Written in 1946 by Dr. Jerome P. Webster, Mastectomy for Gynaecomastia Through a Semicircular Intra-Areolar Incision describes a forward-thinking surgical technique for treating gynaecomastia using a minimally invasive approach.
First introduced in 1934, the Webster procedure holds particular historical significance as one of the first surgical approaches specifically designed to treat male breast tissue enlargement. The procedure, involving a semicircular incision at the edge of the areola, allows for effective tissue removal with minimal scarring.

Book your appointment online now
While modern techniques have largely supplanted this method, the procedure has several notable advantages, especially within the context of its time, and has been recognised for its effectiveness, outcomes, and low complication rates.

Key Aspects of the Webster Technique
- Precise incision placement to reduce visible scarring.
- Dissection under the areola to remove excess breast tissue while leaving enough fat for a smooth chest contour.
- Meticulous suturing to maintain aesthetic outcomes and symmetry.
- Avoids adhesion of the nipple to underlying muscle.

Three Classes Of Permanent Benign Hypertrophy
Presented before The New York Surgical Society and The Philadelphia Academy of Surgery, February 14, 1945, this study, which involved 32 breasts, does not deal with the surgical treatment of the malignant type of male breast hypertrophy, nor does it involve pubescent cases which generally resolve on their own.
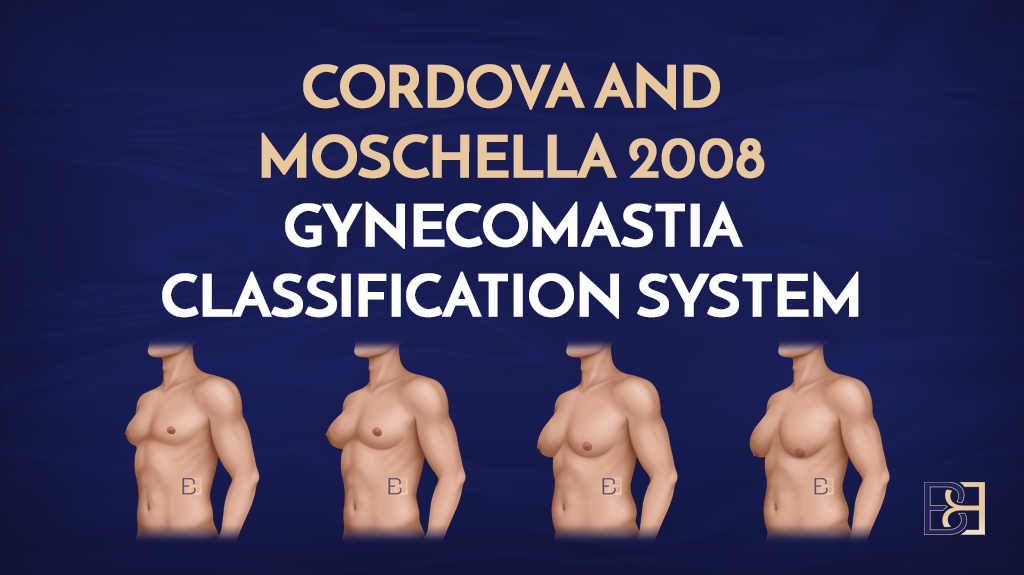
According to Webster, there are three classes of permanent or persistent benign hypertrophy for which surgical intervention may be the advised protocol.
1. Periductal Connective Tissue Hypertrophy without Adipose Tissue
Characteristics
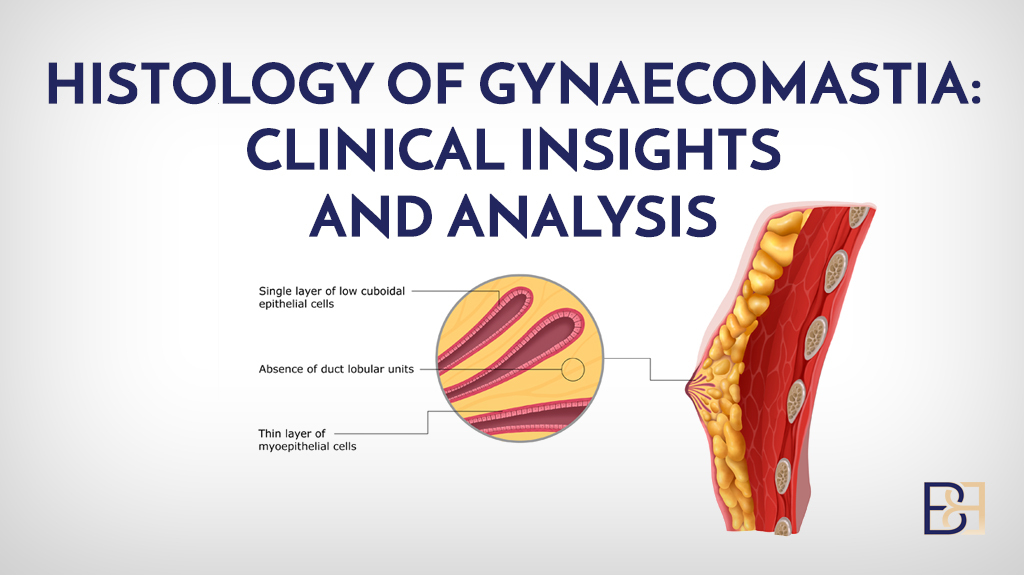
- No male breast cancer evident.
