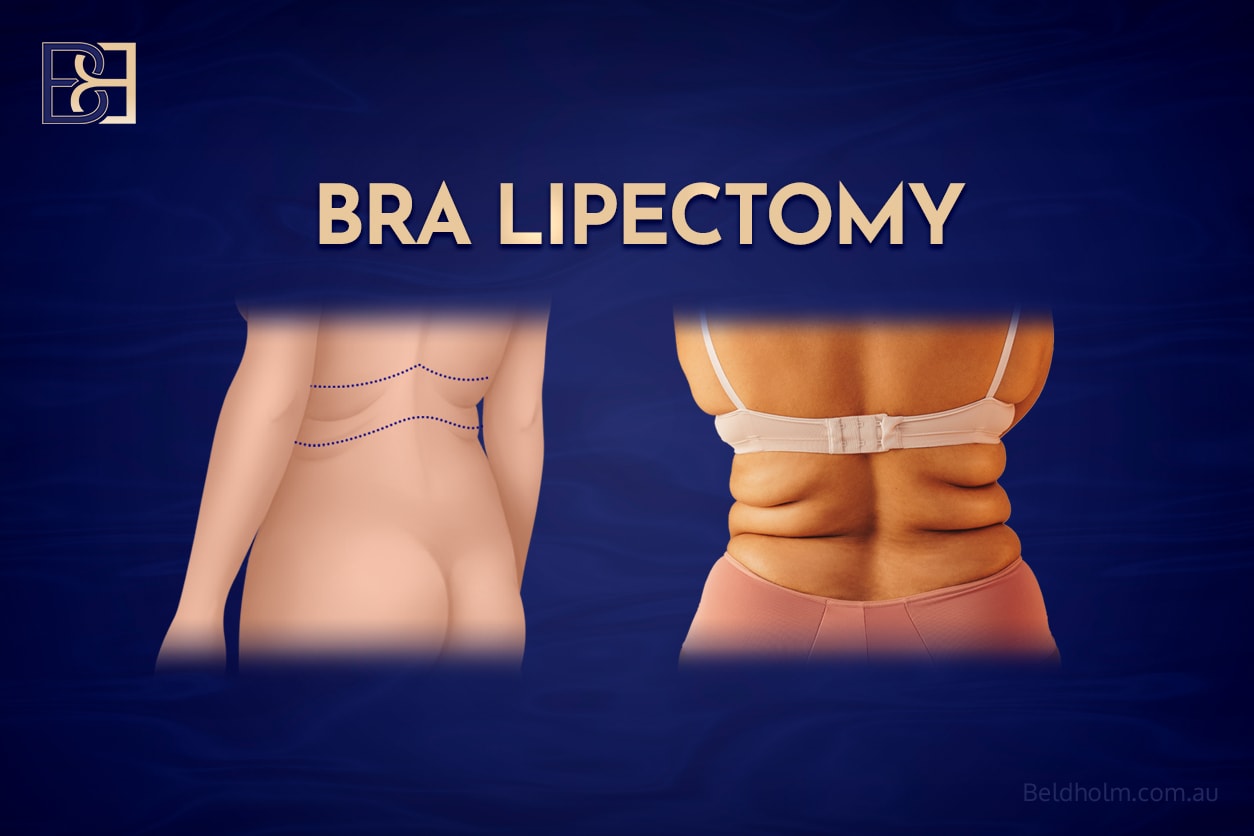
Recovering from a bra lipectomy(upper back lipectomy), also known as a bra line back lift, is a structured and closely supervised process in Dr Bernard Beldholm’s practice. While the surgical procedure itself treats excess skin and redundant tissue along the upper back, the recovery process plays a central role in wound healing, comfort, scar quality, and longer-term surgical outcomes.
This comprehensive guide focuses on recovery from a bra lipectomy (upper back lipectomy), outlining what patients can expect from the first day after surgery through long-term follow-up at 12 months. It reflects Dr Beldholm’s usual post-operative routines in the Hunter Valley region, including PICO dressing changes at day 7, LED light therapy in the Lorn rooms, and intensive follow-up during the first two weeks.
