Book your appointment online now
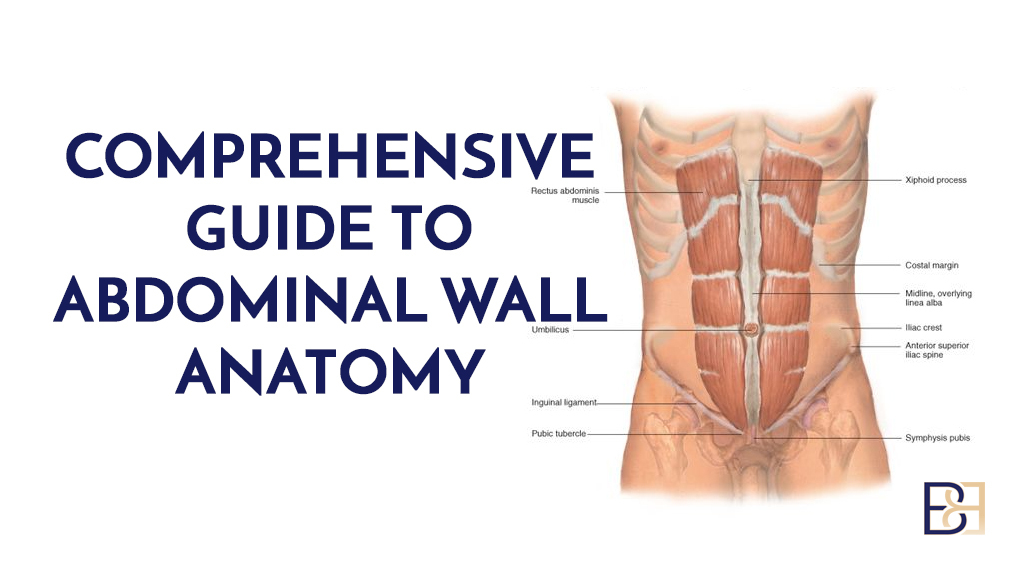
Umbilical hernia is a common condition in infants, occurring as a protruding navel that is particularly noticeable when the infant cries. It’s mostly painless and heals on its own between the ages of one and five. An umbilical hernia may also occur in adults, also appearing as a protruding umbilicus, noticeable when coughing or lifting heavy objects. Unlike babies, for which the condition is generally painless, umbilical hernia in adults can be unattractive, painful, and can be a threat to one’s health.

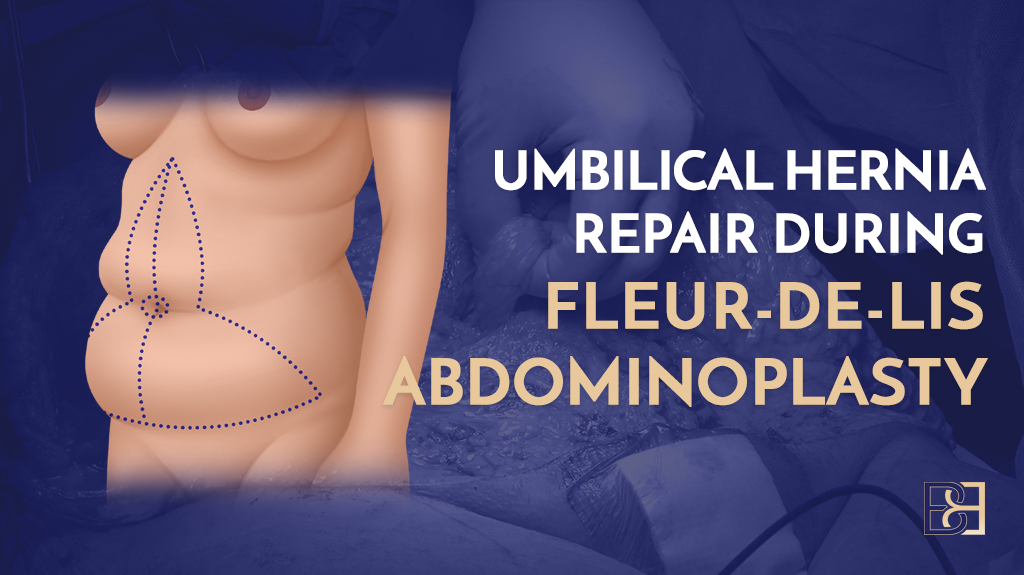
Umbilical hernia results from weak abdominal cavity muscles. This is a common condition in massive weight loss patients and postpartum women. Combining Fleur-de-Lis abdominoplasty with hernia repair offers an opportunity to repair the weak and separated abdominal muscles, correct umbilical hernia, and simultaneously remove excess skin and fatty tissue in the abdomen.
In this guide, I’ll cover everything you need to know regarding umbilical hernia repair during fleur-de-lis abdominoplasty, including the procedure’s process.
