Indications: Experiencing loose skin after losing 30 kilograms, leading to functional issues such as skin fold rashes in the lower abdomen.
Approach: VASER Assisted Fleur de lis Abdominoplasty Surgery

Book your appointment online now
Because this patient experienced extensive loose skin and fat after losing weight due to gastric bypass surgery, a standard abdominoplasty surgery would not be sufficient for removing the excessive redundant skin on her abdomen. Therefore, I recommended that a Suction-Assisted Lipectomy Fleur-De-Lis Abdominoplasty Surgery be the most appropriate solution. The patient was also experiencing abdominal muscle separation (diastasis rectus abdominis), requiring an additional step to fix diastasis recti. Diastasis recti occurs when the connective tissue in the abdominal area stretches, often due to significant weight fluctuations. Diastasis recti abdominis is a condition where the core muscles in the abdomen separate, leading to complications like urinary incontinence and lower back pain.
For a deeper dive into diastasis recti repair, see my article: Everything You Need to Know about Diastasis Recti.
Though most patients experience sustainable weight loss, a reduced body mass index, and a smaller waist circumference after bariatric surgical procedures, many continue to carry stubborn weight and experience obesity related conditions despite lifestyle changes, exercise, healthy eating habits, and reduced food intake.
Suction-Assisted Lipectomy Fleur-De-Lis Abdominoplasty Surgery is a type of surgery that combines liposuction treatment with FDL, a specialised type of surgery that targets redundant skin and fat on both the upper and lower abdominal areas.
Named after the shape of a water lily, the fleur-de-lis portion of the surgical procedure involves two intersecting incisions that leave a T-shaped scar.

Suction-Assisted Lipectomy with VASER is a modern technique that uses sound waves to liquefy the fat before it is removed from the body.
In this article, I will review the entire operation, outline the steps involved for each portion of the surgery, and provide visual aids to provide an up-close-and-personal and fully transparent explanation of the surgical procedure I will utilise. Though some of the images are extremely vivid, I believe it’s best to educate my patients as thoroughly as possible before embarking on such an exciting, extensive, and life-changing journey.
Prepare the Patient/Markings in Anaesthetic Bay
Before heading into surgery, I will meet you in the anaesthetic bay to go over any last-minute questions.
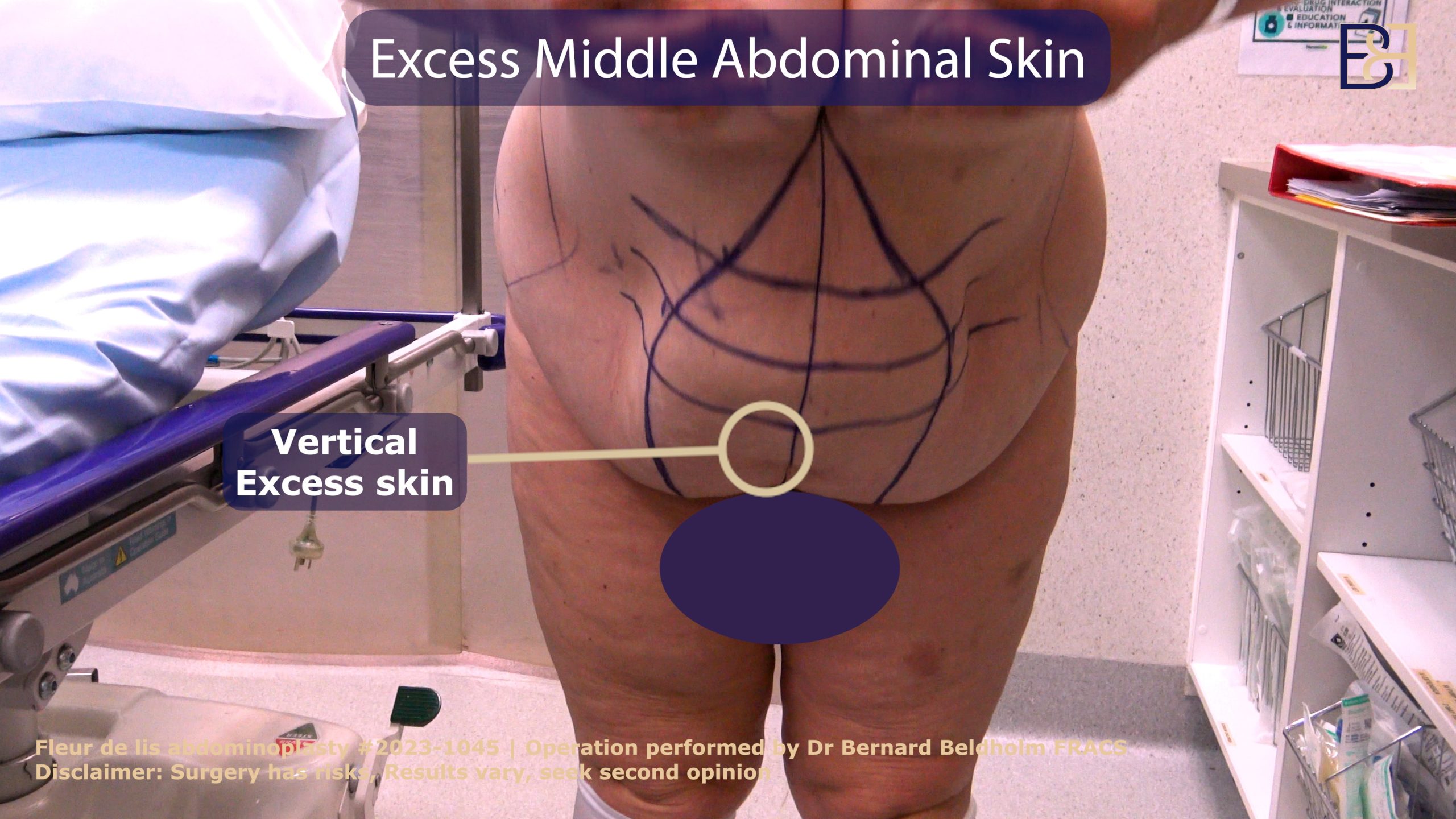
Markings

While the patient is in the anaesthetic bay, I will mark your abdomen with an indelible marker. Representing the excision area during the surgical process.