What Is a Bra Lipectomy (upper back lipectomy) and Why Recovery Matters
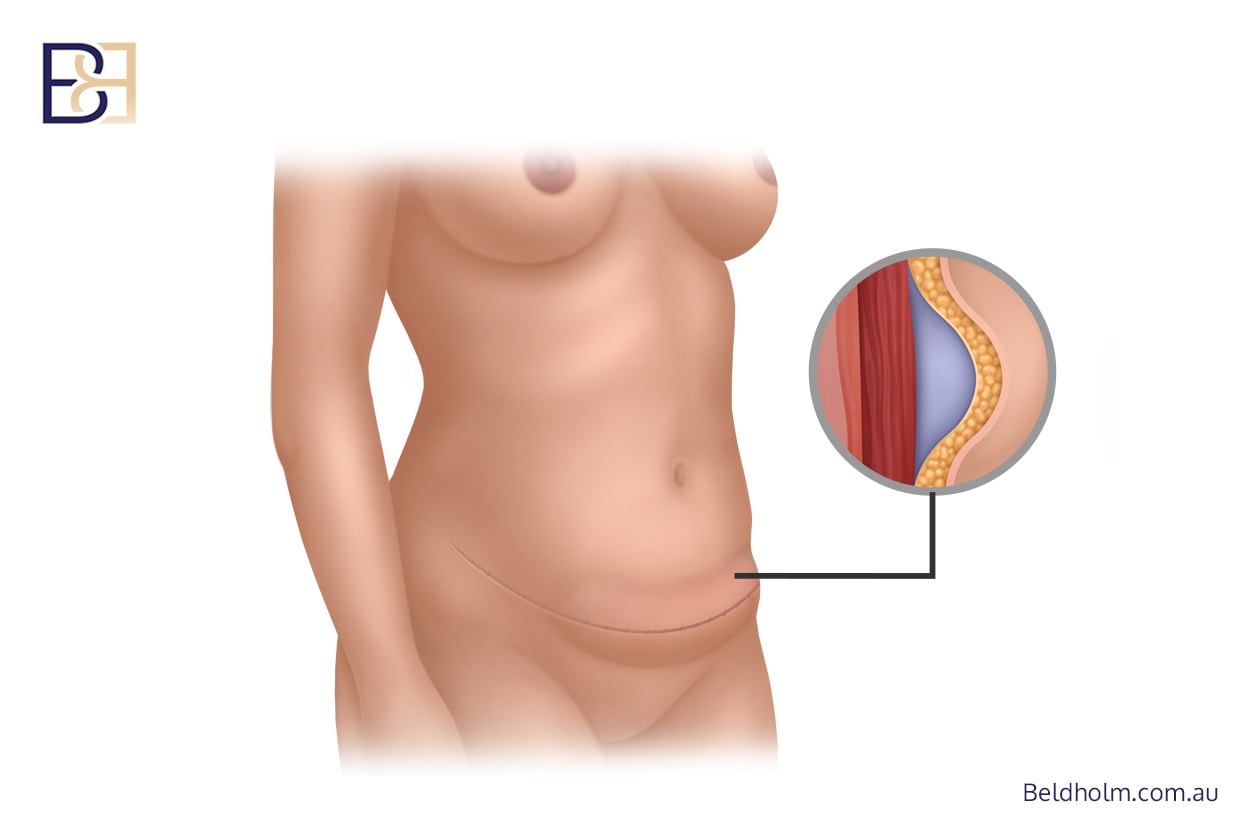
A bra lipectomy (upper back lipectomy) is a surgical procedure designed to remove excess skin and, when required, fat from the upper and middle back. It is commonly performed in patients who have experienced significant weight loss, including after bariatric surgery, or in individuals with reduced skin elasticity following substantial weight fluctuations.
This procedure is sometimes referred to as a back lift or bra line back lift, as the incision is positioned along the bra line to allow concealment beneath clothing. It may be performed as a standalone upper body lift (upper back lipectomy) or combined with other body lift procedures such as a tummy tuck (abdominoplasty), breast reduction (Reduction mammoplasty), breast lift (mastopexy), or lower body lift (belt lipectomy).
