Lower torso operations after massive weight loss are a common part of body contouring surgery. These operations include abdominoplasty (tummy tuck), extended abdominoplasty, Fleur-de-Lis abdominoplasty, and circumferential lipectomy (belt lipectomy). For post bariatric patients, these operations can treat excess skin that remains after significant weight loss.
This article provides an overview of complications from lower torso operations post weight loss. In Dr Bernard Beldholm’s experience as a Specialist Surgeon, patients who undergo these procedures may experience a range of complications. Understanding the potential issues helps patients prepare for discussions during consultations.
Why Complications Occur After Weight Loss Surgery
The Role of Skin Quality
After massive weight loss, skin often loses its elasticity. Surplus skin can make closure under tension more difficult, leading to wound problems. Poor elasticity also makes it harder for skin to heal smoothly. In Dr Beldholm’s practice, this is a common factor linked with wound-related complications for massive weight loss patients.

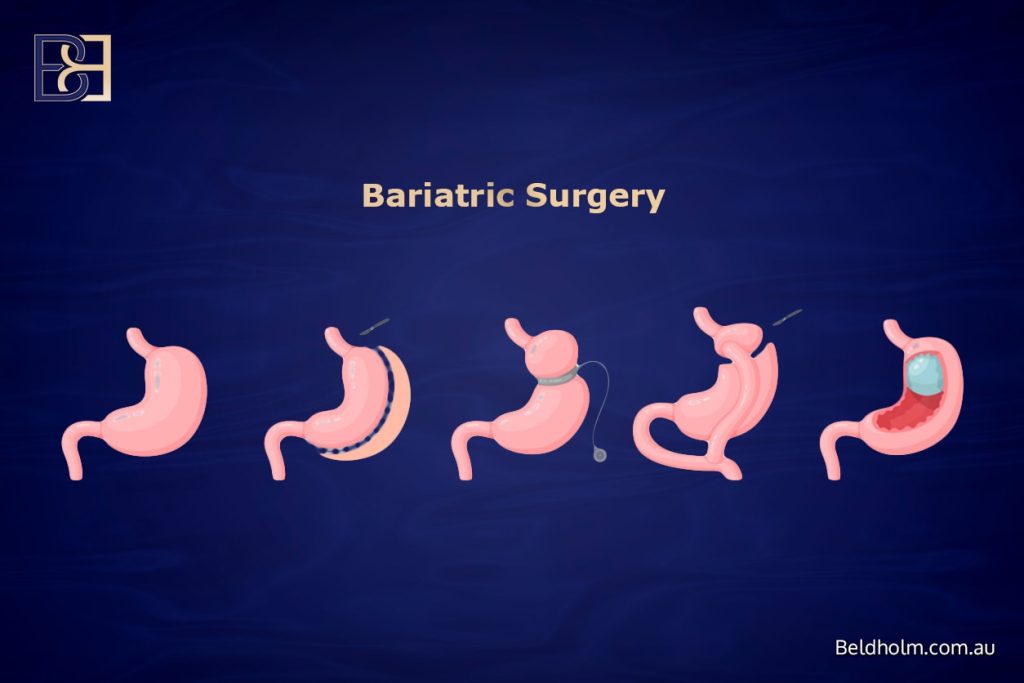
Nutrition After Bariatric Surgery
Patients who have had bariatric surgery such as gastric bypass surgery, sleeve gastrectomy, or gastric banding may develop nutritional deficiencies. Protein deficiency, vitamin deficiencies, and general nutritional imbalance impair wound healing. In Dr Beldholm’s experience, managing nutrition with the help of dietitians before surgery forms part of preparation. This is important since some bariatric surgery risks are directly related to poor nutrition and bariatric procedures.
Stable Weight Matters
Surgeons typically recommend that patients are at a stable weight for 6–12 months before surgery. In Dr Beldholm’s clinical practice, patients who have maintained stable weight often find that their recovery pathway is clearer compared to those with ongoing fluctuations. This requirement is particularly relevant for post bariatric surgery patients who may still be adjusting after their original weight loss surgery or other weight loss method.
