For many people who have achieved significant weight loss—whether through bariatric surgery such as a gastric bypass surgery or through consistent lifestyle change—the journey doesn’t end when the weight comes off. What remains is often excess skin and fat that doesn’t contract naturally.

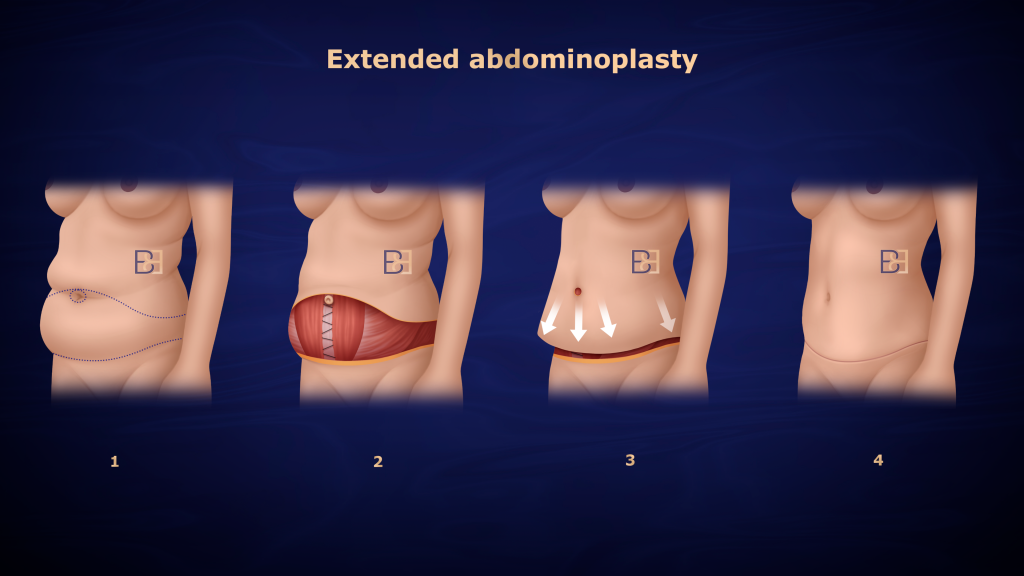
A full or extended abdominoplasty (tummy tuck surgery) is a surgical procedure designed to remove excess skin and tighten the abdominal muscles after massive weight loss, with the goal of treating function. However, surgery is only one step in the treatment process.
Recovering from abdominoplasty post weight loss requires time, careful follow-up, and structured clinical support. In my practice, operations are performed at Maitland Private Hospital, followed by coordinated post-operative care at my Maitland rooms. This guide explains what to expect during the recovery process, including routine care & follow-up timing.
The Setting: Surgery and Early Recovery
Your abdominoplasty procedure is performed at Maitland Private Hospital in the Hunter Valley, which provides 24-hour medical coverage and intensive care facilities.