Recovery is not simply a waiting period. It is an active phase of care designed to:
- Support wound healing
- Reduce swelling and fluid accumulation
- Protect incision sites
- Reduce risks such as infection or seroma
- Optimise surgical outcomes over time
Immediate Post-Operative Care After a Bra Line Back Lift (upper back lipectomy)

Hospital Stay and Early Monitoring
A bra line back lift (upper back lipectomy) is usually performed under general anaesthesia at Maitland Private Hospital. Depending on the extent of surgery and whether other procedures are performed at the same time, patients may be discharged the same day or remain in the hospital overnight.

Before discharge, patients are:
- Reviewed by Dr Beldholm
- Assessed by nursing staff
- Provided with written recovery instructions
- Prescribed appropriate pain medication
Most patients will feel tightness across the bra line rather than sharp pain. This sensation reflects normal tension across the incision sites.
The First Week: Early Recovery Period

The first week is one of the most important stages in the recovery period following bra lipectomy (upper back lipectomy).
PICO Dressings and Wound Care
At the end of surgery, PICO negative pressure dressings are applied over the incision sites. These dressings are designed to:
- Reduce fluid accumulation at the surgical site
- Support wound healing
- Minimise tension across incision sites
- Lower the risk of wound healing complications
During the first week:
- Dressings must remain intact and dry
- Showering is usually permitted with care
- The surgical site should not be submerged in water
- Arms should remain close to the body to reduce strain
Pain Medication and Comfort
Prescription pain medications are provided and should be taken exactly as directed. Many patients transition to simple pain medication within several days. Anti-inflammatory medications should only be used if approved, as some may impair healing.
Day 7: PICO Dressing Change Appointment

A key milestone when recovering from a bra lipectomy (upper back lipectomy) is the scheduled day 7 post operative appointment.
At this visit:
- PICO dressings are removed
- Incision sites are carefully examined
- Early wound healing is assessed
- Dressings are changed to Hypafix tape for ongoing support
This appointment allows early identification of wound healing concerns, which is critical for long-term outcomes.
Intensive Follow Up During the First Two Weeks
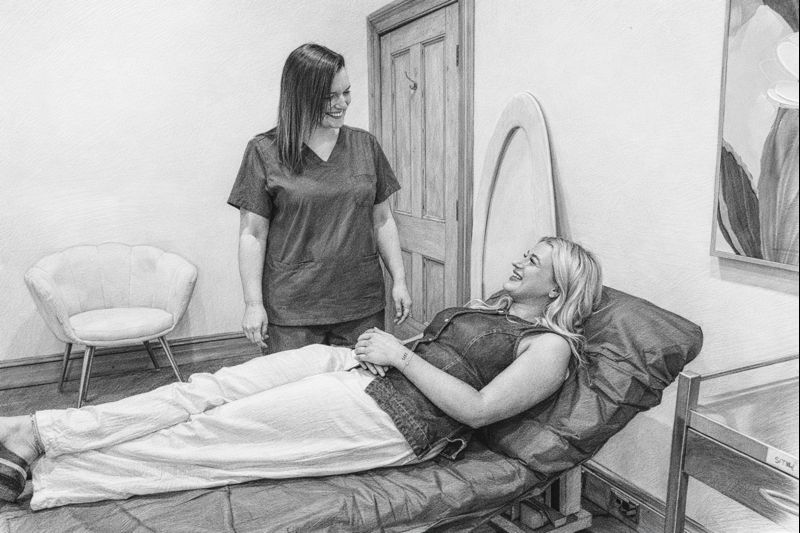
Frequent Clinical Reviews
Book your appointment online now
Dr Beldholm’s usual protocol involves intensive follow-up appointments during the first two weeks after surgery. Most patients are reviewed two to three times per week during this early phase.
These visits allow:
- Monitoring of incision sites
- Assessment of swelling and bruising
- Review of pain medication requirements
- Early management of wound healing issues
Early and frequent review is a cornerstone of postoperative care in this practice.
LED Light Therapy in the Lorn Rooms
As part of recovery support, LED light treatment is commonly used during early follow-up appointments in the Lorn consultation rooms. LED therapy is used as an adjunct to:
- Support the healing process
- Reduce inflammation
The number of LED sessions varies depending on individual healing response, medical history, and surgical extent.
Activity Restrictions After Bra Lipectomy

Movement and Daily Activities
During the first few weeks post surgery:
- Arms should remain adducted where possible
- Overhead reaching should be avoided
- Heavy lifting is restricted
- Sudden twisting movements should be minimised
Light walking is encouraged to support circulation and reduce the risk of blood clots.