General Complications of Surgery

These are complications that are common for most operations performed under a general anaesthetic.
Anaesthetic Risks
- Potential problems: Rarely, anaesthetic complications can include heart rhythm issues, blood pressure instability, or lung problems such as atelectasis.
- Treatment: These risks are managed with modern anaesthetic monitoring. In Dr Beldholm’s experience, working with experienced anaesthetists supports early detection and management when issues occur.
Blood Clots
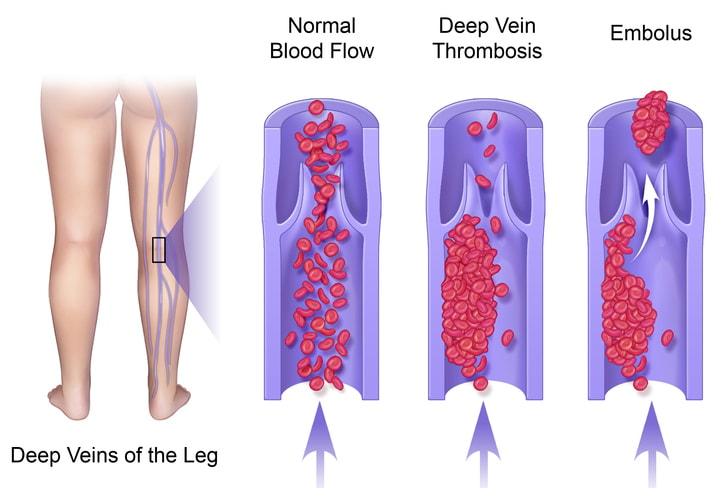
- Potential problems: Deep vein thrombosis (DVT) may occur in the legs after surgery due to immobility. Severe cases can lead to a pulmonary embolism.
- Treatment: Standard care can include compression stockings, anticoagulants, and early mobilisation. Dr Beldholm advises patients to walk early post-surgery as part of standard surgical treatment protocols.
Bleeding and Haematoma
- Potential problems: A haematoma can cause swelling, pain, and pressure on the skin.
- Treatment: Small haematomas may resolve naturally, while larger ones may need surgical drainage. In Dr Beldholm’s experience, monitoring patients post-operatively allows timely identification and treatment if this occurs.
Infection
- Potential problems: Infection can still occur despite antibiotics.
- Treatment: Minor infections are treated with oral antibiotics; severe cases may need intravenous therapy or surgical cleaning. Dr Beldholm and his team provide wound care guidance as part of routine follow-up.
Early Complications After Lower Torso Surgery

Seroma (Fluid Collection)
- Explanation: A seroma is a common issue after body contouring surgery due to large areas of tissue mobilisation.
- Treatment: Needle aspiration or drains may be needed. In Dr Beldholm’s practice, seromas are reviewed during follow-up and, when necessary, treated with drainage.
Wound Breakdown

- Explanation: Wound breakdown is one of the most common post operative complications for trunk operations after weight loss. Wound edges separate due to tension or poor blood supply.
- Treatment: Minor separations can be managed in-office; severe cases may need hospital readmission. Dr Beldholm often uses advanced dressings and negative pressure therapy as part of management, and in some cases further surgery may be required.
Necrosis (Skin Death)
- Explanation: Lifting and tightening the skin reduces its blood supply. If blood flow is inadequate, necrosis may occur within the first week.
- Treatment: Necrotic skin must be removed and debrided. In Dr Beldholm’s experience, many wounds are managed with VAC therapy and follow-up, though healing can take time and varies between patients. In some cases, further procedures may be necessary. In very rare situations, if the necrosis is extensive, skin grafting may be required.
Late Complications After Lower Torso Surgery

Scarring
- Explanation: All patients will have scars, which may stretch or thicken.