These markings serve as reference points to represent the excision area during the surgical process. The first marking involves a horizontal pattern running from hip to hip. An inferior vertical marking that runs along the upper abdomen’s midline is also indicated.
Anaesthesia

Suction-Assisted Lipectomy Fleur-De-Lis Abdominoplasty Surgery is performed using a general anaesthetic administered through an IV. After you are sedated, a tube is placed in your breathing canal by a licensed anaesthetist who will oversee the entire surgery.
VASER Liposuction (Suction assisted lipectomy)
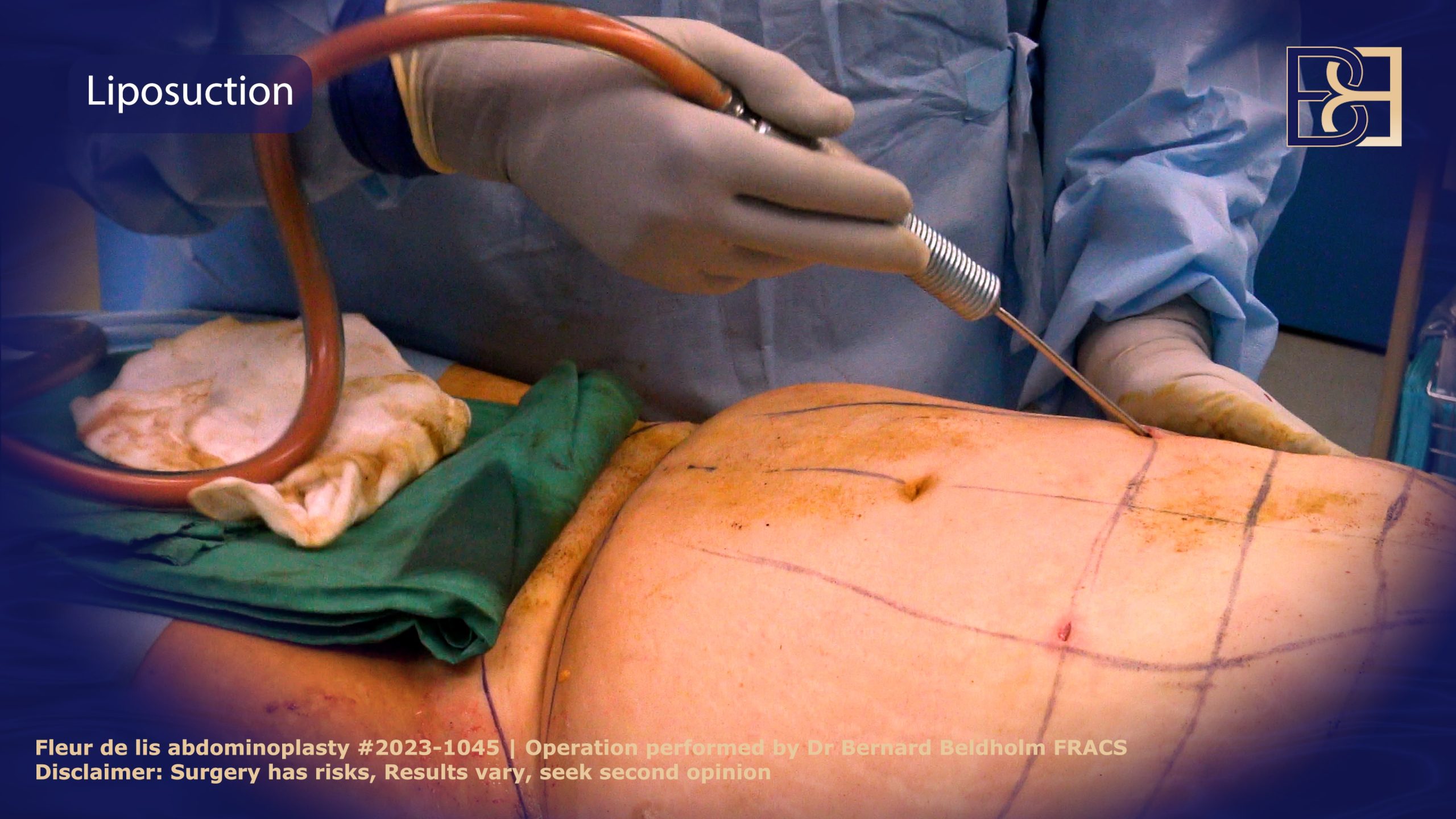
VASER Liposuction (Suction assisted lipectomy) melts fat so your abdomen will look more trim and toned. It also reduces bleeding and helps free the loose redundant skin so it can be removed easier. VASER fat reduction takes approximately 1.5 additional hours.
- First, I inject tumescent fluid mixed with adrenaline and a local anaesthetic into the target area.
- Next, I make a small incision and pass the VASER ultrasound (Suction assisted lipectomy) probe into the skin, focusing on the lateral and mons pubis areas.
- To prevent burns before introducing the probe, I place protective ports in the skin.
- When the VASER is powered on, it vibrates to break down the fat cells.
- After the fat reaches the texture of melted butter, I turn off the VASER and insert a cannula, or thin hollow tube.
- The cannula is hooked up to a suction device, which suctions out the fat.