Exercise and Physical Activity
- Strenuous exercise should be avoided for at least six weeks
- Heavy lifting must be avoided during early wound healing
- Intense exercise is reintroduced gradually under guidance
Returning to activity too early can place excess tension on incision sites and impair proper healing.
Compression Garments and Swelling Management
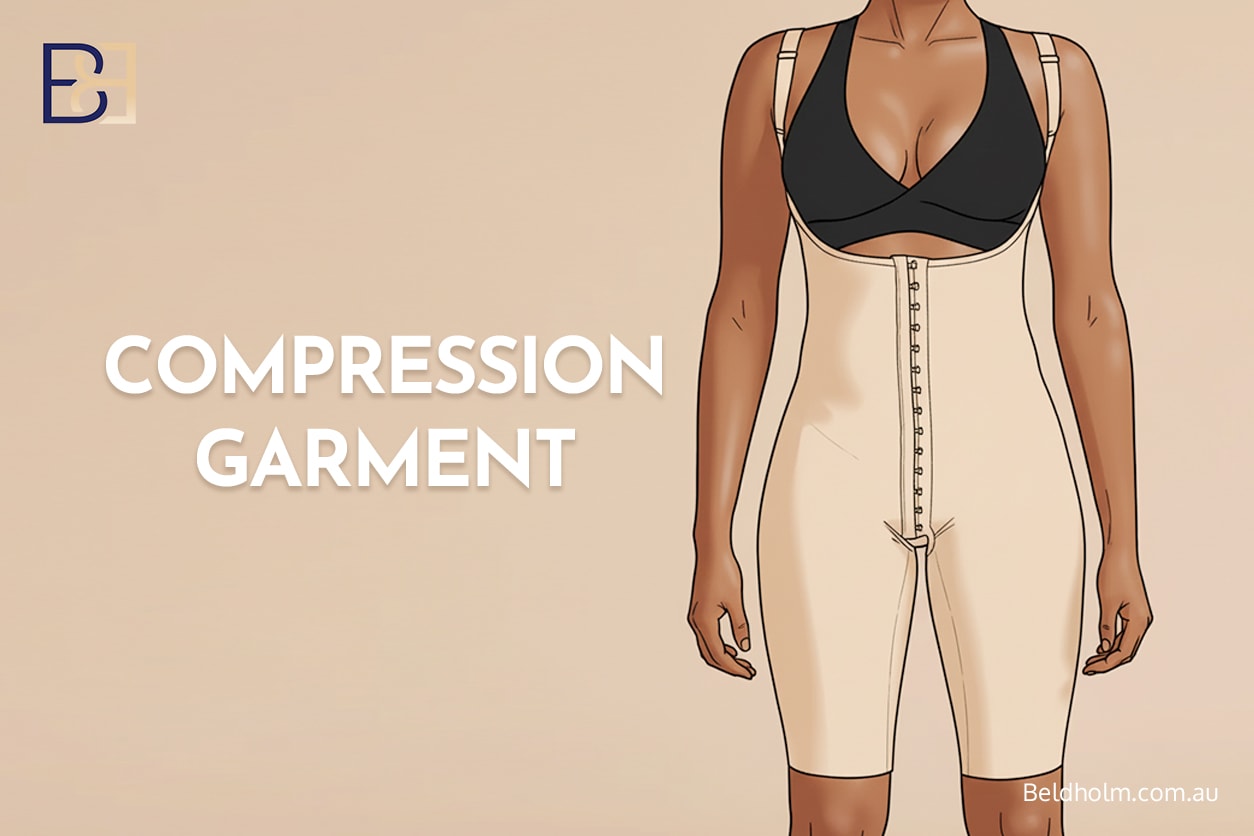
Most patients are advised to wear compression garments following a bra line back lift. Compression garments help:
- Reduce swelling
- Support underlying tissues
- comfort during movement
Wearing compression garments exactly as instructed is an important part of post operative care and can influence recovery timelines.
Weeks Two to Four: Ongoing Healing Phase
By weeks post surgery two to four:
- Swelling gradually reduces
- Bruising continues to fade
- Most patients resume light daily activities
- Wound healing continues beneath the skin surface
Hypafix tape is usually maintained during this stage to support incision sites and minimise tension.