- Mammary gland is hypertrophied, forming a firm discrete nodule beneath the areola and adjacent tissue .
- A well-defined white fibrous tissue is also present, while microscopic examination reveals elongated ducts and ductules surrounded by a mass of connective tissue and a complete absence of adipose tissue within the nodule.
- The intra-ductal epithelium may be hypertrophied forming projections into the lumens of the ducts.
- No true acini are found as in the female mammary gland, although terminal Ductules may exhibit similarities.
- Onset commonly occurs during puberty.
Treatment
The treatment for periductal connective tissue hypertrophy without adipose tissue, according to Webster, involves a surgical approach tailored to the dense fibrous tissue concentrated around the ducts. The key aspects of his treatment approach are:
The treatment for periductal connective tissue hypertrophy without adipose tissue, according to Webster, involves a surgical approach tailored to treat the dense fibrous tissue concentrated around the ducts. The key aspects of his treatment approach are:
1. Direct Excision
- Webster advocated for a subareolar incision through the areola to access and excise the periductal fibrous tissue.
- An approach that targets the hypertrophic connective tissue while preserving the surrounding normal tissues, direct excision ensures a flat chest contour.
2. Preservation of Normal Tissue
- Webster’s technique emphasizes removing only the hypertrophic tissue without disturbing the nipples, skin, or areolar structures to ensure aesthetic integrity.
3. Minimal Liposuction
- In an absence of adipose tissue, suction-assisted lipectomy (liposuction) is typically unnecessary. However, Webster allowed for adjunctive liposuction if minor fatty tissue is present.
4. Focus on Functional and Aesthetic Outcomes
- For aesthetic outcomes, the focus was achieving a masculine chest contour while minimising scarring and disruption to the nipple-areola complex.
2. Increase in Hypertrophy and Adipose Tissue
Characteristics
- Connective tissue elements exist only in small amounts in the region beneath the areola with the remainder of excess tissue composed of adipose tissue.
- The body appears feminine (eunuchoid) or masculine.
- Genitalia may be normal or underdeveloped.
- One or both breasts may be involved.
- Commonly occurs at puberty.
Treatment
For cases involving increased hypertrophy of periductal connective tissue along with adipose tissue, Webster’s approach combines techniques to both fibrous and fatty components. Here’s an overview:
1. Combination of Excision and Liposuction (Suction-assisted lipectomy)
- A subareolar incision directly removes the dense, hypertrophic connective tissue surrounding the ducts, an essential step because liposuction alone cannot adequately treat the fibrous component. Suction-assisted lipectomy (liposuction) is employed to remove excess tissue and contour the chest.
2. Contouring
- Liposuction (Suction-assisted lipectomy) is extended to the surrounding chest areas to eliminate any uneven fat distribution and ensure a smooth transition. This step minimises the risk of postoperative complications.
3. Skin Retraction and Redundancy
- In cases significant tissue removal is needed, Webster emphasised evaluating the skin’s elasticity to predict its ability to retract.
- Skin tightening procedures or direct excision of redundant skin may be performed to achieve optimal results when necessary.
4. Aesthetics
- Special care is taken to maintain the integrity of the nipple-areola complex and ensure minimal scarring.
5. Postoperative Care
- Compression garments are used to support skin retraction, reduce swelling, and promote proper healing. Webster stressed the importance of this step for maintaining contour and minimising complications.
Combining excision and liposuction (Suction-assisted lipectomy), Webster focused on both hypertrophic connective tissue and adipose tissue, ensuring functional and aesthetic outcomes tailored to the patient’s body shape. This treatment remains a cornerstone for treating complex gynecomastia cases.
3. Adipose Tissue Hypertrophy
Characteristics
- Increase in size of the breast is due entirely to excessive adipose tissue with no mammary gland hypertrophy.