- Treatment: Scar care can include silicone, laser, or revision surgery if needed. Dr Beldholm uses silicone taping and LED therapy as part of his routine follow-up care protocols.
Nerve Changes
- Explanation: Numbness is common post-surgery. Rarely, nerve pain may persist.
- Treatment: Symptoms often change over time. Medications or physiotherapy may be used for persistent issues. Dr Beldholm observes that sensation may return gradually in many patients.
Complication Rates in Post Bariatric Patients
In Dr Beldholm’s experience, post bariatric patients who have undergone bariatric surgery face higher risks of wound healing problems and revision surgery compared to those without such a history. Research, including publications in the International Wound Journal, supports this observation and highlights the importance of thorough preoperative assessment. A higher complication rate is particularly noted in patients with morbid obesity or ongoing excess weight at the time of their surgical procedure.
Risk Factors That Increase Complications

Patient Factors
- High body mass index (BMI): Associated with higher rates of complications.
- Smoking: Linked with wound breakdown. Dr Beldholm requires patients to stop smoking at least 6 weeks before surgery.
- Diabetes/metabolic syndrome: Impairs healing.
- Older age: Associated with slower recovery.
Surgical Factors
- Extent of surgery: Larger procedures carry greater risk.
- Multiple procedures: Increase operative time.
- Excess tension: Raises risk of wound separation or necrosis.
Book your appointment online now
Complications by Specific Procedure
Standard Abdominoplasty
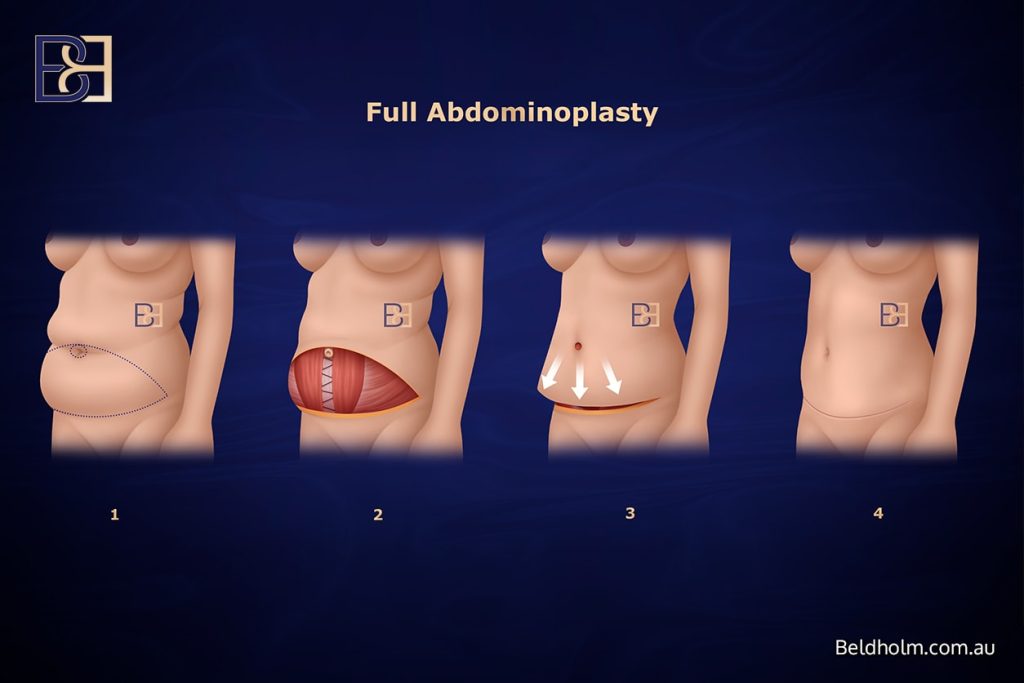
- Risks: Seroma, wound breakdown, infection.
- Treatment: Drainage, dressings, revision if needed. Dr Beldholm observes that smaller operations generally involve shorter recovery times, though postoperative complications can still occur.