Returning to Work
- Working from home or desk-based roles: often possible within 1–2 weeks
- Physically demanding roles: may require extended recovery time
Recovery time varies depending on overall health, medical history, and whether other procedures were performed.
Long-Term Recovery and Follow Up Appointments
Structured follow up appointments are scheduled at:
- 1 month
- 3 months
- 6 months
- 12 months
These appointments allow ongoing assessment of:
- Wound healing
- Scar maturation
- Residual swelling
- Surgical outcomes
Long-term follow up is essential, as scar and tissue changes continue for many months after surgery.
Scar Care and Wound Healing Over Time

Scar appearance following a bra line back lift evolves gradually. During follow up appointments, patients receive guidance on:
- Silicone-based scar treatments
- Tape management
- Sun protection strategies
Wound healing differs between individuals and is influenced by skin elasticity, overall health, and adherence to recovery instructions.
Patients Travelling From Outside the Hunter Valley
Patients travelling from interstate or regional areas are advised to:
- Remain locally for 7–10 days after surgery
- Attend early follow up appointments in person
- Utilise telehealth for later reviews where appropriate
Care is often coordinated with the patient’s GP once early recovery is complete.
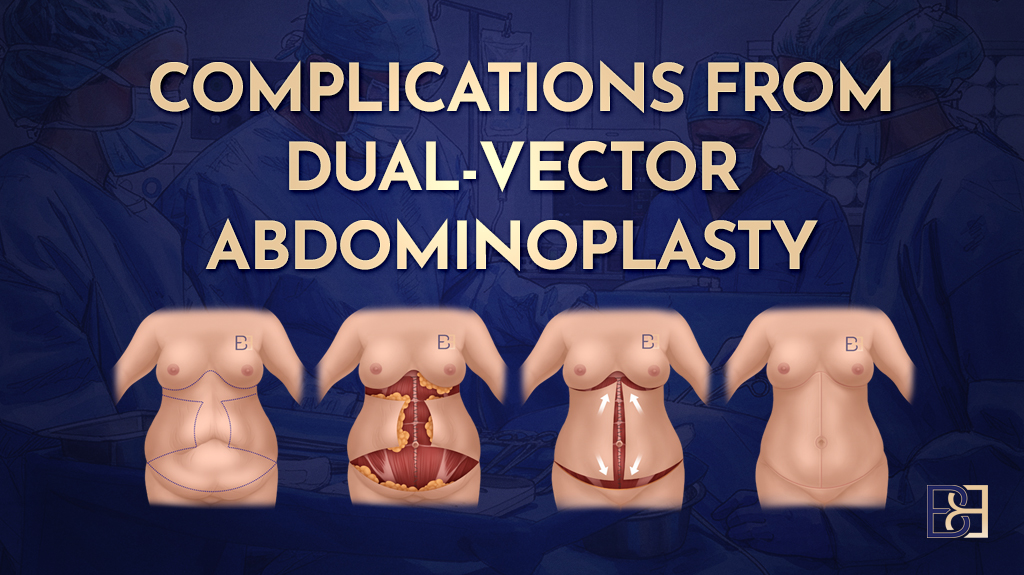
Potential Risks During the Recovery Process
As with any surgical procedure, potential risks exist during recovery, including:
- Delayed wound healing
- Infection
- Seroma or fluid accumulation
- Scar widening
- Blood clots
Close monitoring and early intervention during follow up appointments reduce the impact of complications should they arise.
Recovery, Body Heals, and Realistic Expectations

Every patient’s body heals differently. Maintaining a stable weight, a healthy lifestyle, and realistic expectations is essential. A bra lipectomy (upper back lipectomy) is intended to remove redundant skin rather than produce weight loss.
Final surgical outcomes continue to evolve over several months.
Final Thoughts on Recovering From a Bra Lipectomy

In Dr Bernard Beldholm’s practice, recovery is treated as an active and carefully managed phase of care. Structured dressing changes, LED light therapy, compression garment use, and intensive early follow-up are all used to support proper healing and optimise surgical outcomes.
Attending all follow-up appointments and following recovery instructions closely is essential for ensuring proper healing and long-term results.