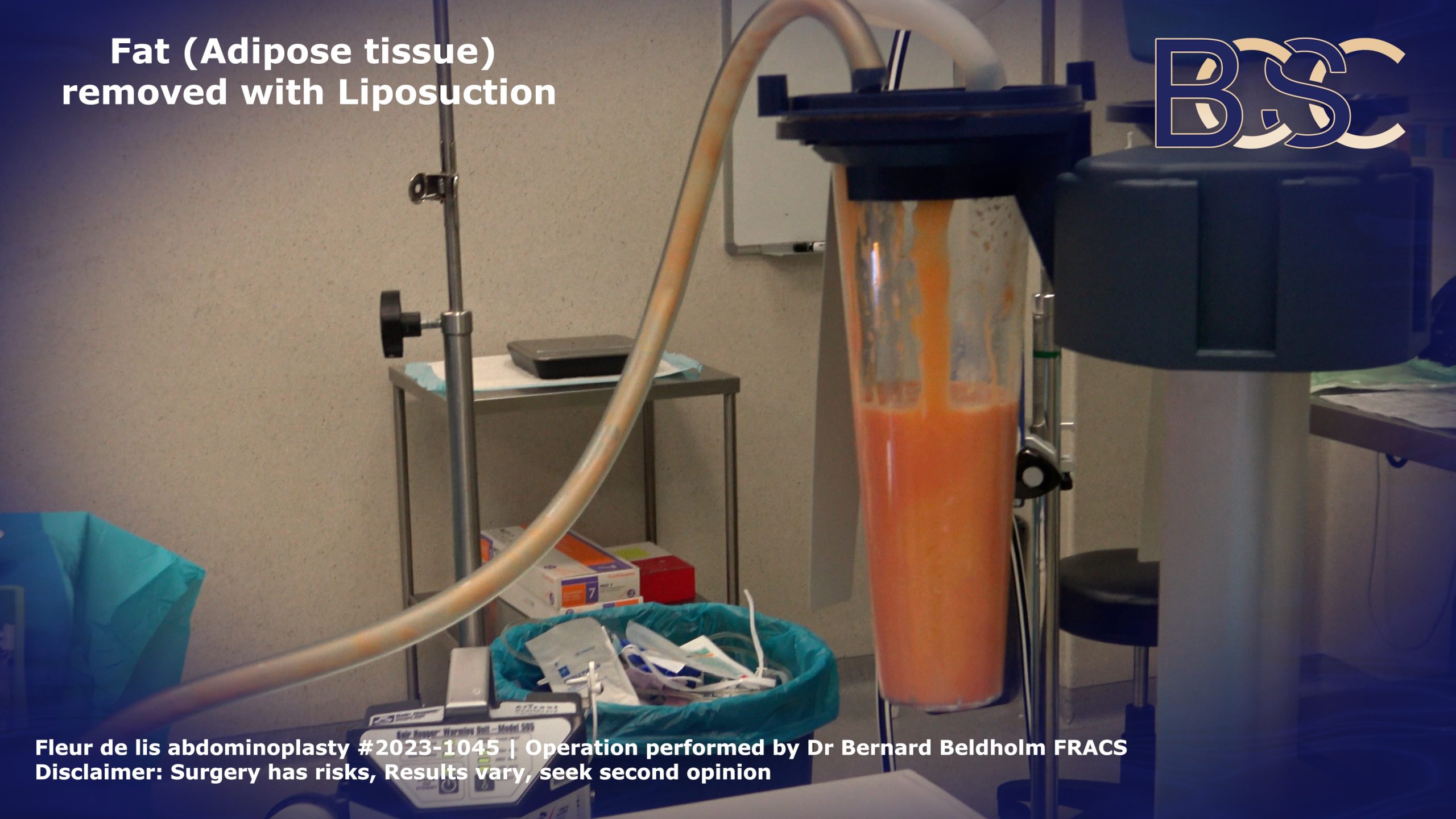
By targeting stubborn fatty areas, Suction-Assisted Lipectomy reduces the need for extensive tissue dissection. VASER liposuction is not necessary in all Fleur-de-Lis operations as many post-weight and weight loss surgery patients have minimal fat left after their bariatric procedure and subsequent weight loss.
Umbilicus Relocation
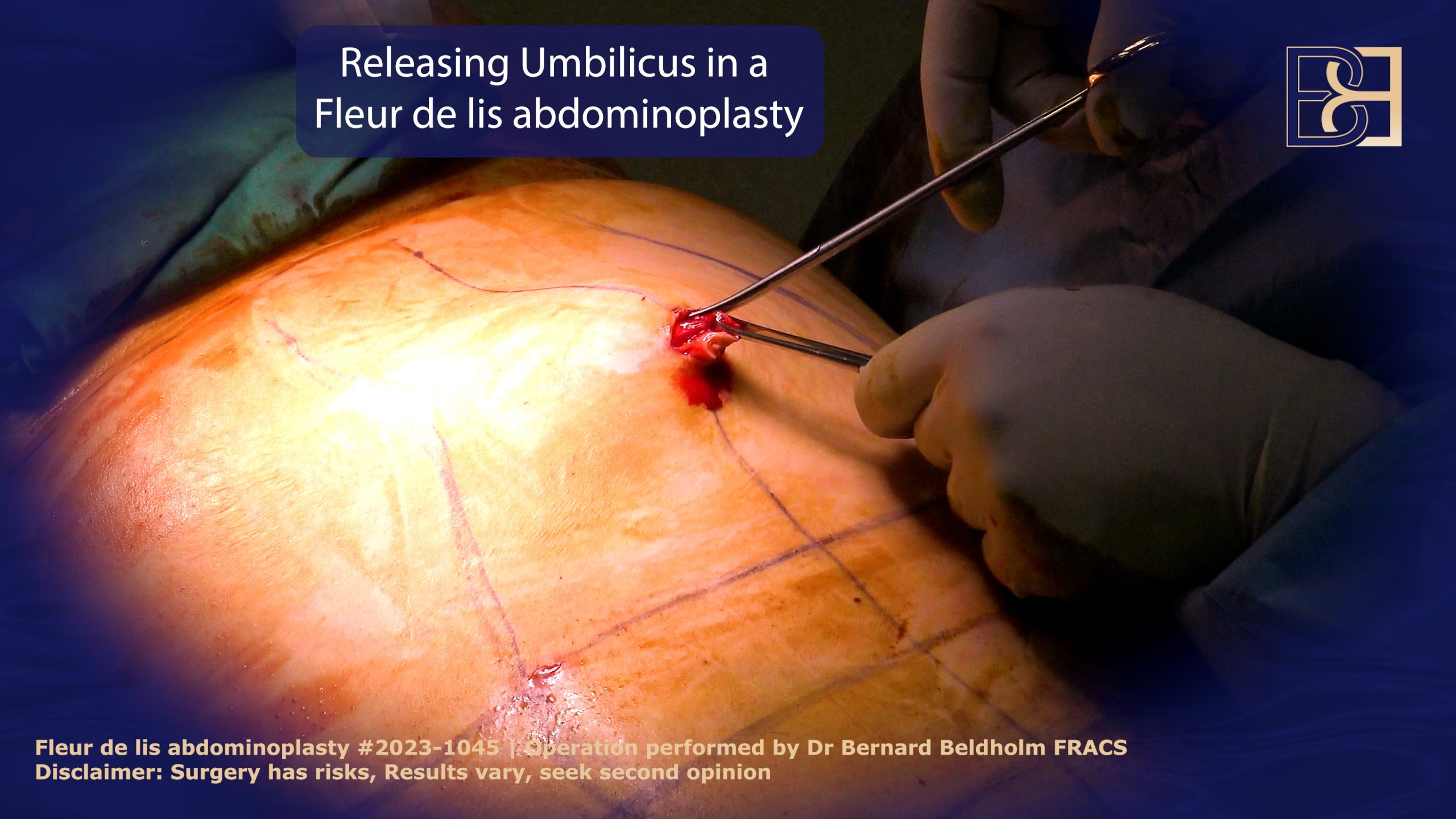
Your navel is like a button on a tufted cushion, tethering your abdominal tissues in place. Because fleur-de-lis involves