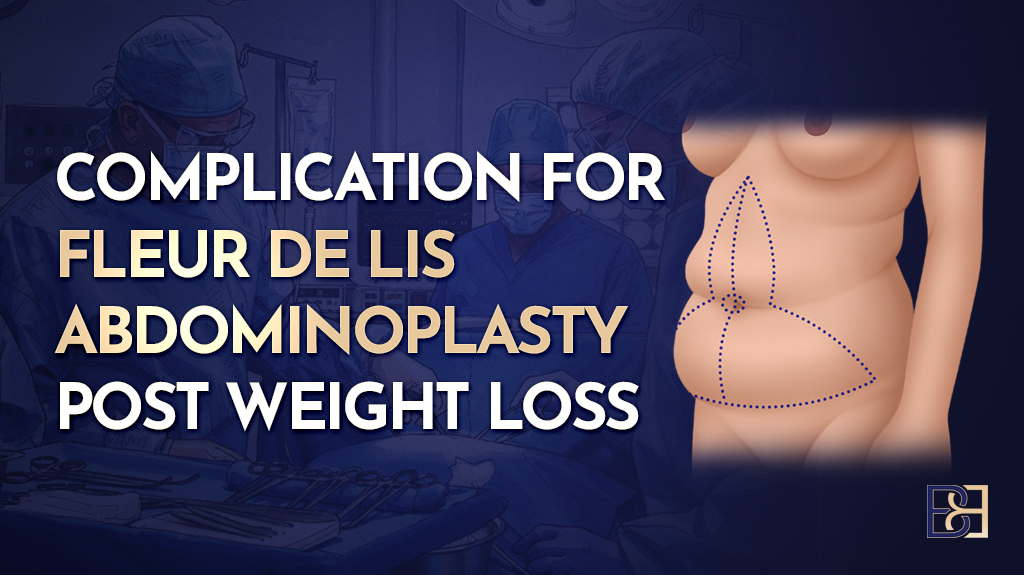
Fleur-de-Lis Abdominoplasty
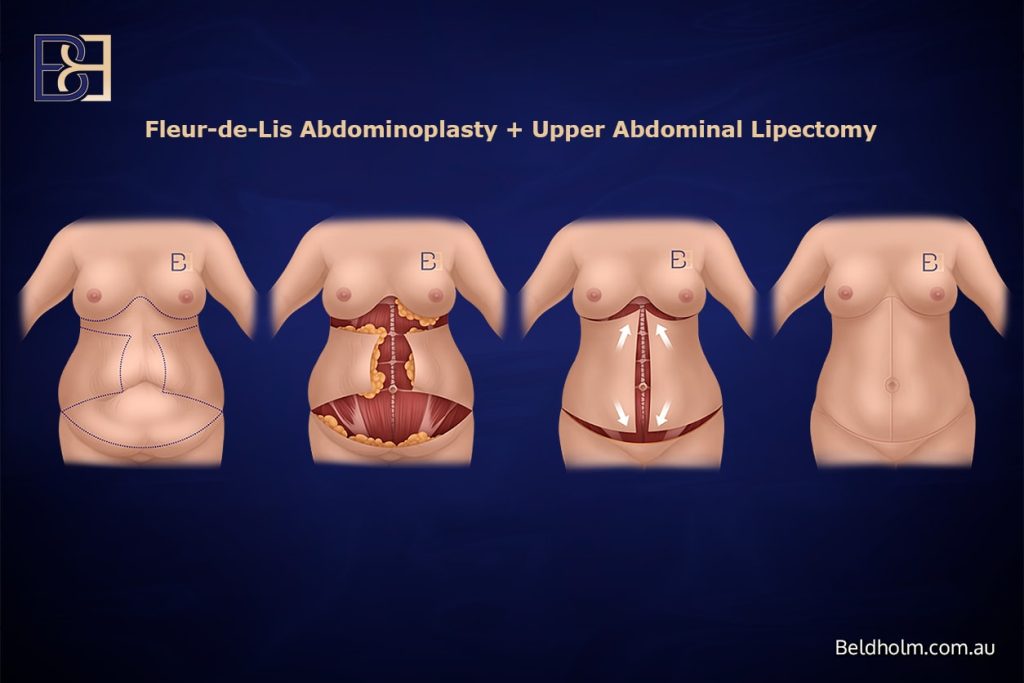
- Risks: Higher chance of wound breakdown.