Umbilical Hernia Explained
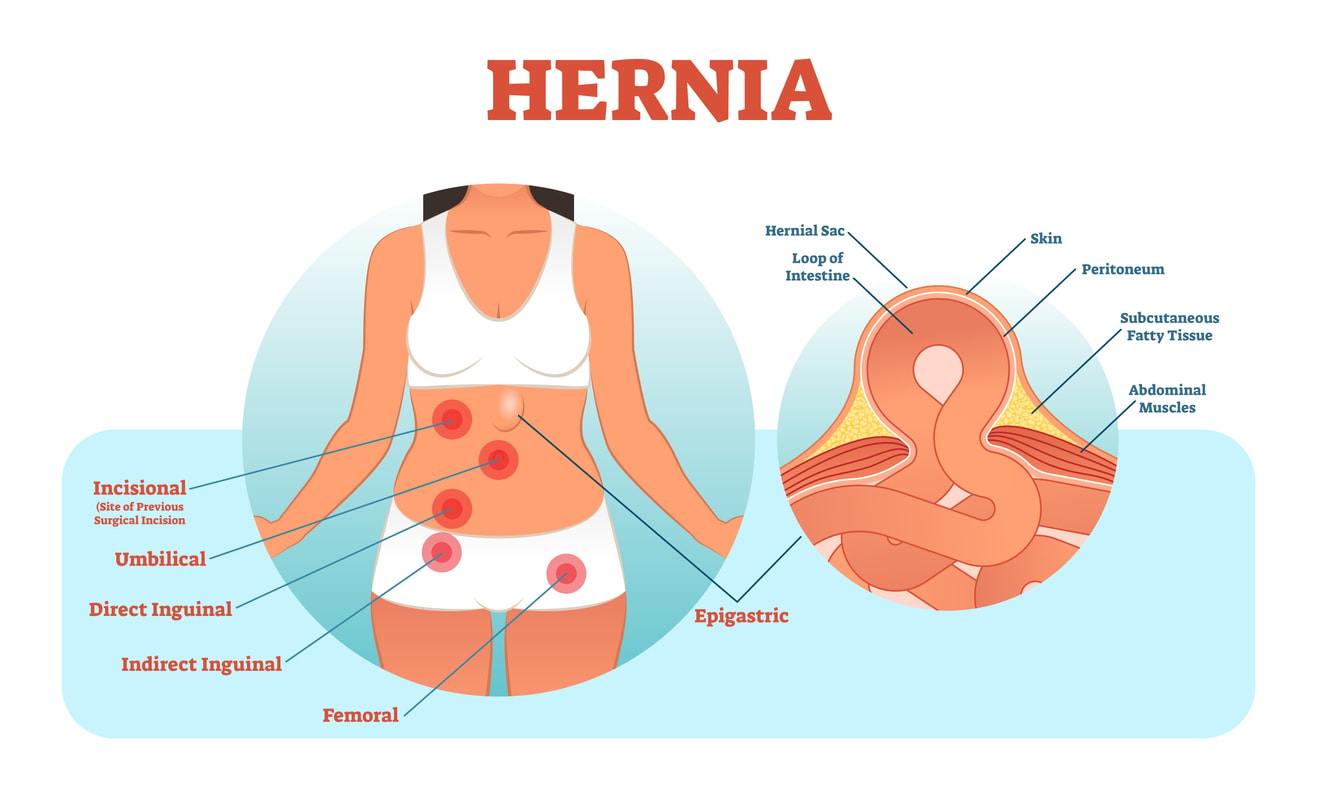
A hernia is a condition where the body’s internal organs protrude through the muscle wall, a common phenomenon involving the intestines or stomach. The type of hernia is determined by the exact location where the hernia develops.
An umbilical hernia occurs at the umbilicus (navel), happening when the intestine pushes through weakened abdominal muscles, causing a noticeable protrusion on the skin. As noted, an umbilical hernia may occur in adults, requiring surgical intervention.
Many patients report that the protrusion becomes noticeable particularly when coughing, sneezing, or lifting heavy objects. Some of the major causes of umbilical hernia in adults include multiple pregnancies, accumulation of abdominal fluid, and obesity. The hernia sac mainly contains omentum or preperitoneal fat, and a section of the small intestine.
Adult umbilical hernias are grouped by size, with those less than 1 cm considered small, those between 1 cm to 4 cm considered medium, and those larger than 4 cm considered large. A study by PubMed notes, “[u]mbilical hernias account for 6% to 14% of all adult abdominal wall hernias and are second in frequency only to inguinal hernias.”

Symptomatic vs Asymptomatic Hernia
Hernia may occur as symptomatic or asymptomatic. Let’s take a look at each one of them to create a distinction.
Asymptomatic Hernia
An asymptomatic hernia is commonly painless, involves little or no symptoms, and it’s not as noticeable. This type of hernia has a protrusion of less than 1 cm and mostly appears as an impulse while coughing. Most doctors commonly diagnose an asymptomatic hernia during a general check-up. Asymptomatic hernia doesn’t require surgery, and I always recommend pushing the protrusion back.
