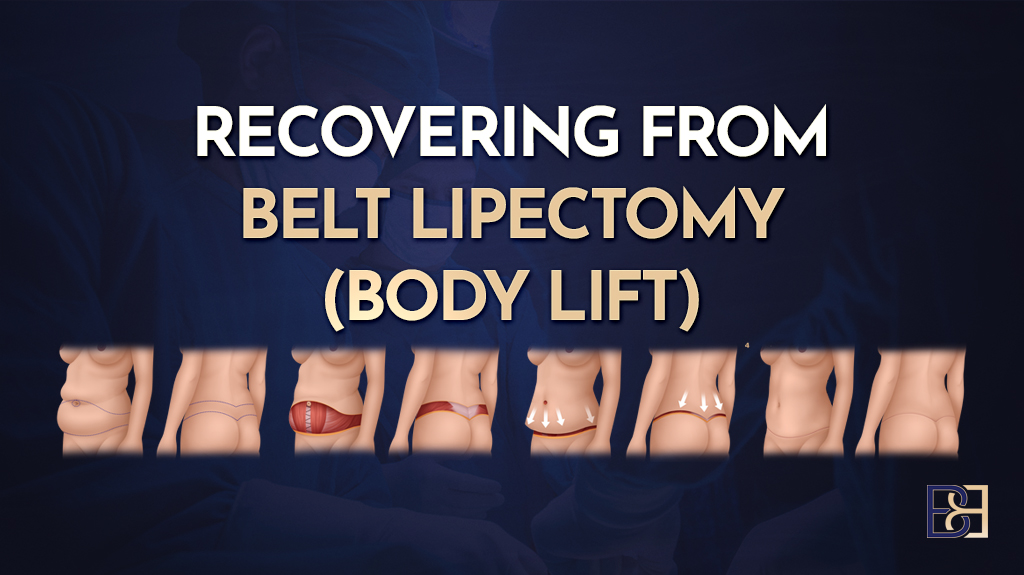
Recovering from belt lipectomy (lower body lift) surgery is a structured process that requires time, patience, and professional guidance. A belt lipectomy is a major surgical procedure that removes excess skin and fat from the lower body, including the abdomen, flanks, and back. This surgical procedure helps reshape the lower torso after massive weight loss or bariatric surgery (1,2).

During the operation, a continuous incision is made around the torso to allow for the comprehensive removal of excess tissue and to remove excess skin from the lower torso. Belt lipectomy is a type of plastic surgery and can be combined or staged with other procedures such as breast lift (mastopexy), breast reduction (Reduction Mammoplasty), thigh lift (thighplasty), tummy tuck (abdominoplasty), or fat grafting to achieve comprehensive body contouring.
At my clinic, recovery focuses on personalised support, mobility, and continuous monitoring to promote wound healing and achieve good long-term outcomes. Every stage—from the hospital stay to your return to normal activities—is carefully planned and supervised.
Preparing Your Home and Support
Arrange for someone to drive you home after surgery and assist you during the first two weeks, as you’ll need to avoid heavy lifting, strenuous exercise, and vigorous activity. Taking time off work and preparing your home for a comfortable recovery will help you focus on healing. Following your surgeon’s advice and making these preparations can help set the stage for a good recovery.
Preparation for the Procedure
Preparing for a belt lipectomy (lower body lift) starts several weeks before your scheduled surgery. Your surgeon will provide specific instructions, which may include stopping certain medications, such as blood thinners, and avoiding smoking to lower the risk of complications. Focusing on a healthy diet and regular, gentle exercise can help you reach optimal physical condition for your lower body.
GLP-1 Medications and Surgery: What You Need to Know
1. Continue Your GLP-1 Medication
- You usually do not need to stop GLP-1 drugs (such as semaglutide, liraglutide, dulaglutide, tirzepatide) before an operation.
- Stopping these may lead to poor blood sugar control or weight regain, which can delay recovery.
2. Risk During Anaesthesia
- These medicines slow the stomach from emptying, which can leave food or liquid in your stomach.
- That can increase the risk of aspiration (food or fluid entering the lungs) when you are asleep under anaesthetic.
- This risk is small but important to plan for.
3. How to Reduce Risk
Before your operation:
- Follow a clear-fluid diet for 24 hours (only water, broth, clear juices, black tea/coffee).
- Then fast for 6 hours before your scheduled surgery.
- If this diet wasn’t followed, the anaesthetic team may:
- Use an ultrasound to check if your stomach is empty,
- Give medicine (e.g., IV erythromycin) to help empty your stomach,
- Delay surgery if needed for safety.
4. On the Day of Surgery
- Your anaesthetist will ask if you are on GLP-1 medication and plan accordingly.
- You may be treated as if your stomach is “not empty” (similar to someone who has recently eaten), so they can take special airway precautions during anaesthesia.
5. After Surgery
- Restart your GLP-1 medication once you are eating and drinking again, as advised by your doctor.
- Continue your usual diabetic or weight-loss management plan.
The Day Before Surgery