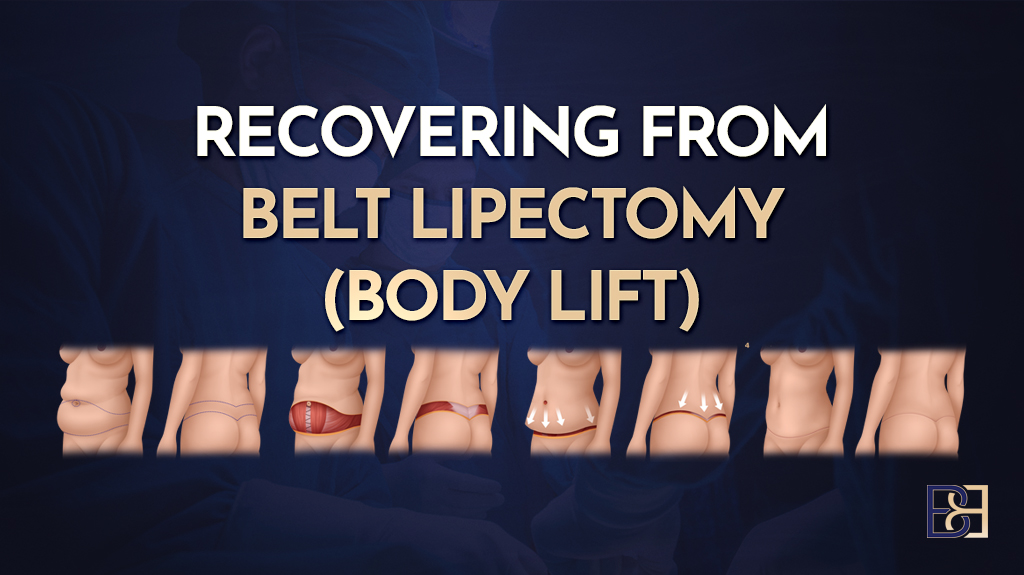
The operation involves removing excess skin and tightening underlying abdominal muscles that may have separated during weight gain. Advanced surgical techniques are used to support effective closure and minimise bleeding.
After surgery, you will wake wearing a compression garment that supports your abdominal area and helps control swelling. You may also have temporary surgical drains to prevent fluid accumulation.
Most patients stay two to four nights in hospital. During this period:
- You’ll receive appropriate pain management and antibiotics.
- Nursing staff and I will monitor for bleeding, blood clots, and signs of poor wound healing.
- Gentle walking is encouraged to reduce the risk of deep vein thrombosis (DVT).
- Instructions will be provided on wound care and garment management before discharge.
Your hospital recovery provides the foundation for predictable healing in the weeks ahead.
Week 1: Initial Recovery at Home
Once discharged, you’ll continue recovering at home. Many patients need temporary assistance with meals and mobility for the first few days. Remain slightly bent at the hips when walking or lying down to reduce tension on the incision. Continue wearing your compression garment full-time for the first four weeks after surgery. After this period, reduce wear to half-time for another two weeks—either during the day or overnight. I generally recommend wearing it during the day, as this is when patients most commonly experience swelling. The garment is essential for comfort and supports the healing process.
Follow-Up at My Practice
Your first follow-up appointment will depend on your discharge day, typically between day 5 and day 7 post-surgery. You will then be seen regularly in my practice for the first two weeks. During your initial visit:
- Dressings and drains (if present) are reviewed or removed.
- The incision is checked for skin irritation or wound complications.
- 830nm LED skin healing therapy may be provided to support circulation and healing.
- I use PICO dressings, which are negative pressure dressings designed to support wound care and healing. These are changed on day 7 post-surgery, and fresh Hypafix tape or PICO dressings are then applied by my nurse.

Patients who have undergone bariatric surgery or experienced massive weight loss often have thinner skin and reduced skin elasticity, making careful wound checks essential.
Weeks 2–3: Early Healing
During this period, swelling and tightness are common but should gradually normalise. There is usually significant swelling at this stage, and gentle lymphatic massage can be helpful. You will normally be able to stand up straight between 10 days and 2 weeks post-surgery. My nurse will instruct you on how to perform this massage at home. We also have a massage therapist available in the rooms who can assist with lymphatic drainage at an additional charge. Continue short walks daily and maintain good hydration.
- Continue wearing the compression garment day and night.
- Avoid lifting or stretching movements.
- Sleep with knees slightly bent to relieve incision tension.
Regular reviews continue at my Maitland practice, where we assess wound healing, adjust garments, and provide LED therapy. Most patients begin to move more comfortably by week three.
Skin Care
Mild skin irritation can occur as skin elasticity adjusts. It is also common to experience dry or flaky skin in the first few weeks after surgery. This dryness is related to swelling that stretches the skin early on. As the swelling resolves and the skin begins to return to normal, temporary dryness and flakiness can appear. I generally recommend using an unscented vitamin E cream or Bio-Oil to keep the skin moisturised and support comfort. Use gentle, fragrance-free products and avoid heat exposure.