Symptomatic Hernia
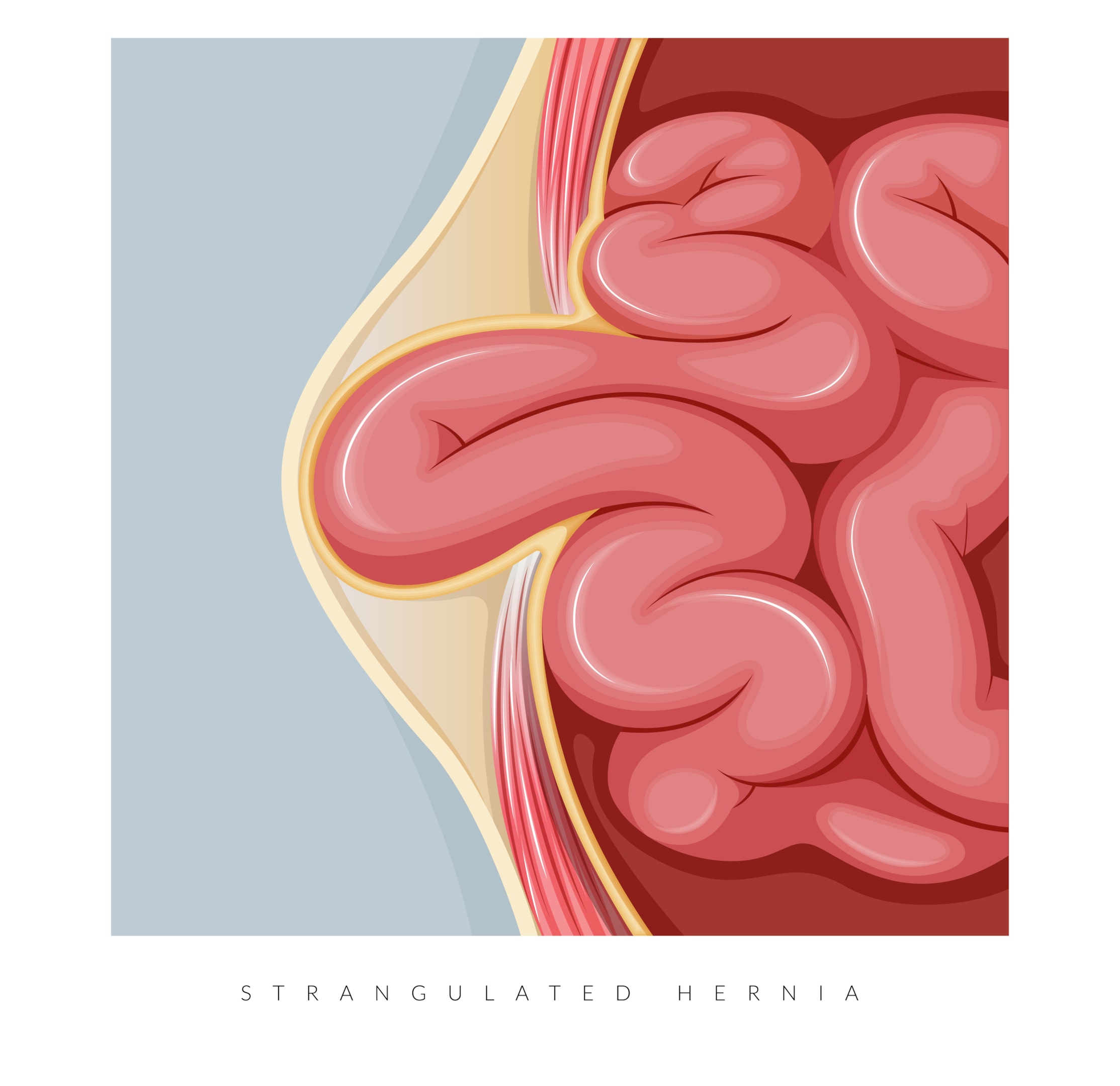
Symptomatic hernia is characterised by discomfort and pain, particularly when lifting heavy objects and even coughing. The protrusion is much larger than in an asymptomatic hernia, and there’s discolouration around the area. Symptomatic hernias often require immediate surgical intervention. This helps prevent an increase in size, which may cause hernia strangulation or bowel obstruction.
Umbilicoplasty for Umbilical Hernia Repair
Umbilicoplasty is a reconstructive procedure for repairing an umbilical hernia. Additionally, I use the procedure to treat the appearance of the umbilicus.
Neo-umbilicoplasty is a common procedure for postpartum patients. This is because most postpartum patients experience pain, discomfort, and a protrusion in the umbilical region. Sometimes, the umbilicus is missing due to destruction during pregnancy or agenesis, necessitating neo-umbilicoplasty. The procedure aims to reconstruct the umbilicus and it’s therefore commonly known as umbilical reconstruction.
Combining Umbilicoplasty with Fleur-de-Lis Abdominoplasty
It is possible to undergo umbilicoplasty with Fleur-de-lis simultaneously. Umbilicoplasty is a common procedure involving the doctor reconstructing and enhancing the belly button appearance. A study notes, “[u]mbilicoplasty is a key component of any abdominoplasty as the umbilicus has been described as the central aesthetic subunit to the abdomen.” The same study also notes, “[u]mbilicoplasty in abdominal contouring procedures involves repositioning and in setting of the umbilicus following excision of excess skin and subcutaneous tissue with or without plication of the abdominal wall.”

Understanding Fleur-de-Lis Abdominoplasty
Fleur-de-Lis abdominoplasty is an advancement of the standard abdominoplasty procedures. The procedure is ideal for massive weight loss patients with significant vertical and horizontal skin laxity and separated abdominal muscles, which is challenging to perform with standard abdominoplasties. A study on Fleur-de-Lis notes, “[I]deal candidates are patients with upper abdominal skin laxity who may not achieve an adequate aesthetic result with transverse-only excision.”
The surgery involves a horizontal and vertical incision that meet at the groin area forming an inverted T. When partially closed, the incision resembles the Irish flower, and this is the origin of the procedure’s name.
The vertical incision makes the procedure unique by allowing the specialist surgeon to treat vertical skin laxity effectively and correct separated abdominal muscles. Due to significant skin removal, there is always a need to reconstruct and reposition the umbilicus. Therefore, I incorporate umbilicoplasty into the procedure.
Benefits of Combining the Procedures
Reduced Downtime
Patients are often eager to resume their normal routines post-surgery. Opting for separate umbilicoplasty and FDL procedure will naturally require more recovery time. However, combining both surgeries minimises time off work and shortens the period away from family, pets and daily responsibilities. This makes it a better and more efficient option for many.
Single Anaesthesia Events
At the start of your umbilicoplasty and Fleur-de-lis abdominoplasty, an anaesthetist will place you under general anaesthesia. You will experience effects like confusion, drowsiness and a sore throat. Combining these procedures will reduce the number of times you experience these effects. Additionally, you’ll spend less on anaesthesia costs as you’ll pay once (not twice) for separate procedures.
Minimal Risks
Surgical procedures pose the risk of complications during and after surgery. These complications include wound infection, abnormal scarring, hematoma, seroma, blood clots, and more. Combining the procedures reduces the risk of complications that may otherwise result from two separate surgical procedures.
Optimised Recovery Period
Combining the procedures means you’ll have a single recovery period.