- The body is generally underdeveloped and may be of the Froehlich type. Also known as adiposogenital dystrophy, Froehlich syndrome is a group of endocrine abnormalities believed to result from damage to the hypothalamus, a part of the brain that links the nervous system to the endocrine system via the pituitary gland.
- Bi-lateral.
- Appears in the first decade of life, but usually does not cause issues until the age of puberty.
- No nodule palpable beneath the areola.
Treatments
Webster’s treatment for adipose tissue hypertrophy (predominantly involving excess fat without significant glandular or fibrous tissue enlargement) primarily focused on removing the fat deposits and contouring the chest. Here’s a breakdown of his approach:
1. Suction-assisted liposuction as the Primary Treatment
Suction-assisted liposuction is the first-line treatment for adipose tissue hypertrophy because the primary issue is fat accumulation, liposuction effectively reduces volume and reshapes the chest without the need for extensive glandular excision.
- Cannula Insertion: Small incisions made in inconspicuous areas
- Fat Removal: Suction used to selectively remove excess fat while preserving overall chest structure.
2. Assessment of Skin Elasticity
- Skin Retraction: If the skin has good elasticity, it can naturally contract after suction-assisted lipectomy (liposuction), negating the need for additional skin-tightening procedures.
- Management of Loose Skin: In cases of poor skin elasticity (e.g., older patients or significant weight loss), Webster noted the potential need for additional procedures to treat skin redundancy, though these were less common in adipose-dominant cases.
3. Minimal Incisions and Aesthetic Considerations
- Scarring: The suction-assisted lipectomy (liposuction) incisions are minimal and strategically placed to ensure they are as inconspicuous as possible.
- Contour Smoothness: Careful liposuction technique is employed to avoid irregularities and achieve a symmetric, masculine chest contour.
- Rare Need for Glandular Excision
- Since adipose tissue hypertrophy lacks significant glandular or fibrous tissue, glandular excision is typically unnecessary unless there is a mixed presentation.
4. Postoperative Care
- Compression Garments: These are essential to support skin retraction, reduce swelling, and aid in recovery.
- Follow-Up: Monitoring for any residual irregularities or asymmetry, which could be corrected with touch-up suction-assisted lipectomy (liposuction).
Surgical Indications
In the early 20th century, widely accepted treatments for gynaecomastia included radiotherapy, endocrine therapy, and surgery. According to Webster, radiotherapy and other non-surgical techniques were ineffective, however, with surgical removal of the excess tissue offering the best method for correcting enlarged male breasts.
1. Malignancy
Though quite rare, mammary hypertrophy carcinoma (male breast cancer) develops late in life.
2. Breast Pain Relief
Pain or tenderness was a complaint in some of the men. Though painful gynecomastia was reported as a complaint, however, the true cause was the unwelcome shape of the breast.
3. Preventing Psychic Trauma
The psychic trauma caused by enlarged breast development and a feminine appearance due to oestrogen levels is the main reason for surgical interference for non-malignant gynaecomastia.
Subjected to bullying, men with enlarged breast tissue whose bare chest is exposed on a regular basis— such as in the military, locker rooms, and pools—may exhibit changes in behaviour patterns— such as hesitating to undress for the gym or the beach and refrain from swimming or wearing thin clothing, may exhibit psychotic disturbances.