The hospital will contact you the day before your operation to confirm your arrival time. Because belt lipectomy surgery is a long and complex operation, it is often scheduled later in the day, following a few shorter cases.
Day of Surgery
Arrival and Admission
You’ll arrive at Maitland Private Hospital and present to the theatre area on the ground floor. The theatre staff will admit you, confirm your details, and complete all required paperwork. Once checked in, you’ll be taken to the anaesthetic bay for preoperative preparation.
Anaesthetic Preparation and Surgical Markings
In the anaesthetic bay, your anaesthetist will review your medical history, discuss your anaesthetic plan, and insert one or more IV cannulae. I will meet with you to confirm the surgical plan, answer any final questions, and draw surgical markings while you are awake and standing.
Pre-Operative Warming and Anaesthesia
Before entering the operating theatre, you’ll be covered with a warming blanket to maintain temperature and reduce postoperative shivering. Once in theatre, you will receive TIVA (Total Intravenous Anaesthesia). After you are asleep, a urinary catheter (IDC) is inserted for fluid monitoring throughout the operation.
The Operation
The belt lipectomy (lower body lift) operation takes approximately six to eight hours, depending on the extent of excess skin removal and any additional contouring procedures. The surgical team works carefully to reshape the lower body while you are under constant monitoring.
Recovery and Ward Transfer
After the procedure, you’ll be taken to the recovery unit, where nurses monitor vital signs and manage pain medication. As it is a long surgery, you may wake up later in the day and remember little from recovery. I usually visit you to update you on how the surgery went. Once stable, you’ll be transferred to the ward, where nurses will continue to monitor your blood pressure, oxygen levels, and comfort throughout the night.
Hospital Stay and Early Recovery
Book your appointment online now
The belt lipectomy typically requires a three to five-day hospital stay. You’ll have a urinary catheter and surgical drains placed during surgery to remove excess fluid and aid healing. These are monitored and removed once drainage is minimal. Pain and blood pressure are managed closely, and you’ll be encouraged to move early with assistance to prevent blood clots (deep vein thrombosis). An incentive spirometer will be provided to encourage deep breathing and prevent chest infection.
Over the next few days, the nursing team will check your dressings and assist with mobility. Once you can walk comfortably and tolerate meals, you’ll be discharged home with a compression garment to reduce swelling and support underlying tissues as the healing process continues.
The First Few Weeks
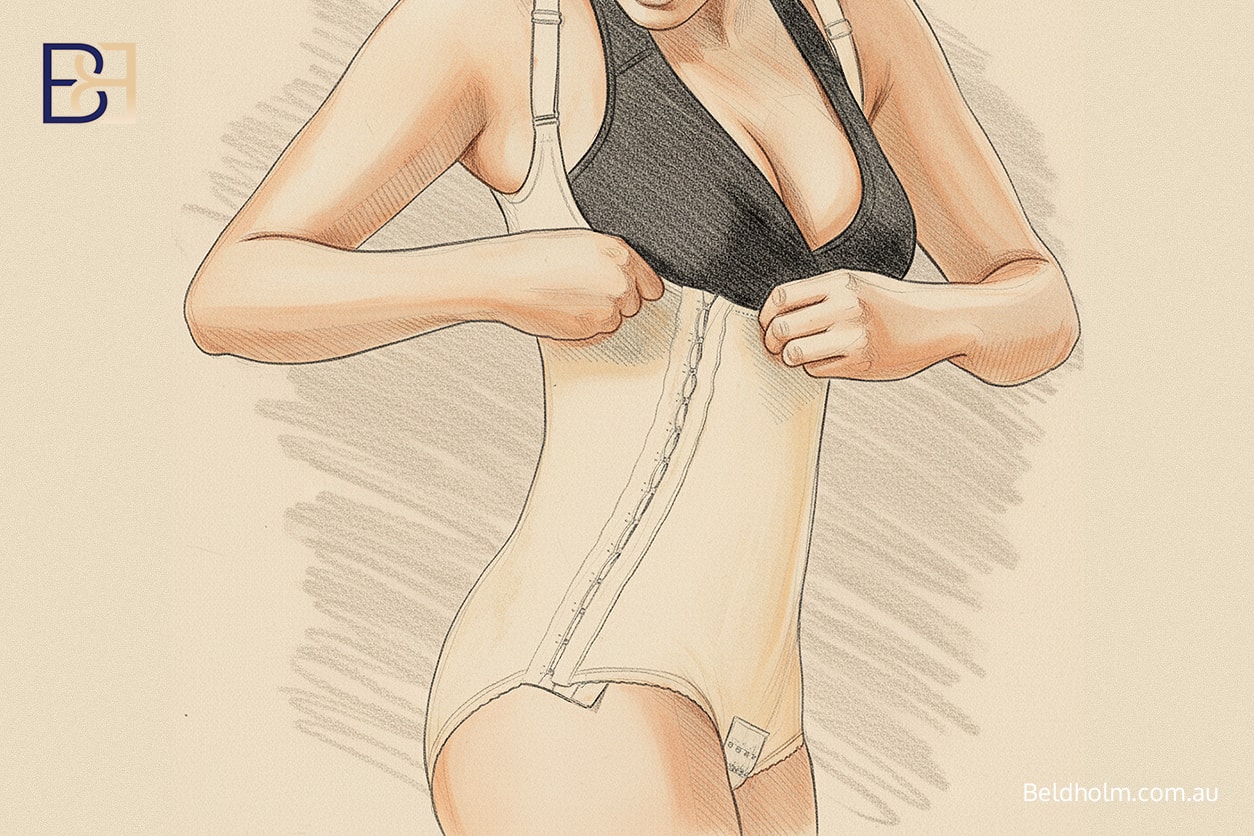
The first few weeks are critical for recovery. You’ll continue wearing your compression garment day and night, removing it only for showering. This helps control swelling, supports the healing process, and maintains stability of the underlying muscles (5).
Follow-up visits are conducted two to three times per week during this stage. My nurses perform sterile dressing changes, LED light therapy, and monitor wound separation or skin irritation. We also assess the compression garment for proper fit.
It’s important to avoid heavy lifting or strenuous exercise. Gentle walking promotes circulation and lowers the risk of blood clots. Pain is managed with prescribed medications, which are gradually reduced as you improve.
Weeks 4 to 8: Returning to Routine