Comprehensive Procedure Results
Undergoing umbilicoplasty and Fleur-de-Lis simultaneously optimises the results since I will focus on multiple issues at once. Therefore, the procedure leads to long-term results that get you closer to your personal goals.
Lower Cost
During a combined surgical procedure, you’ll only pay a single anaesthesia fee, hospital fee, and surgeon’s fee. This lowers the cost significantly. Additionally, you cut down on the costs related to travel to and from the clinic for consultation, procedure, and follow-up visits.
Step-by-Step Surgical Procedure
To achieve optimal results during a combined procedure, I develop a detailed plan in advance that I follow during the procedure. The following outlines key steps involved in the process.
Administering the Anaesthesia

Before surgery, I will walk you through what to expect during the procedure and answer any questions you may have, after which the anaesthetist will administer general anaesthesia. The amount of anaesthetic used will depend on factors such as your medical history and tolerance to medicine. It’s important to notify the anaesthetist of any allergies to anaesthesia you have to ensure we are well prepared for any complications.
Making the Incisions
After the anaesthesia has been administered and you are unconscious, you’ll be taken to the operating room, where the surgery will begin.
I’ll start by making incisions on your abdomen.
Fleur-de-lis involves two incisions, a vertical and a horizontal incision. The horizontal incision runs hip-to-hip just above the pubic region, while the vertical incision runs along the midline. The vertical incision intersects the horizontal incision at the pubic region and runs upwards to just below the ribs. I’ll also make an incision around the umbilicus (belly button) for reconstructing the belly button and hernia repair.
Umbilicoplasty
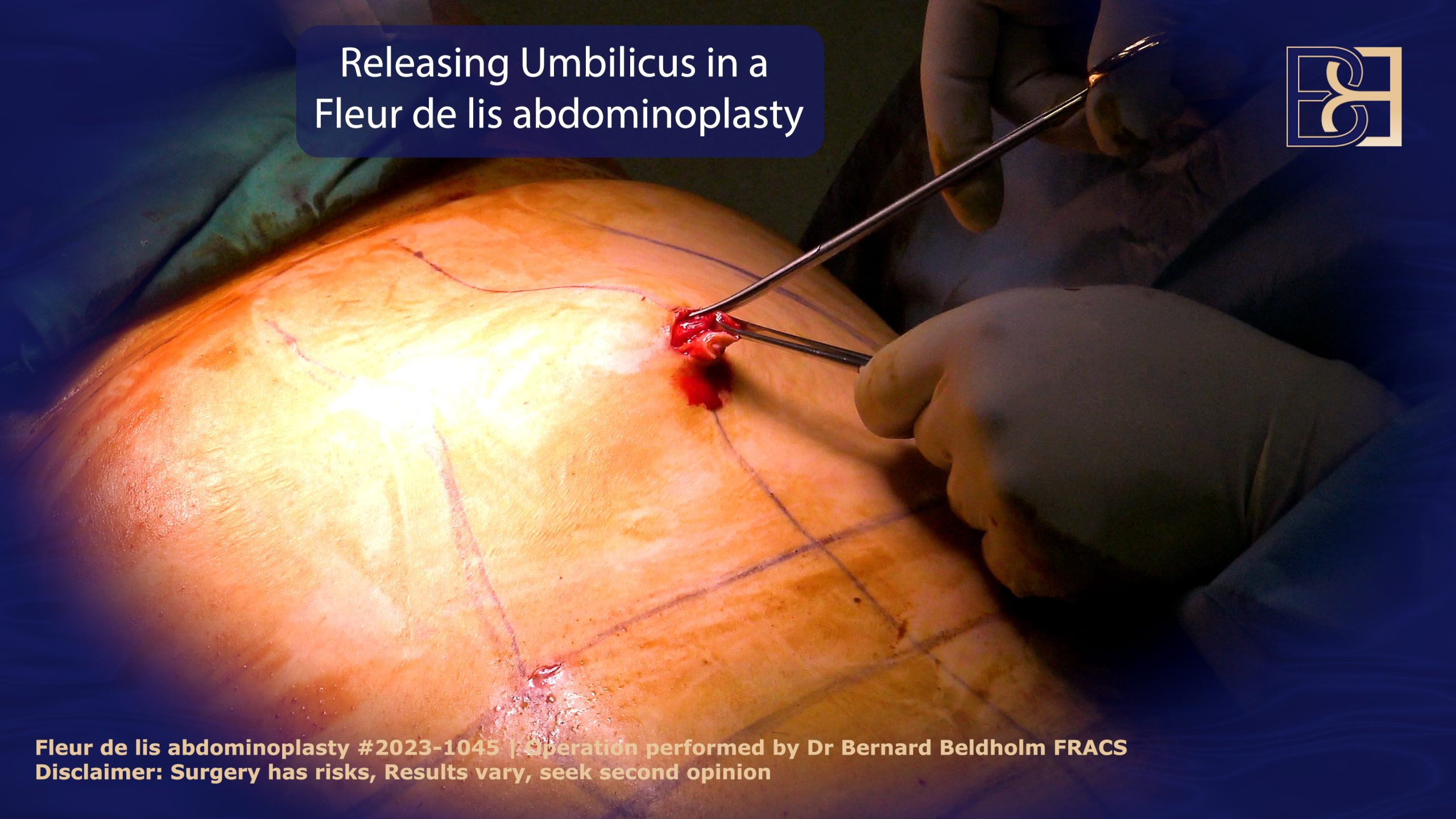
The next step after making the incisions is umbilicoplasty. The operation helps to reconstruct the umbilicus. To do this, I remove excess fat and skin tissue around the umbilicus and reshape it. Reconstructing the umbilicus requires experience and expertise.
Umbilical Hernia Repair
The approach for umbilical hernia repair depends on the hernia size, and certain factors like the patient’s body mass index (BMI) and comorbidities like obesity.