- Treatment: Dressings or surgical revision. In Dr Beldholm’s practice, tension management is one aspect of the surgical technique used for this specific procedure.
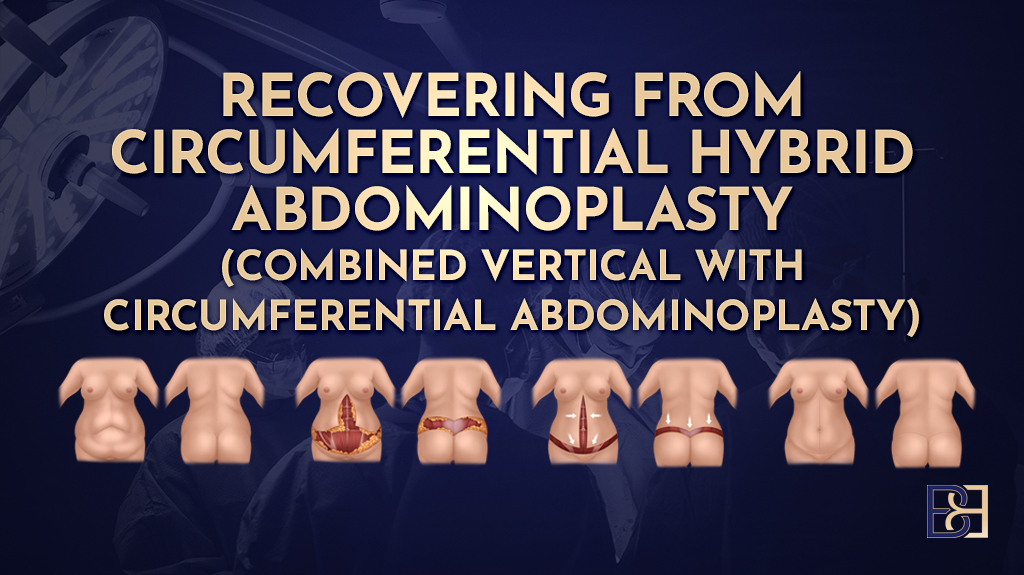
Belt Lipectomy (Lower Body Lift)
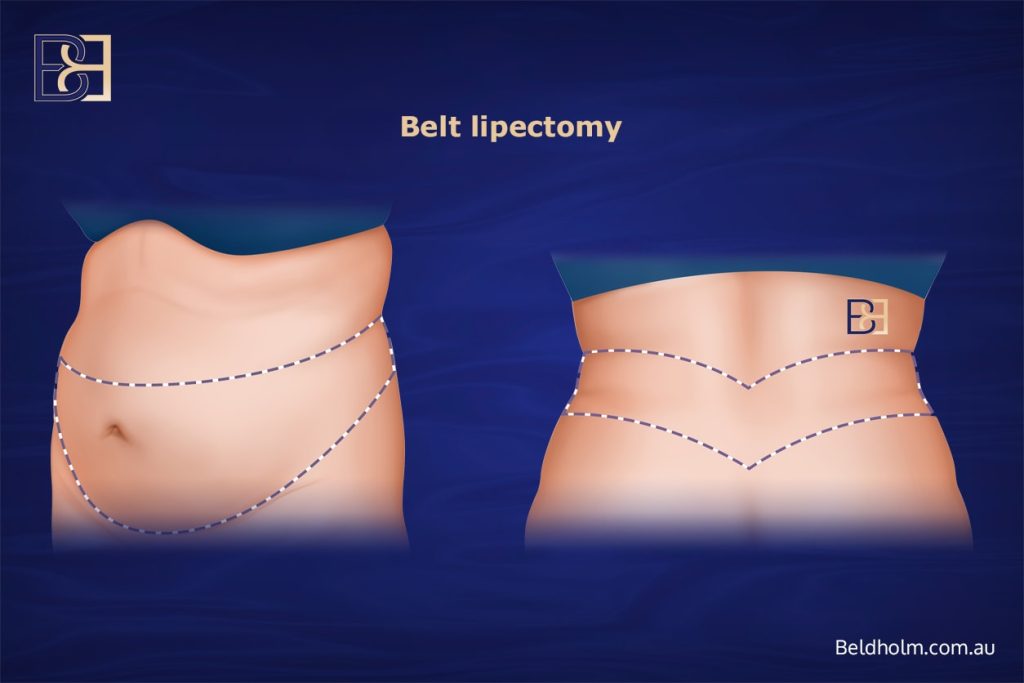
- Risks: 360-degree scar increases wound healing challenges.