the removal of extensive amounts of skin, it is necessary to relocate the umbilicus.
Freeing the Umbilicus
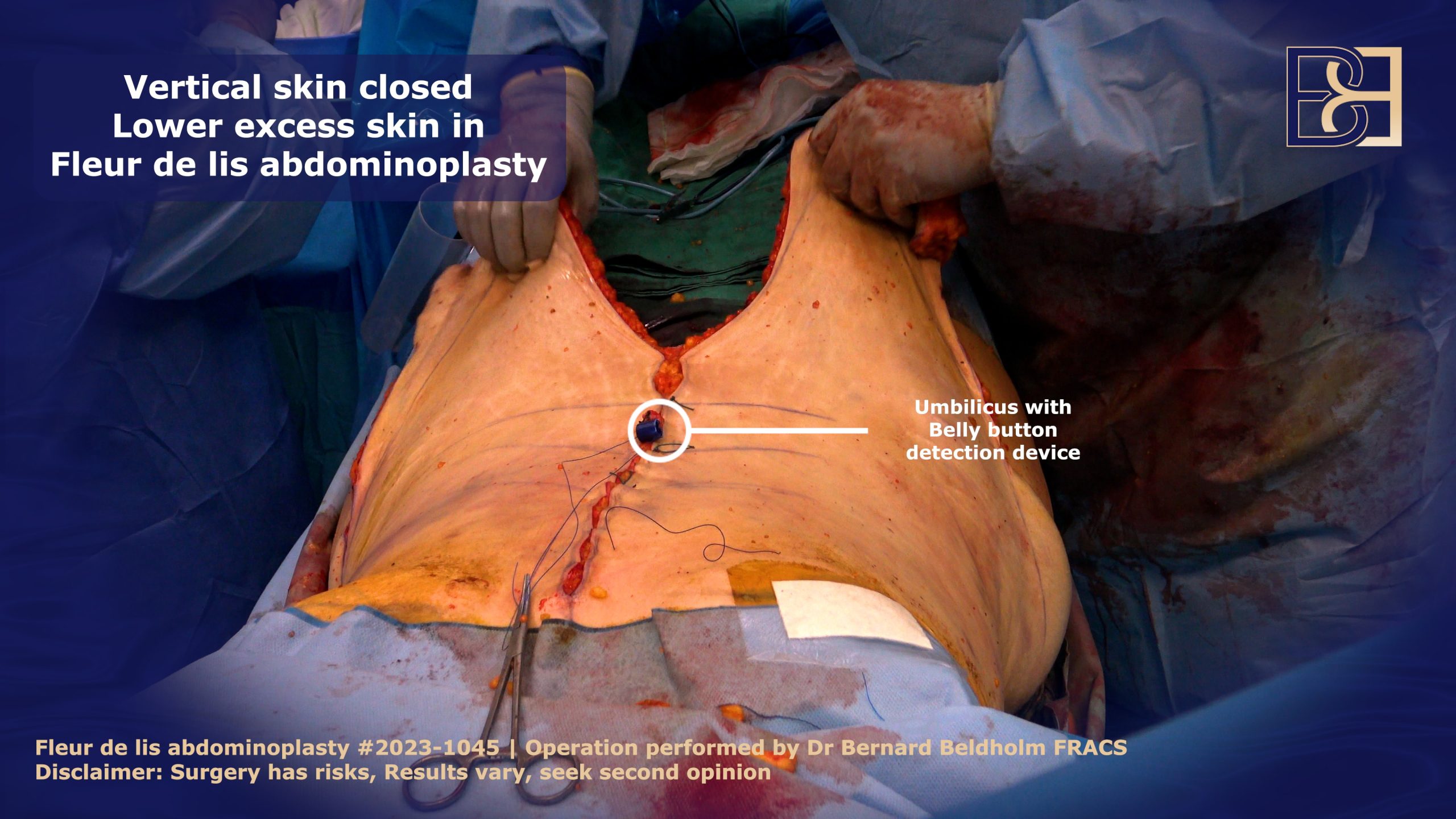
The skin around the umbilicus in the midline will be removed during the fleur-de-lis abdominoplasty. To make it easier for me to locate your belly button later in the surgery, I will attach a small plastic bit to the umbilical stalk. Once the skin in the middle is closed, I can locate the umbilicus and pull it through the vertical incision to create a new location for the belly button.