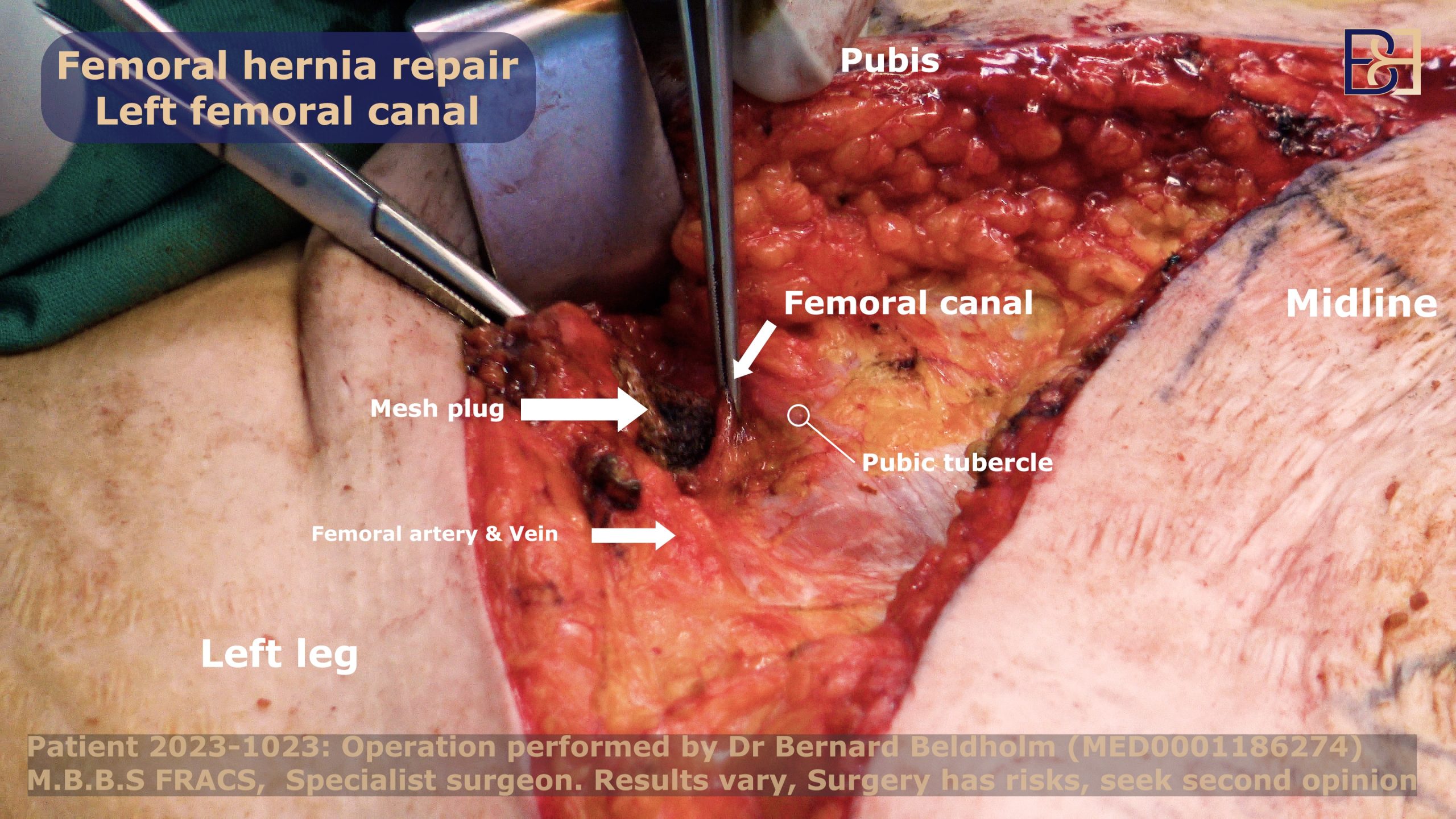
To repair the umbilical hernia, I will first locate the hernia sac. After identifying it, I will remove the sac and gently push the hernia contents back into the abdomen. Then, I will close the opening to prevent the hernia from recurring. Typically, I will use a small dual-mesh to ensure a tension-free repair.