Surgical Techniques
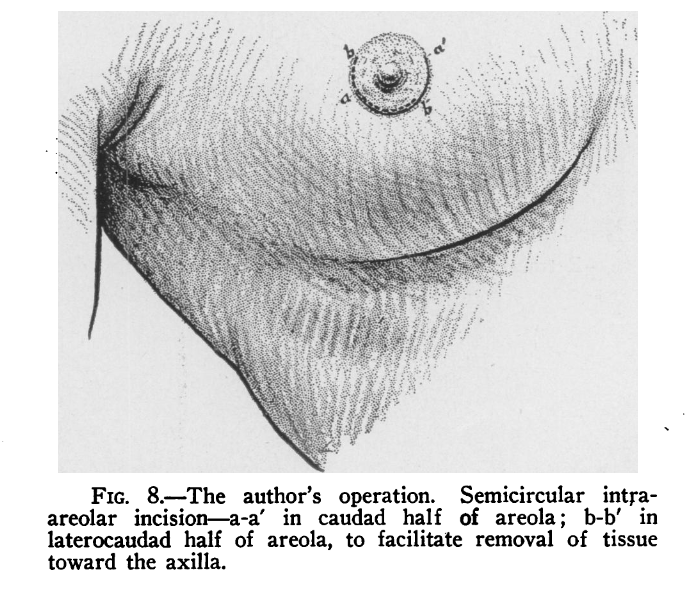
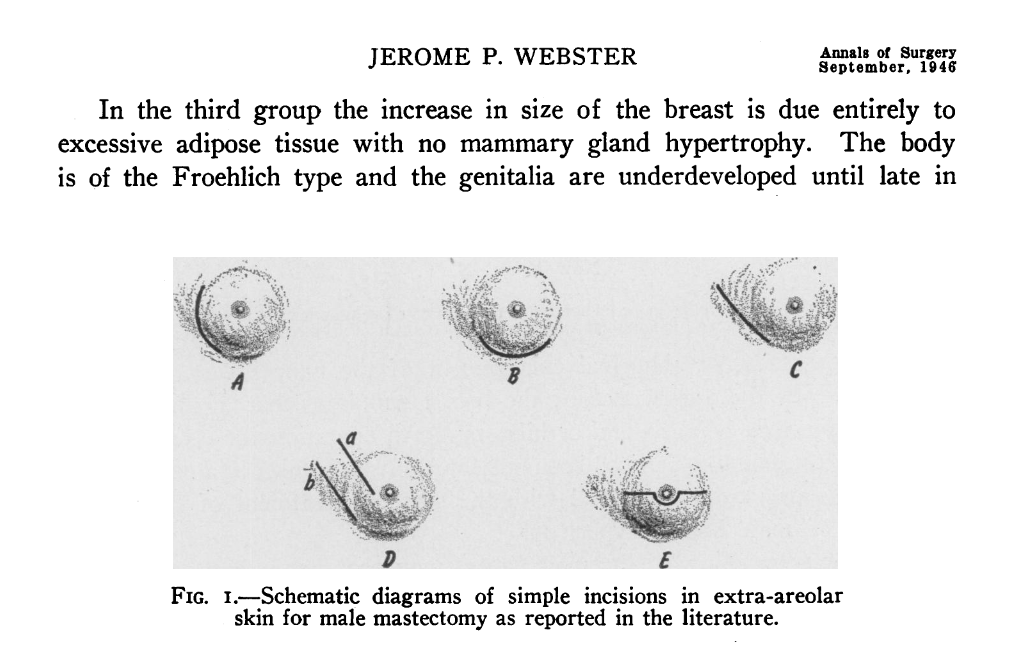
There was a time when surgeons advocated removing the entire areola together as there is no indication that the resulting scars cause as much embarrassment as the original condition, especially when the scars are bilateral and symmetrical. As such, this operation which was devised by the author and first performed in 1934, resulted in questionable outcomes.
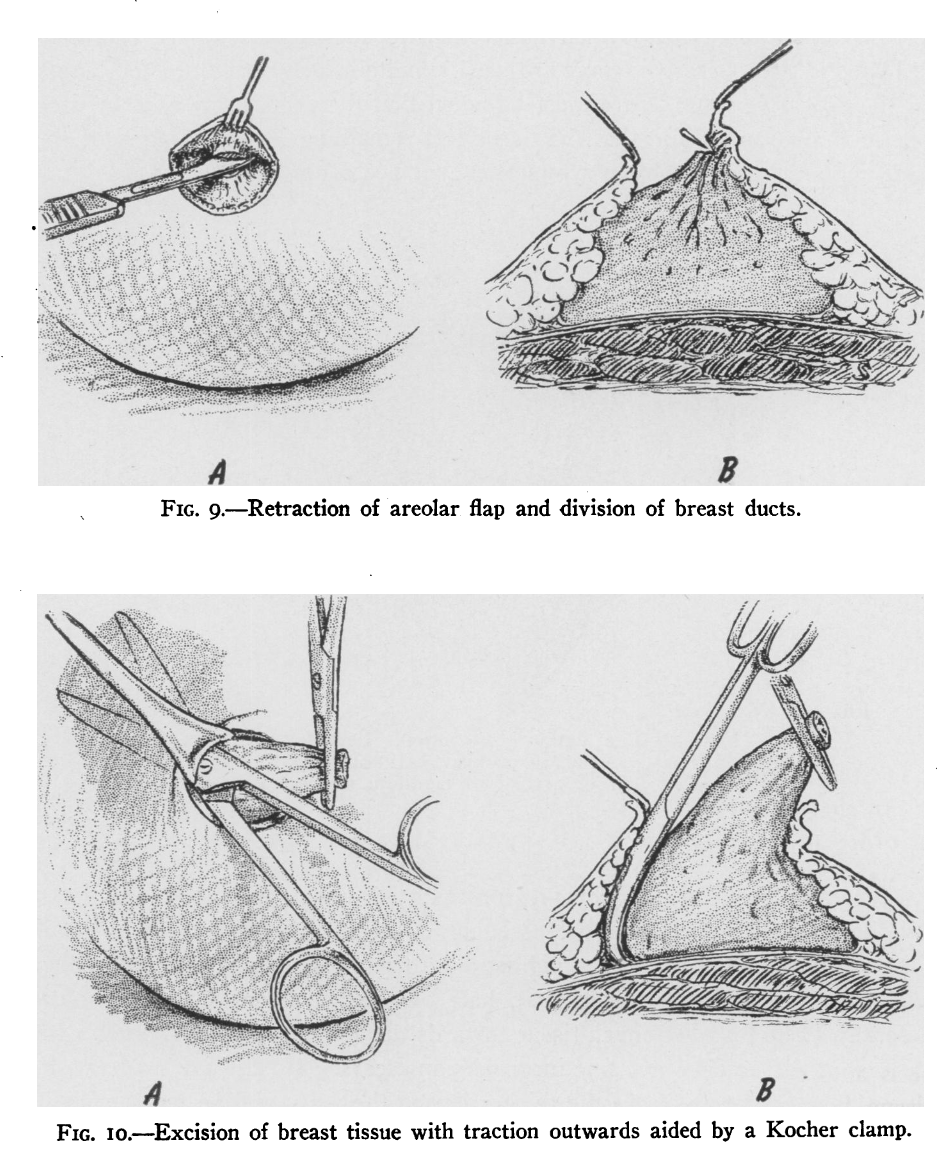
Using general anesthesia, the surgery proceeded as follows:
- Regarding the mammary appearance, the removal of the excess tissue through a single submammary lunar incision was the preferred treatment.
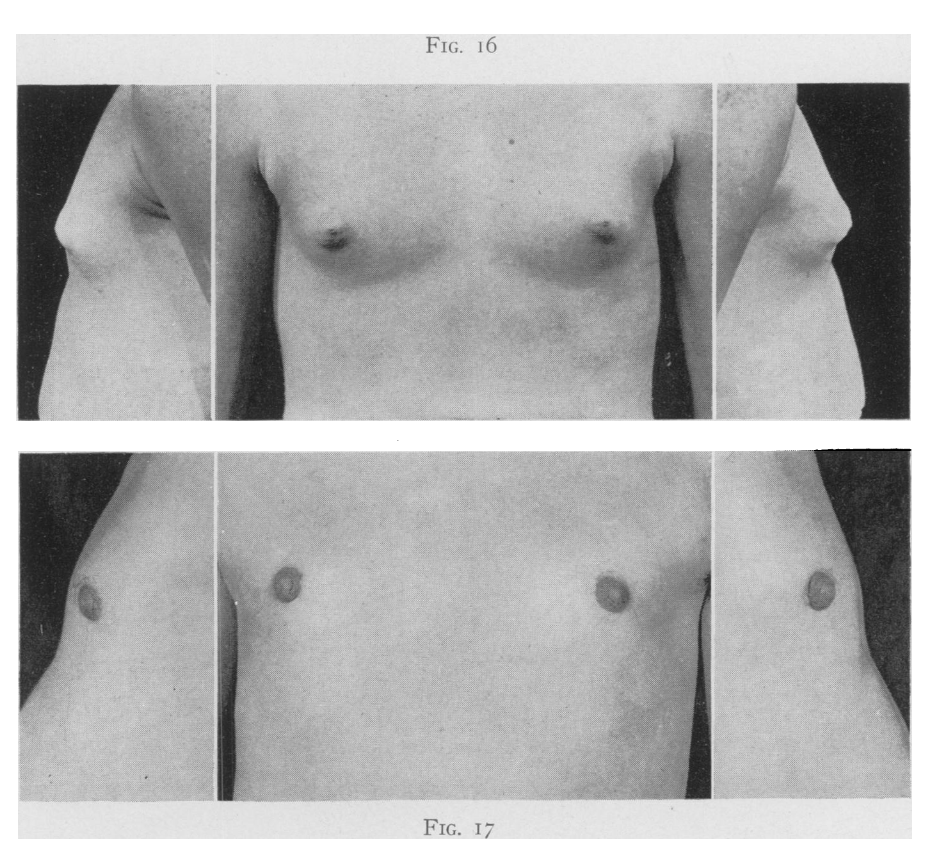
- If the condition was bilateral, two operative teams were used simultaneously to reduce the length of the operative time. Care was taken so the procedures used by each operator were similar and that the tissue remaining on each side was symmetric.
- The areola was distended by pressure exerted downwards about the breast by the encircling hands of the assistant.