Most patients notice better energy and reduced swelling by week four. As the swelling subsides, you may return to light activities. However, vigorous exercise should be delayed up to 6-8 weeks.
Ongoing scar management includes silicone taping and topical care to minimise scarring and protect the incision site from sun exposure. Patients are reviewed at 1, 3, 6, and 12 months to assess contour and healing progress (2,5).
A balanced diet rich in protein supports the healing process. Patients who have undergone bariatric surgery should continue working with their healthcare provider to monitor nutritional levels. Maintaining a stable weight and a healthy lifestyle helps preserve your final results.
Long-Term Recovery
After several weeks, the recovery period becomes easier. Most patients resume normal activities within two months. The final results continue to change over 6–12 months as the body settles and scars mature. Some visible scars may remain, but they are usually positioned low along the belt line (3,4).
Maintaining your healthy lifestyle, avoiding sudden weight gain, and following Dr Beldholm’s instructions will help sustain results and prevent the need for further surgery.
Healthy Lifestyle

Adopting a healthy lifestyle is essential for both preparing for and recovering from lower-body lift surgery. Achieving and maintaining a stable weight before your procedure can help minimise surgical risks and positively affect your final results. A balanced diet rich in nutrients supports the healing process, while regular, moderate exercise helps maintain muscle tone and reduces the risk of complications.
After your body lift (belt lipectomy), it’s important to continue these healthy habits. Avoiding excess weight gain can help prevent the return of sagging skin and preserve your new body contours. During the recovery period, follow Dr Beldholm’s guidance on activity levels to avoid overexertion and support proper healing. By committing to a healthy lifestyle, you can enjoy the benefits of your lower body lift for years to come and promote overall well-being.
Key Recovery Steps
_-_Infographic.jpg)
Follow-Up Care

Consistent follow-up care is a vital part of the recovery process after lower body lift (belt lipectomy) surgery. You will need to attend regular appointments with your surgeon to monitor your healing, remove sutures or drains, and address any concerns that may arise. Proper wound care and hygiene are essential during the recovery period to minimise the risk of infection and promote optimal healing.
Wearing compression garments as directed will help reduce swelling and support your lower body as it heals. Be attentive to any signs of complications, such as excessive bleeding, severe pain, or difficulty breathing, and contact Dr Beldholm immediately if these occur. By following Dr Beldholm’s instructions and keeping up with scheduled follow-up visits, you can help ensure a good recovery.
Summary
Recovering from a body lift (belt lipectomy) takes time and attention to detail. The recovery process focuses on rest, nutrition, and gradual movement. Most patients feel comfortable returning to normal routines after several weeks, though full results develop over many months.
References
- Aly AS et al. Truncal Body Contouring Surgery in the Massive Weight Loss Patient. Clin Plast Surg. 2004;31:611–624.
- El-Gharbawi AH et al. Postbariatric Abdominal Contouring: Technical Approach and Quality of Life. Plast Reconstr Surg. 2022;150:796–802.
- Richter DF, Stoff A. Circumferential Body Contouring: The Lower Body Lift. Clin Plast Surg. 2014;41:775–788.
- Carloni R et al. Circumferential Contouring of the Lower Trunk: Indications, Operative Techniques, and Outcomes—A Systematic Review. Aesth Plast Surg. 2016;40:652–668.
- van Huizum MA et al. Circular Belt Lipectomy: A Retrospective Follow-up Study. Ann Plast Surg. 2005;54:459–464.
Disclaimer
This content is considered Adult content. Individual results vary. All surgery carries risks. You should seek a second opinion before proceeding. The information provided is general and does not replace medical advice.
Dr Bernard Beldholm (MED0001186274) M.B.B.S B.Sc (Med) FRACS
Specialist General Surgeon – Surgery (General Surgery)
Body Contouring Surgery Clinic, Maitland Private Hospital