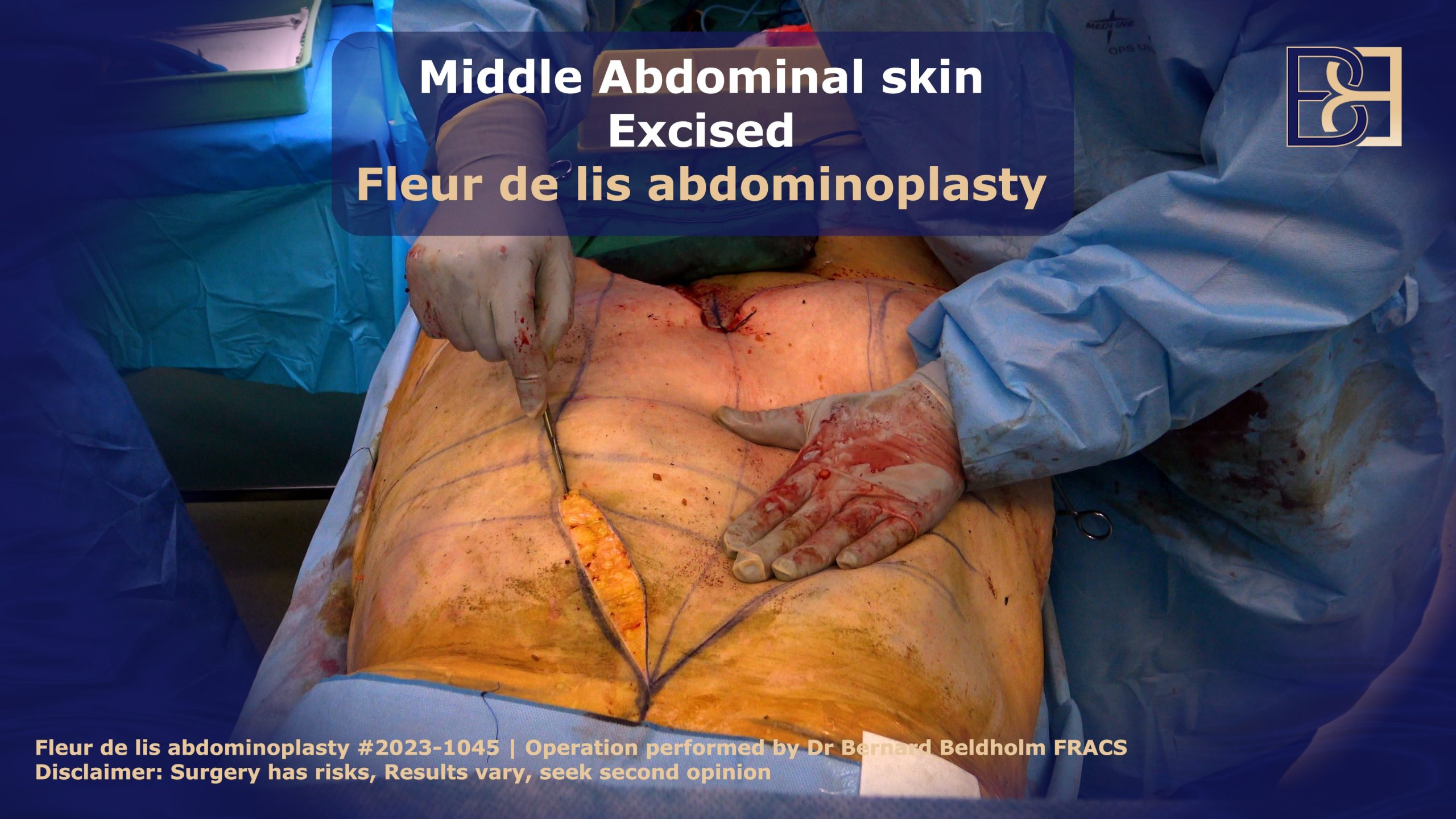
Fleur-de-lis Abdominoplasty
FDL abdominoplasty focuses on the excess and loose skin on your abdomen. During the procedure, I’ll dissect the excess skin tissue in the upper and lower abdomen. The amount of skin excised depends on the amount of excess skin present and the patient’s desired abdominal contour.
Suction-Assisted Lipectomy (VASER Liposuction)
If there is excess fat, I will incorporate Suction-Assisted Lipectomy (VASER liposuction) into the procedure to effectively remove the excess fatty tissue. The ultrasonic technology used in Suction-Assisted Lipectomy breaks down fat cells while minimising damage to the surrounding tissues.
Repair Separated Abdominal Muscles
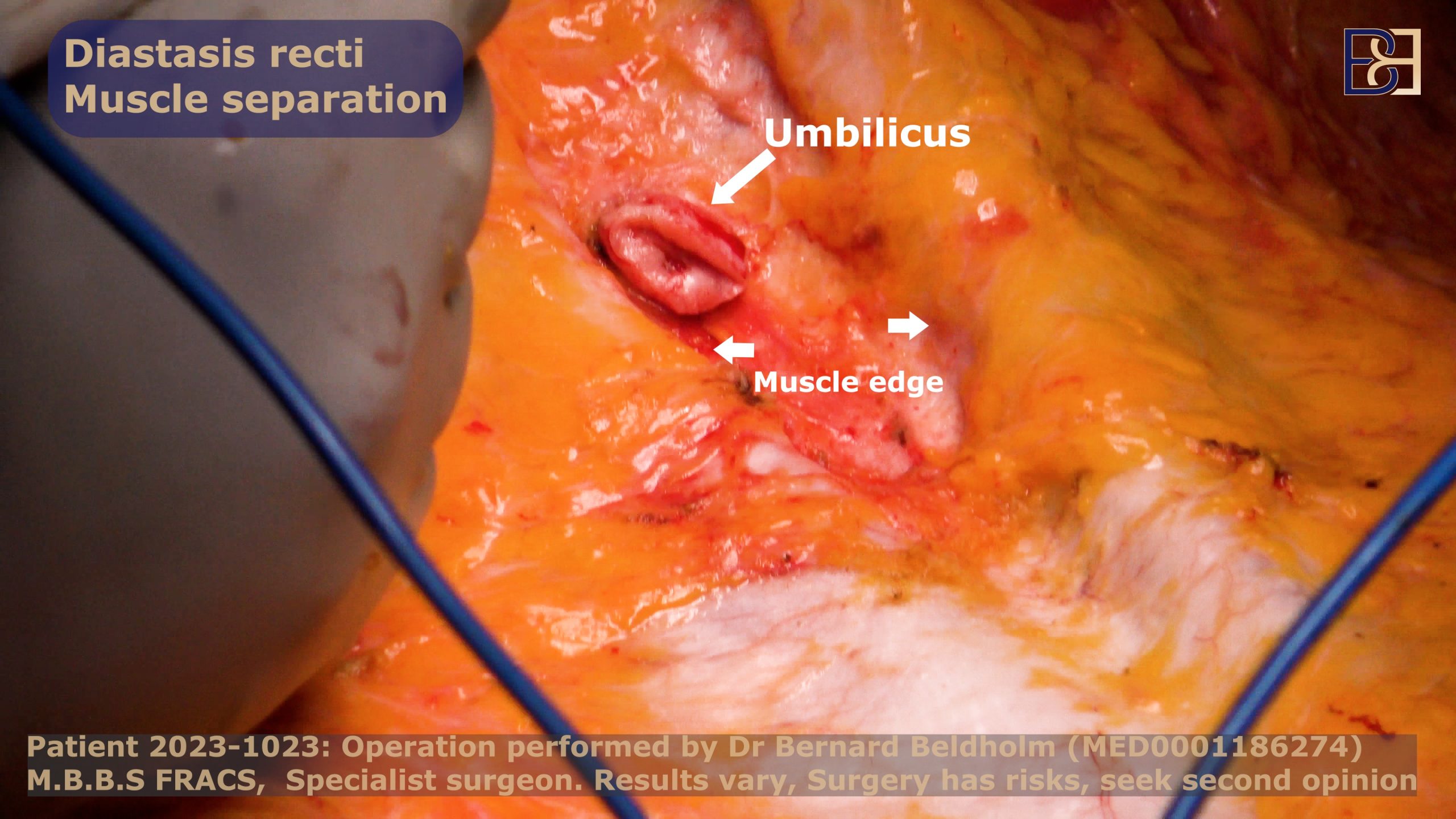
Additionally, I’ll repair separated abdominal muscles (diastasis recti), which occur when the abdominal muscles are stretched and separated, often as a result of pregnancy, weight gain, or significant physical strain. The procedure, which involves stitching the muscles back together and bringing them into their original alignment, helps with core function and strength. As a result, the patient will enjoy an elevated aesthetic appearance, better posture, reduced back pain, and increased core stability.