- A semicircular incision was made just within the margin of the pigmented area of the areola. It may either extend over the lower, or caudad, half of the areola, or be placed more laterally, leaving fine inconspicuous scars.
- Dissection beneath the areola with division of the ducts was made early to facilitate operation.
- Excision was aided by traction upwards with Kocher clamps on the divided ductal stump or on the mass of tissue that has been freed.
- Enough adipose tissue was left to be drawn together eventually beneath the nipple.
- If the areola was small in comparison with the amount of tissue to be re-moved through the incision, the tissue was halved or quartered and removed in separate portions.
- Sufficient fat was left over the pectoral fascia to obtain a smooth, even surface when the remaining tissues are replaced.
- Reduction of the adipose tissue was sufficient to overcome the similarity to the female breast, with the remaining amount remaining proportionate to the rest of the body.
Advantages of Mastectomy through a Semicircular Intra-areolar Incision for the Correction of Gynecomastia
1. Direct Glandular Removal
- The Webster procedure is effective at removing dense glandular tissue, which can be challenging to eliminate with suction-assisted lipectomy (liposuction) alone.
- This makes it particularly useful for patients with firm, fibrous gynecomastia that is resistant to other interventions.
2. Straight forward
- The procedure involves an inframammary incision, allowing direct access to the glandular tissue.
- To treat gynaecomastia, this straightforward approach requires fewer specialised tools compared to modern suction-assisted lipectomy (liposuction) techniques, making it accessible for surgeons.
3. Predictable
- Since the tissue is excised directly, the procedure provides a high degree of certainty in removing the gland, reducing the risk of recurrence due to incomplete tissue removal.
4. Practical
- Unlike modern methods that often involve ultrasound-or laser-assisted liposuction, the Webster procedure does not require advanced or expensive equipment, making it more practical in resource-limited settings.
5. Foundation for Modern Techniques
- The Webster procedure served as an essential starting point for understanding gynaecomastia and refining surgical techniques. Many modern approaches, which combine glandular excision and suction-assisted lipectomy (liposuction), are built on principles first formalised by Webster.
6. Reliable for Severe Cases
- In cases of severe gynaecomastia with significant glandular tissue, the direct excision offered by the Webster procedure ensures comprehensive removal, which might not be achievable with suction-assisted lipectomy (liposuction) alone.
7. Low Risk of Incomplete Gland Removal
- Modern suction-assisted lipectomy (liposuction)-based techniques sometimes fail to remove all glandular tissue, requiring follow-up surgery. The Webster procedure eliminates this concern by prioritising complete excision.
While the Webster procedure is largely outdated today due to advancements in minimally invasive techniques that cause scarring and recovery time, it remains a significant milestone in the surgical treatment of gynaecomastia.
Disadvantages of Mastectomy through a Semicircular Intra-areolar Incision for the Correction of Gynaecomastia
The Webster procedure, developed in 1946 by Frederick S. Webster, is one of the earliest techniques for gynaecomastia. While it has historical significance, it is not commonly used in modern practice due to several disadvantages compared to contemporary surgical techniques. Disadvantages include:
1. Scarring
- The procedure involves an inframammary incision (under the breast), which can result in visible and sometimes prominent scars, particularly if the patient has poor wound healing or keloid tendencies.
2. Limited Ability
- The Webster procedure is primarily designed to remove glandular tissue but does not remove fatty tissue or skin excess effectively.
- It lacks the precision of modern suction-assisted lipectomy (liposuction)-assisted techniques for contouring the chest.
3. Skin Laxity
- In cases of significant gynaecomastia or when there is excess skin, the Webster procedure does not result in skin tightening, often leaving the chest with residual flaps or irregularity.
4. Higher Risk of Asymmetry
- The direct excision method may lead to uneven tissue removal, resulting in chest asymmetry or unnatural contours.
5. Limited Application
- This technique is less effective for pseudo-gynaecomastia (enlarged male breasts caused by fat rather than glandular tissue), which is common in many patients.
6. Prolonged Recovery Time
- The surgery and the recovery period can be more invasive compared to minimally invasive methods that include suction-assisted lipectomy (liposuction).
7. Potential for Nipple Distortion
- Improper technique or excessive tissue removal could lead to complications like nipple flattening, inversion, or poor positioning.
8. Outdated Technique
- Modern procedures such as ultrasound-assisted suction-assisted lipectomy (liposuction), VASER liposuction, or a combination of suction-assisted lipectomy (liposuction) with glandular excision are preferred. These newer methods minimise scarring and often have shorter recovery times.