Weeks 4–6: Building Mobility
Your regular check with Dr Beldholm will be at 4 weeks post-surgery. I will check the wound and progress at this stage, and this is when I will also take the first set of post-surgery images to document healing and results.

By the fourth week, swelling begins to lessen. You can increase light daily activities while continuing to avoid heavy lifting or core exercises to protect the abdominal muscles and internal repair.
Mild pulling sensations in the lower abdomen are normal. At this stage, many patients can return to light duties or sedentary work once they can move without discomfort.
Scar management may begin with silicone tape to minimise scarring.
Weeks 6–12: Functional Recovery
Recovery during this period focuses on regaining strength and tissue flexibility. Some mild firmness or numbness in the abdominal area may persist.
By week six, the compression garment may only be required during the day, though some patients continue wearing it longer for additional support. Light exercise such as walking or stationary cycling can be resumed if approved. Activities that strain the underlying abdominal muscles should still be avoided until cleared.
At the six-week review, I assess:
- Wound and scar progress.
- Persistent swelling or skin irritation.
- Early signs of poor wound healing.
Patients who live outside the Hunter Valley, such as in Sydney, Tamworth, or regional NSW, may have follow-up via telehealth after the initial in-person checks.
3–6 Months: Long-Term Healing
At this stage, most swelling has settled, and scars begin to soften. The abdominal skin and body contour continue to remodel. Gradual return to full activity, including resistance training, is possible after clearance.

Maintaining a stable weight is important to help prevent recurrent loose skin. Your final contour becomes clearer around 9–12 months post-surgery.
Tips for a good recovery Recovery
- Follow post-operative guidance – Attend all appointments and adhere to wound care instructions to reduce potential complications.
- Use your compression garment – Supports recovery and helps maintain contour.
- Stay active within limits – Gentle walking lowers the risk of deep vein thrombosis.
- Maintain weight stability – Avoid weight fluctuations to protect your results.
- Avoid nicotine products – These delay healing and increase risks of poor wound healing.
- Eat a protein-rich diet – Good nutrition aids recovery.
- Protect scars from sunlight – This prevents darkening or irritation.
Book your appointment online now
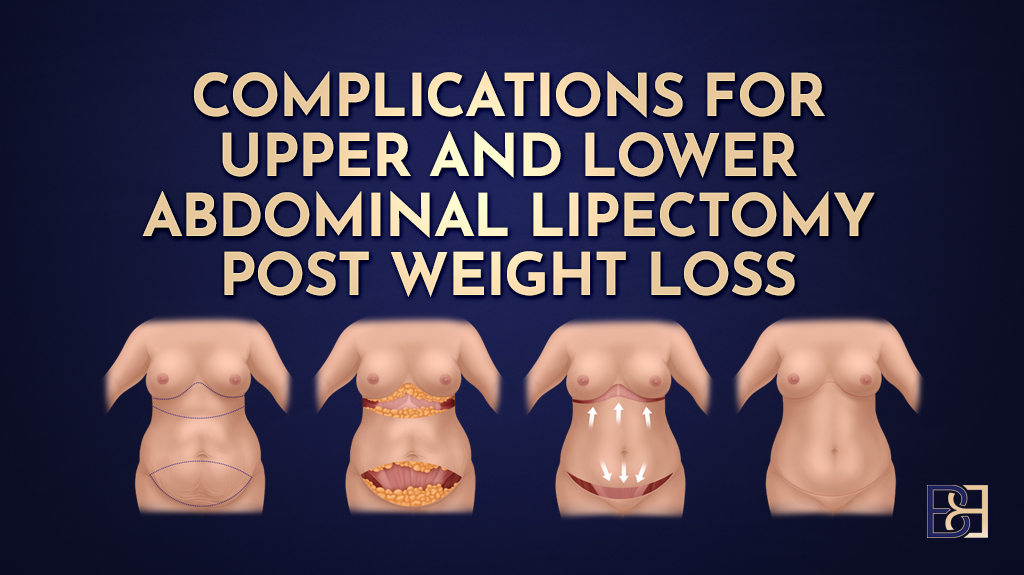
Monitoring for Complications
Early detection of complications are important. Contact my office or Maitland Private Hospital urgently if you experience:
- Increasing redness, swelling, or fever (infection)
- Sudden pain, bleeding, or fluid collection (hematoma/seroma)
- Shortness of breath or calf swelling (deep vein thrombosis)
- Any wound separation or drainage (poor wound healing)
Patients Travelling Long Distances
Many of my patients travel significant distances to have their surgery in Maitland — including those from Sydney, Coffs Harbour, Port Macquarie, Tamworth, Taree, and other areas along the north coast of NSW. We adapt our care routine slightly for these patients due to travel considerations.