Incision Closure
After removing the excess fat and skin tissue and correcting diastasis recti, I close the incisions. I start with the deeper layers going upwards. I always use absorbable sutures to avoid future stitch sinuses or issues long-term. If necessary, I will place surgical drains to reduce fluid accumulation.
I always employ techniques that reduce the chance of using surgical drains and only use them when deemed necessary. Surgical drains help to drain excess lymphatic fluid that accumulate after surgery. This prevents lymphatic fluid accumulation, reducing the risk of haematoma and seroma formation. After this, I’ll then close the outer skin using surgical glue to ensure complete wound closure and reduce the risk of wound dehiscence.
Wound Dressing

The last step is dressing the wound using PICO negative pressure dressing.
Compression Garment
Additionally, I’ll place a compression garment on the incision site for support and recovery, which should be worn for 4 weeks full time followed by 2 weeks half time.
Recovery Process after FDL Abdominoplasty and Umbilical Hernia Repair
After the surgical procedure, I’ll provide you with guidelines to help you recover smoothly and reduce the risk of complications. Below are some of the items to take into account during recovery.
Hospital Stay
Fleur-de-Lis is an invasive procedure. Therefore, I’ll require you to stay in the hospital for a few days for observation. Most patients stay between two and three days. In addition to medical observation, the hospital stay ensures the effects of the anaesthesia have completely worn off, and the patient has gotten over the most difficult and painful period before being discharged to home care.
Regardless of the length of your hospital stay, you will not be able to drive home on your own and will therefore require someone to do this for you as well as care for you during the first few weeks. It’s important to make these arrangements well in advance of the actual procedure.
Pain Management

Expect to experience moderate to significant pain after the anaesthesia effects wear off. You may, in fact, feel somewhat intense pain for the first two days, which will be reduced with the use of prescription pain medications. It’s important to discuss your previous use of narcotic pain medications such as opioids and let me know your past tolerance. Likewise, it’s imperative that you are transparent with me about any previous long-term use or issues with addiction, as this may greatly impact your recovery and experience.
The good news is, the pain will subside gradually, and eventually dissipate completely.
Aftercare
Aftercare is an essential extension of your surgery, which is necessary for optimal healing and reducing the risk of irregular scarring and wound infection. This should include keeping the dressings clean and changing them regularly.
Aftercare tips:
- Avoid smoking (at least 6 weeks before and after surgery).
- Follow wound care instructions.
- Wear support garments.
- Avoid strain on the incision.
- Wear loose, comfortable clothing.
- Stay hydrated
- Protect the incision from excess sunlight.
- Attend all follow-up appointments.
- Maintain a stable weight.
- Nutrient-rich eating habits
- Take brief slow walks
Attending follow-up visits is very essential in recovery. I always advise my patients to attend the regular check-up appointments even when they feel fine. This is because it’s possible to develop serious complications which may go unnoticed by the untrained eye.
Book your appointment online now
Restriction on Activities
After surgery, you need to take some time off from work and make adjustments to your daily routine, including your normal activities such as pet and child care, exercise (including heavy lifting), driving, and housekeeping. Though you’ll need to avoid any activity that will exert pressure onto the wound, I recommend taking light walks around the house to assist with blood flow and reduce the risk of blood clots and deep-vein thrombosis.
Additionally, you should sleep on your back in an inclined position to reduce pressure on the incision. Also, you’ll need to avoid showers until the PICO dressing is removed, normally after a week or two.
Activity Modifications
- Driving
- Showering
- Child and pet care
- Working
- Sleeping
- Compression Garment
- PICO Dressing
Scar Management
Managing scars effectively is a vital part of the recovery process after surgery. The scars might take 1 to 2 years to fully fade, however this will vary among patients.
To elevate the appearance of these scars over time, one can use various techniques which include scar creams, silicone strips, and laser treatments. Additionally, I make incision scars as low as possible during the surgery and can be hidden with underwear, hence less visible.
Scar Creams: Using specialised scar creams and moisturisers helps keep the skin hydrated, which aids in natural healing.
Vitamin E: Fragrance-free vitamin E creams may be particularly beneficial for scar healing. They offer soothing properties that can help alleviate irritation while promoting skin recovery.