- Treatment: Close monitoring, possible transfusion. Dr Beldholm explains this is one of the most extensive forms of lower body contouring surgery and requires careful patient selection.
Extended Abdominoplasty
- Risks: Similar to standard but covering more area.
- Treatment: Prolonged support and wound care. Dr Beldholm sometimes advises staging complex procedures depending on patient needs.
Complications Related to Bariatric Surgery History
Gastric Bypass Patients
- Risks: Nutritional deficiencies and bariatric surgery risks.
- Treatment: Supplements and monitoring. Dr Beldholm highlights the importance of managing nutrition before surgery.
Sleeve Gastrectomy Patients
- Risks: Less severe deficiencies but still relevant.
- Treatment: Ongoing nutritional support.
Gastric Banding Patients
- Risks: Band complications complicate anaesthesia.
- Treatment: Coordination with a bariatric surgeon. Dr Beldholm emphasises joint care planning for those with laparoscopic gastric banding history.
Duodenal Switch Patients
- Risks: Higher risk of nutritional problems and long-term bariatric surgery risks.
- Treatment: Requires lifelong follow-up and sometimes total parenteral nutrition. This weight loss surgery is less common in Australia but can be associated with complex complications.
Lifestyle and Long-Term Effects
Impact of Weight Gain After Surgery
Weight gain can stretch scars and undo results of body contouring. Dr Beldholm highlights the importance of maintaining stable weight and avoiding excess weight regain.
Ageing and Skin Quality
Natural ageing leads to reduced elasticity over time. In Dr Beldholm’s experience, some massive weight loss patients may undergo revision surgery many years later.
Exercise and Lifestyle Changes
Lifestyle changes such as regular exercise, balanced nutrition, and smoking cessation are important factors. Dr Beldholm encourages multidisciplinary care, including GP and dietitian involvement. A healthier lifestyle can support long-term recovery and reduce associated health issues such as joint pain or metabolic syndrome. Patients are advised that the risks involved in not following recommended care plans can include poorer scar healing or ongoing complications.
Questions Patients Commonly Ask
What Complications Are Commonly Reported After Post Bariatric Abdominoplasty?
- Wound breakdown.
- Seroma.
- Higher wound complication rate. In Dr Beldholm’s practice, these are the most frequent issues he manages in postbariatric patients.
What Are the Long-Term Effects of Weight Loss Surgery?
- Lifelong supplementation, risks of weight regain, and potential need for further operative management for complications such as strictures, hernias, or bowel obstruction. Some patients may also experience dumping syndrome, particularly after gastric bypass surgery. Dr Beldholm often counsels patients on long-term follow-up care.
Conclusion

Lower torso operations after weight loss are complex. While many patients choose to undergo reconstructive surgery, complications can occur. In Dr Bernard Beldholm’s experience, factors such as patient preparation, stable weight, and multidisciplinary care may influence the recovery process and the complications that can arise. Discussing these risks openly helps patients make informed choices and approach surgery with realistic expectations.