Final Thoughts

In the context of modern medicine, Webster’s treatments for gynaecomastia remain foundational and continue to influence current surgical practices. His emphasis on tailoring interventions to the underlying tissue composition provides a structured approach that balances aesthetic outcomes with patient-specific anatomy. Advances in suction-assisted lipectomy (liposuction) techniques, such as ultrasonic or power-assisted suction-assisted lipectomy (liposuction), have further precision and efficacy, especially in cases involving adipose tissue hypertrophy.
Webster’s legacy lies in his commitment to both functional correction and aesthetic refinement, making his techniques as relevant today as they were when first introduced, particularly in the era of patient-centered, minimally invasive approaches to gynaecomastia treatment.
While the Webster procedure for gynaecomastia holds historical importance as one of the first surgical approaches designed to specifically correct male breast tissue enlargement due to chronic gynaecomastia, pubertal gynaecomastia, or idiopathic gynaecomastia (of unclear cause), and played an essential role in the evolution of gynaecomastia surgery, advancements in treatments and technology have made it largely obsolete.
While modern techniques have largely supplanted Webster, the procedures do have notable advantages, especially within the context of the time period.
Since the normal appearance of the male pectoral region is achieved with almost no evidence of operative interference, the patient can return to normal activities and expose his chest without the fear of ridicule.
To learn more about the surgery, whether you’re a candidate for the procedure, and the overall process in my article, Essential Insights on Gynaecomastia Surgery for Men, or book a consultation to learn if gynaecomastia surgery is right for you.
After performing a thorough examination and asking questions about your goals, concerns, expectations, and medical history, I will tell you about the benefits, risks, downtime, costs associated with the surgery, and answer all of your questions. This informative consultation takes place in a discreet, professional office environment, convenient to most localities.
Resources
- https://academic.oup.com/asj/article-abstract/38/1/58/4110193?redirectedFrom=fulltext
- https://docslib.org/doc/7572473/mastectomy-for-gynecomastia-through-a-semicircular-intra-areolar-incision-jerome-p
- Menville, J. G.: Gynaecomastia. Arch. Surg., 26, 1054-1083, 1933.
- Lisser, H.: Adrenal Cortical Tumor. Endocrinology, 20, 567-569, 1936.
- Zondek, Hermann: The Diseases of the Endocrine Glands. London, Edward Arnold & Co., 1935.
- Lewin, Michael L.: Gynaecomastia: The Hypertrophy of the Male Breast. J. Clin.
Endocrinol., 1, 511-514, 1941. - Schonfeld, William A.: Management of Male Pubescence. J. A. M. A., 121, 177-
182, 1943. - Schonfeld, William A.: Primary and Secondary Sexual Characteristics: Study of Their Development in Males from Birth through Maturity:
- With Biometric Study
- of Penis and Testes. Am. J. Dis. Child., 65, 535-549, 1943.
- Buirge, Raymond E., Samuels, Leo T., and McCartney, J. S.: Treatment of Puber-
- tal Bilateral Gynecomastia. Surgery, 17, 397-403, 1945.
- Menville, J. G.: X-Ray Treatment in Gynaecomastia. Radiology, 18, 295-301, 1932.
- Adair, F. E.: A Consideration of Recent Additions to Clinical and Experimental Knowledge of Breast Conditions. West. J. Surg., 48, 645-661, 1940.
- 10 Wernicke, H. O.: Gynecomastia. Surgery, 5, 217-225, 1939.
” Klinefelter, Harry F., Jr., Reifenstein, Edward C., Jr., and Albright, Fuller: Syndrome Characterized by Gynaecomastia, Aspermatogenesis without A-Lydigism, and Increased Excretion of Follicle-stimulating Hormone. J. Clin. Endocrinol., 2, 615-627, 1942. - Sullivan, J. M., and Munslow, R. A.: Gynaecomastia. A Study of Five Cases.
- J. A. M. A., 118, 1443-1444, 1942.
- ” Gooel, Elmer F.: Gynaecomastia. Surgery, 15, 938-943, 1944.
- Bannayan, G. ,A. and Hajdu, S. .I Gynaecomastia: Clin- icopathologic study of 351 cases. Am. .J Clin. Pathol. 57: 431, 1972.
- Jackson, .A W., Muldal, S,. Ockey, .C H,. and O’Connor, P. .J Carcinoma of male breast in association with the Klinefelter syndrome. B.r Med. .J 1: 223, 1965.
- Beckenstein, M. S,. Windle, B. H,. and Stroup, .R .T Anatomical parameters for nipple position and areo- lar diameter in males. An. Plast. Surg. 36: 3, 1996.
- Murphy, .T P,. Ehrlichman, R. J.,and Seckel, B. R. Nipple placement in simple mastectomy with free nipple grafting for severe gynecomastia. Plast. Reconstr. Surg. 94: 818, 1994.