Vertical Incision
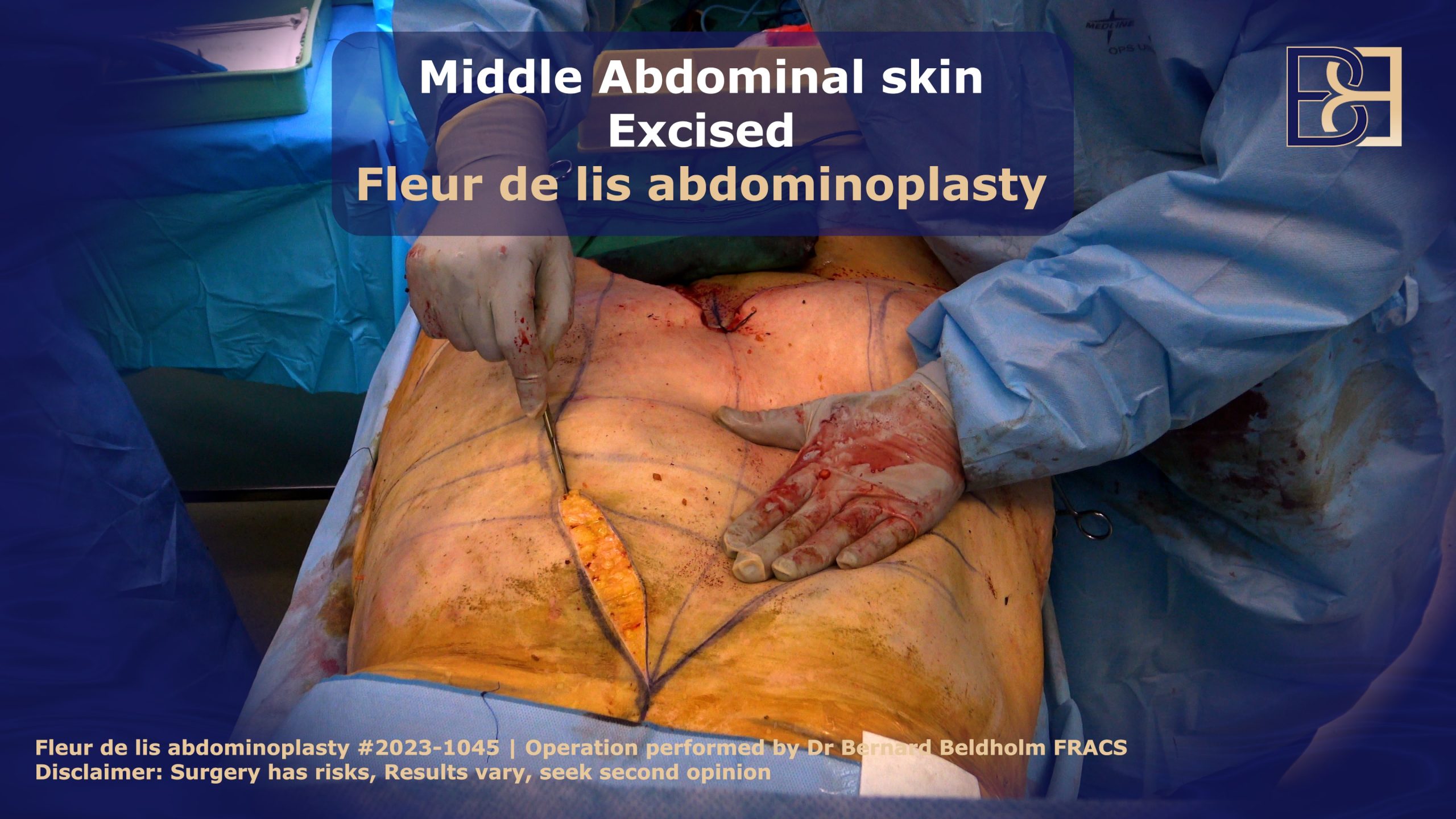
As per the markings I made in the anesthesia bay, I will use a scalpel to make an upside-down “V” on your abdomen. I will then use diathermy to seal any opened blood vessels to minimise bleeding. The dissection will continue down to the deep abdominal wall, and then any excess skin will be removed.
As I carefully remove the skin from the deeper layers, I make sure not to cut through the umbilical cord. The umbilicus detection device will assist with this. There are often major blood vessels that pass through the abdominal wall, especially around the umbilical area. The liposuction allows for less dissection which has been shown to preserve blood flow, lymphatics, and nerves.

Abdominal Muscle Separation (Diastasis Recti) Repair
Diastasis of the rectus abdominis muscle is defined as an inter-rectus distance of 22 mm or more, three centimetres above the umbilicus, when measured with the patient in a relaxed state. Diastasis of rectus abdominis is a common condition where the two long muscles of the abdomen separate from each other, particularly during the second half of pregnancy. The linea alba, the connective tissue between the muscle, can get stretched during pregnancy or weight gain leading to a separation of the abdominal muscles.