The first two weeks after surgery are the most critical. Ideally, you should plan to stay in the Maitland area during this time so that we can monitor your recovery closely. After this period, your 4-week post-operative review can be conducted via Zoom. I also recommend scheduling a visit with your GP during this phase for additional local support.
I can review you remotely and provide e-scripts for antibiotics or pain relief if needed in the early post-operative period.
My standard review schedule is:
- 4 weeks post-surgery (in-person or Zoom)
- 3 months, 6 months, and 12 months post-surgery (some can be conducted remotely)
However, I recommend attending at least one in-person review at either 6 or 12 months for a complete clinical assessment and to take formal after-surgery images. Your before-and-after images will be provided as a Dropbox folder during your post-surgery period.
Structured Follow-Up
Recovery care in my practice follows a defined schedule:
- 2–3 nurse or doctor reviews each week during the first two weeks.
- Regular LED light therapy and wound checks.
- Surgeon reviews at 6 weeks, 3 months, 6 months, and 12 months.
- Telehealth for long-distance patients.
This structured approach ensures prompt management of any wound complications and supports a good recovery.
Long-Term Considerations
Weight and Exercise
Maintaining a healthy weight and performing low-impact exercise supports long-term outcomes. Discuss any major weight change plans or additional body contouring procedures with me before proceeding.
FAQs
How long does recovery take?
Most patients resume light activity after six weeks. Full recovery, including internal healing, may take 6–12 months.
What if I lose more weight after abdominoplasty?
Further weight reduction can result in new areas of loose skin. Aim to reach a target weight before surgery and maintain it afterward.
Can I sleep on my side after surgery?
Avoid side sleeping for the first few weeks. Sleep slightly bent with support pillows to protect the incision.
What are the best recovery practices?
Follow instructions, wear your compression garment, eat nutritiously, and attend all follow-ups.
Emotional and Physical Adjustment
Recovery following abdominoplasty post weight loss may bring temporary fatigue or emotional adjustment. This is normal and usually settles as strength returns. Focus on rest, gradual activity, and realistic expectations throughout the recovery process.
When to Contact Us
My team is available for any concerns. Please reach out if you experience new pain, fever, or signs of deep vein thrombosis. Prompt review helps identify problems early.
Conclusion by Dr Beldholm

Recovering from abdominoplasty post weight loss is a process that involves teamwork between you and my clinical team. Your operation is performed at Maitland Private Hospital, followed by structured clinical care in my Maitland practice.
Recovery occurs in stages — beginning with rest and wound management, then progressing to mobility and full functional recovery. Wearing your compression garment, maintaining a stable weight, and attending regular reviews are essential steps. The entire recovery process generally spans 6–12 months, during which swelling subsides & scars mature.
Each patient’s recovery is individual, and my team and I are here to support you through every phase — whether in person at Maitland or through remote reviews for those travelling from Sydney, the North Coast, or regional NSW.