- Gingrass, M. K,. and Kenkel, .J M. Comparing ultra- sound-assisted lipoplasty with suction-assisted lipo- plasty. Clin. Plast. Surg. 26: 283, 1999.
- Bowers, S. P,. Pearlman, N. W,. Meintyre, R. C., Jr., Fin- layson, C. ,A. and Huerd, S. Cost-effective manage- ment of gynecomastia. Am. J. Surg. 176: 638, 1998.
- Beck, W,. and Stubbe, P. Endocrinological studies of the hypothalamo-pituitary gonadal axis during dana- zol treatment in pubertal boys with marked gyneco- mastia. Horm. Metabol. Res. 14: 653, 1982.
- McGrath, M. H. Gynaecomastia. In M. .J Jurkiewicz, S. J. Mathes, .T J. Krizek, and .S Ariyan (Eds.), Plastic Sur- geyr: Principles and Practice. St. Louis: Mosby, 1990.
- Webster, J. P. Mastectomy for gynaecomastia through a semi-circular intra-areolar incision. An. Surg. 124: 57, 1946.
- Barsky, .A,.J Kahn, S,. and Simon, B. E. Principles and Practice of Plastic Surgery, 2nd Ed. New York: McGraw Hill, 1964.
- Pitanguy, I. Transareolar incision for gynaecomastia. Plast. Reconstr. Surg. 38: 414, 1966.
- Letterman, G,. and Schurter, M. The surgical correc- tion of gynaecomastia. Am. Surg: 35: 322, 1969.
- Letterman, G,. and Schurter, M. Surgical correction of massive gynaecomastia. Plast. Reconstr. Surg. 49: 259, 1972.
- Pers, M,. and Bretteville-Jensen, G. Reduction mamma-plasty based on the vertical vascular bipedicle and “tennis ball” assembly. Scand. .J Plast. Reconstr. Surg. 6: 61, 1972.
- Simon, B. E., Hoffman, S,. and Kahn, .S Classification and surgical correction of gynaecomastia. Plast. Recon- str. Surg. 51: 48, 1973.
- Eade, G. G. The radial incision for gynaecomastia exci-sions. Plast. Reconstr. Surg. 54: 495, 1974.
- Wray, .R ,C. J,.r Hoopes, .J ,E. and Davis, G. M. Cor- rection of extreme gynaecomastia. Br. .J Plast. Surg. 27: 39, 1974.
- Balch, .C R. Atransaxillary incision for gynaecomastia. Plast. Reconstr. Surg. 61: 13, 1978.
- Artz, ,S. and Lehman, .J ,A. J.r Surgical correction of massive gynaecomastia. Arch. Surg. 113: 199, 1978.
- Davidson, B. .A Concentric circle operation for massive gynaecomastia to excise the redundant skin. Plast. R-e constr. Surg. 63: 350, 1979.
- Fara, M,. and Hrivnakova, .J Reduction mammaplasty in serious gynaecomastias using a single superiorly based flap. Acat Chir. Plast. 23: 159, 1981.
- Huang, T. ,T. Hidalgo, J.,E. and Lewis, .S R. Acircum- areolar approach in surgical management of gynaecomastia. Plast. Reconstr. Surg. 69: 35, 1982.
- Plast. Surg. 16: 220, 1986. Samdal, F., Kleppe, G,. Amland, P. F,. and Abyholm, F. Surgical treatment of gynaecomastia. Scand. .J Plast. Reconstr. Surg. Hand Surg. 28: 123, 1994.
- Abramo, .A.C Axilary approach for gynaecomastia -liposuction. Aesthetic Plast. Surg. 18: 265, 1994.
- Smoot, E. C. Eccentric skin resection and purse-string closure for skin reduction with mastectomy for gynaecomastia. An. Plast. Surg. 41: 378, 1998.
- Ohyama, T., Takada, ,A. Fujikawa, M,. and Hosokawa, K Endoscope-assisted transaxillary removal of glandular tissue in gynaecomastia. An. Plast. Sugr. 40: 62, 1998.
- Botta, S. .A Alternatives for the surgical correction of severe gynaecomastia. Aesthetic Plast. Surg. 2: 65, 1998.
- Chiu, D. ,T. and Siegel, H. W. The pinwheel technique: An adjunct to the periareolar approach ingynecomastia resection. An. Plast. Surg. 42: 465, 1999.
- Gingrass, M. K,. and Shermak, M. .A The treatment of gynaecomastia with ultrasound-assisted lipoplasty. Perspect. Plast. Surg. 12: 101, 1999.