The degree of abdominal separation varies from one individual to the next. In some cases, the separation of the rectus abdominis muscle is minimal and barely observable. In others, however, it’s a visible pouch of loose skin and fat that hangs from the belly. A weakened pelvis can lead to complications such as urinary incontinence and pelvic organ prolapse, highlighting the importance of exercises that strengthen these pelvic floor muscles both during and after pregnancy.
To repair rectus abdominis muscles during Fleur-de-Lis surgery, I perform diastasis recti surgery which involves bringing the abdominal muscles together using barbed sutures called V-Loc 1 permanent sutures, which do not require knotting. This technique ensures that there are no palpable lumps post-surgery.
My technique involves two layers of sutures, with the final layer being only in the abdominal sheet, which decreases the risk of nerve, muscle, and blood vessel damage.
Close the Vertical Incision

During the vertical closure, the skin from the flanks and sides of the abdomen is brought together, creating significant tension on the wound. I use a strong 1 Ethibond suture to initially bring the tissues together. The horizontal lines that I marked out in the anaesthetic bay are then used to position the skin for an even and symmetrical closure. The initial 1 Ethibond sutures will be removed once the deeper layers have been completed. However, the deeper layers don’t have the strength to hold the skin together initially.

I will then close the skin, initially closing the deeper layers with 2/0 Vicryl sutures. These are absorbable sutures that will take approximately 56 to 70 days to absorb. The superficial layers are closed with 2 running absorbable sutures.
Remove Excessive Loose Skin on the Lower Abdomen
I will now proceed with a standard abdominoplasty to eliminate any excess skin remaining on the lower abdomen by making a horizontal incision. I will then seal any blood vessels to minimise bleeding. After that, I will loosen the skin and start working my way up from the part of the small incision towards the belly button. I will dissect the abdominal tissues just below the position of the belly button. While most of the dissection has already been done as part of the vertical skin removal, there will be some additional dissection required, particularly on the lateral part of the lower abdomen.
Finally, during the last dissection, I will bend the operating table slightly.
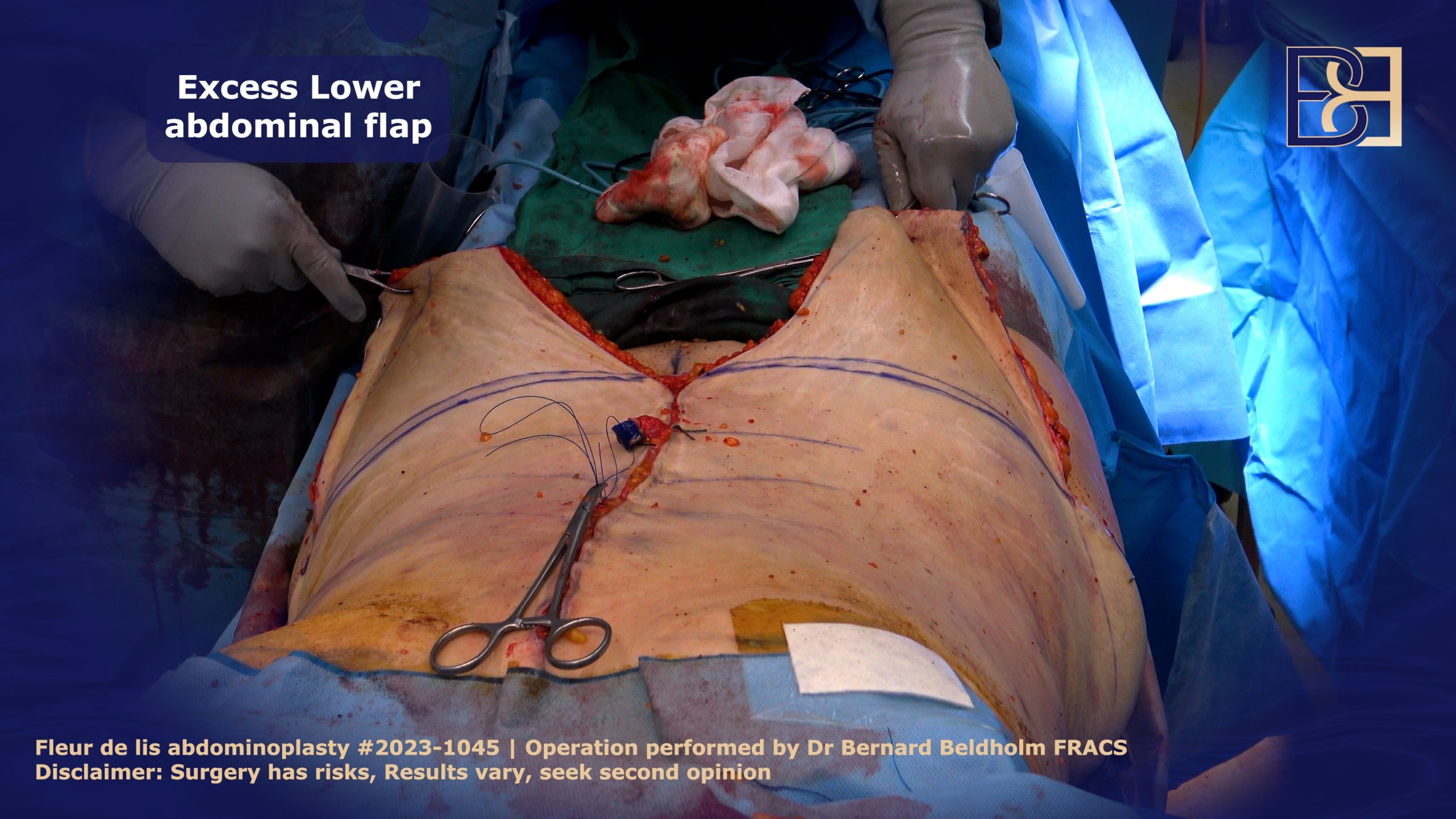
Excess Skin Removal, Lower Abdominal Wall
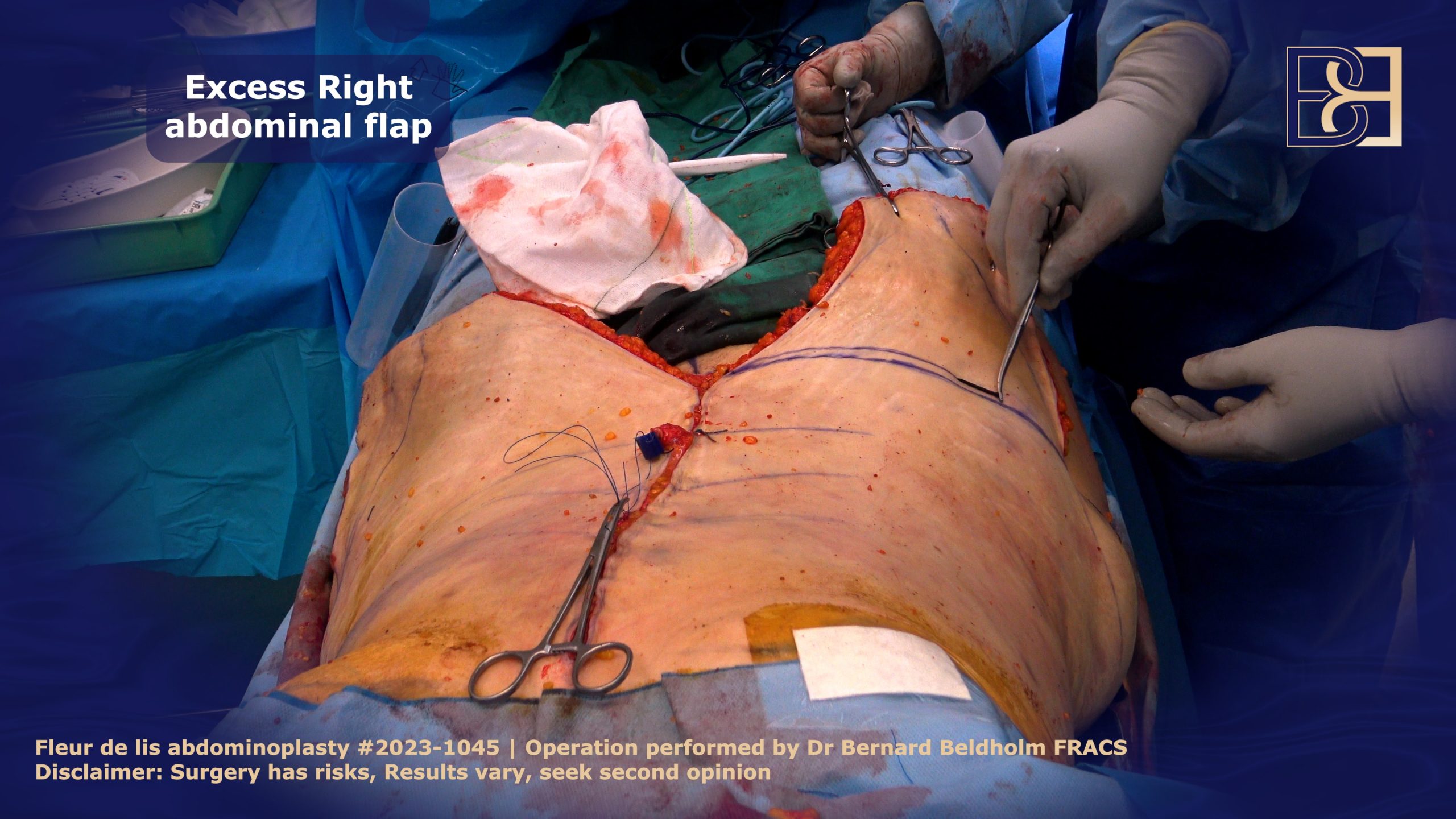
To determine the amount of loose skin that needs to be removed in the lower abdomen, I use an Alias tissue forceps to push up the lower abdominal skin and feel how far it extends.

This helps me decide where to make the incision. After identifying the line of maximum tension, I mark another line 1 cm below to allow for minimal tension when suturing the skin. Symmetry is crucial in these operations, so I always mark out both sides in a similar manner before making any incisions.