Silicone Strips: To maintain moisture around the wound and reduce tension on the scar, silicone strips can be used for 8 to 12 hours daily, starting four weeks post-surgery.
Massage: To aid with circulation and promote flexibility in the skin, a gentle massage of the scar tissue can help the overall healing process.
Sun Protection: It is important to avoid sun exposure for at least one year following abdominoplasty surgery. UV rays can darken and worsen scars. Applying a broad-spectrum sunscreen with an SPF of at least 30 will help protect the scar.
Additionally, wearing thicker fabrics and darker clothing can provide extra coverage from harmful UV rays.
Laser Treatments: This is another effective option for scar management. It works by targeting the scar tissue with focused light, promoting collagen remodelling and skin texture. This treatment can be particularly beneficial for reducing redness.
Potential Post-Surgical Complications
Every surgical procedure poses the risk of complications. Most complications are rare and treatable at an early stage. However, some complications can be serious if they go unnoticed. Therefore, I recommend that my patients contact me immediately if they feel any abnormality during recovery.
Below are some of the common potential complications after the combined surgery.
Wound Infection
Infection is a common complication after any surgery and can potentially result in additional complications and lead to unsatisfactory results. A study notes, “[I]nfections are the second most common complication following abdominoplasty, with an estimated incidence between 1% and 3.8%.”
Therefore, always keep the wound clean and follow the post-operative care guidelines I provide after surgery.
Haematoma and Seroma
Due to the procedure’s invasiveness, the tissues will be damaged. This can lead to accumulation of the lymphatic fluid around the surgical site. Where necessary, I use surgical drains to drain the fluid. However, I employ techniques that reduce the risk factors of hematoma and seroma formation.
I ensure to preserve the Scarpa fascia during surgery, which significantly reduces the risk of fluid formation. A study shows that, “[p]reservation of Scarpa’s fascia during an abdominoplasty procedure was associated with decreased seroma occurrence, reduced drain output, faster drain removal, and fewer infections.”
Hernia Recurrence
The main causes for hernia recurrence include infections, persistent cough, and strenuous activities prior to full recovery. Additionally, large-sized hernias pose a higher risk of recurrence.
Unsatisfactory and irregular Scarring
Scarring after surgery is normal, and the scar fades gradually. An FDL scar appears like an inverted T. However, there are instances where you may develop irregular scarring that is unpleasant and easily noticeable. This includes thick raised scars, scars that spread past the incision site, or scars with a different colour to the surrounding skin. The key to reducing unsatisfactory scarring is following the scar care routine. Patients should follow all the aftercare instructions provided to prevent complications.
Final Thoughts by Dr Beldholm

Massive weight loss and postpartum patients are at risk for developing an umbilical hernia. Combining hernia repair and Fleur-de-Lis abdominoplasty allows the patient to treat both the umbilical hernia and the loose skin resulting from massive weight loss at one time.
The combined procedure presents numerous benefits, including reduced downtime, reduced overall cost, and lower risks, among others.
Book a consultation today for a personalised consultation and customised surgical plan.
References
- Coste, A. H., Bamarni, S., & Leslie, S. W. (2024). Umbilical Hernia. In StatPearls. StatPearls Publishing.
- Köckerling, F., Brunner, W., Fortelny, R., Mayer, F., Adolf, D., Niebuhr, H., Lorenz, R., Reinpold, W., Zarras, K., & Weyhe, D. (2021). Treatment of small (< 2 cm) umbilical hernias: guidelines and current trends from the Herniamed Registry. Hernia : the journal of hernias and abdominal wall surgery, 25(3), 605–617.
- Appleby, P. W., Martin, T. A., & Hope, W. W. (2018). Umbilical Hernia Repair: Overview of Approaches and Review of Literature. The Surgical clinics of North America, 98(3), 561–576.
- Geoffrey E Hespe, David M Stepien, Rami D Sherif, Robert H Gilman, Umbilicoplasty in Abdominoplasty: Modifications for Improved Aesthetic Results, Aesthetic Surgery Journal Open Forum, Volume 3, Issue 3, September 2021, ojab025,
- Dogan T. (2010). Umbilicoplasty in abdominoplasty: a new approach. Annals of plastic surgery, 64(6), 718–721.
- Friedman, T., O’Brien Coon, D., Michaels V, J., Purnell, C., Hur, S., Harris, D. N., & Rubin, J. P. (2010). Fleur-de-Lis abdominoplasty: a safe alternative to traditional abdominoplasty for the massive weight loss patient. Plastic and reconstructive surgery, 125(5), 1525–1535.
- Vidal, P., Berner, J. E., & Will, P. A. (2017). Managing Complications in Abdominoplasty: A Literature Review. Archives of plastic surgery, 44(5), 457–468.
- van der Sluis, N., van Dongen, J. A., Caris, F. L. S., Wehrens, K. M. E., Carrara, M., & van der Lei, B. (2023). Does Scarpa’s Fascia Preservation in Abdominoplasty Reduce Seroma? A Systematic Review. Aesthetic surgery journal, 43(7), NP502–NP512.
- Mitchell, R. T., & Rubin, J. P. (2014). The Fleur-De-Lis abdominoplasty. Clinics in plastic surgery, 41(4), 673–680.
- Bruner, T. W., Salazar-Reyes, H., & Friedman, J. D. (2009). Umbilical hernia repair in conjunction with abdominoplasty: a surgical technique to maintain umbilical blood supply. Aesthetic surgery journal, 29(4), 333–334.
- McCarty, J. C., Lorenzi-Mendez, R., Fruge, S., Hamaguchi, R., & Colwell, A. S. (2023). Does Concomitant Umbilical Hernia Repair Increase the Risk of Complications in Abdominoplasty? A Propensity Score Matched Analysis. Aesthetic surgery journal, 43(9), 986–993.