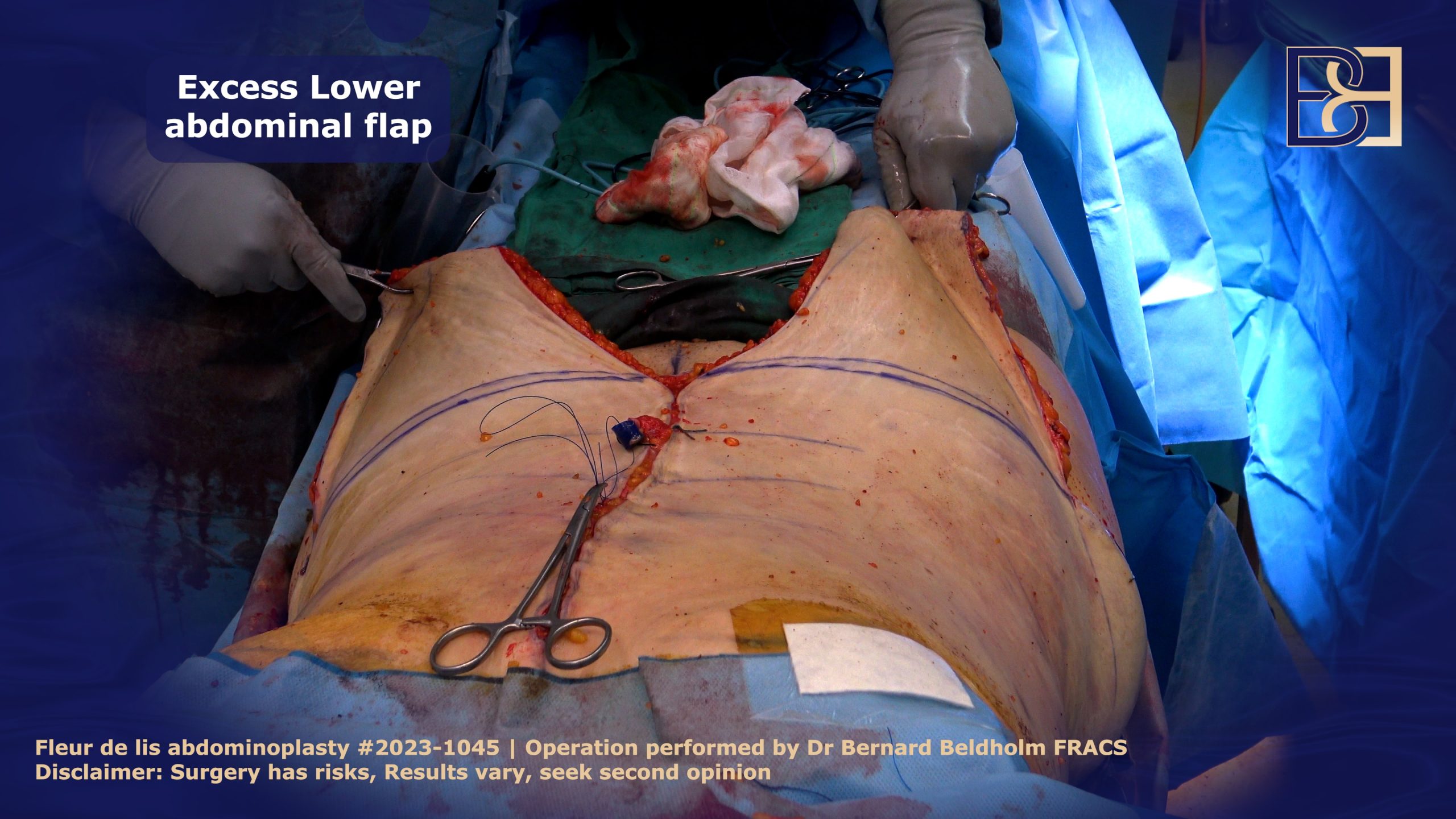
I will compare the right and left sides to ensure they are symmetrical, and also verify that the vertical incision line is in the midline and not pulled to one side.
When I excise the skin, the excision is bevelled upwards. When closing the deep layer this will hold the tension and as I close progressively more superficial there will be less and less tension on the skin. The superficial skin is under the least amount of tension. The less tension there is on the skin the better the scar will be and there is also less chance of wound breakdowns and issues with the scar.
Insert Drains

Positioned on the outer thigh area, I use Belovac 10F drains for all my fleur-de-lis abdominoplasty procedures to remove fluid and blood.
Create New Navel (Umbilicus)
Next, I will carefully shape your Umbilicus using four sutures, making every effort to bury the sutures.
I may remove a small bit of fat from behind the Umbilicus with liposuction. This creates a small depression around your belly button. Typically, the incision is quite vertical, but due to tension on the skin from the side, the Umbilicus will usually be pulled apart and gradually become more oval in shape over time.
Apply PICO Dressing

Next, I apply negative pressure PICO bandages to prevent contamination and support the wound as it heals. This soft bandage, which is attached to a battery pack, exerts negative pressure on the wound to promote healing, lowering the risk of infection by trapping up to 99.9% of bacteria with AIRLOCK technology.
The PICO Negative Pressure device features two dressing kits and a sterile pump that creates negative pressure on the entire wound surface, which effectively promotes healing. Generating negative pressure (80mmHg nominal), the sterile dressing kits keep the wound dry by absorbing any discharge and evaporating it through the outer layer. These dressings will usually stay on for 7 days and are then replaced by a tape dressing.
Apply Compression Garments
To minimise swelling, a normal response to surgery, a compression garment is applied. Compression garments lower the risk of seroma and help the skin mould around your new body contours.
Additionally, wearing a compression garment is recommended to reduce swelling, provide support to the surgical area, promote proper healing, and aid in the recovery process from open surgery.
Recovery
Generally speaking, this is what you can expect as you recover from surgery.
Hospital stay: You will spend around 2 days in the hospital.
Showering: Because you cannot get the PICO dressing wet, sponge baths will be your best option. Once the dressing is removed, you will be able to resume your normal hygiene schedule.
Pain medications: Pain is generally moderate after the procedure, although each patient’s experience is different. Pain medications will be prescribed to make your recovery less challenging.
Downtime: For the most part, my patients take two to four weeks off work and start driving after three to four weeks. Heavy lifting and exercise are off limits for at least six weeks.
For more information, read my article Dr. Beldholm’s Step-by-Step Guide to Fleur-de-Lis Abdominoplasty.
FAQs
Is VASER Liposuction-Assisted FDL Abdominoplasty Covered by Medicare or Private Health Insurance?
Medicare will cover your surgery if it is deemed medically necessary. After reviewing your medical history during a physical exam, I will determine whether you meet the specified criteria, such as the loose skin and fat affecting your work and daily life.
Post Pregnancy
Many pregnant women and new mums are eligible for medicare rebates to patients for undergoing abdominoplasty to cover symptoms resulting from pregnancy, including separated abdominal muscles (diastasis recti).
Post-Weight Loss
Medicare covers patients undergoing abdominoplasty (tummy tuck) procedure to remove excess loose skin resulting from significant weight loss of at least 5 BMIs. In addition, the patient must have maintained a stable weight for a minimum of six months before surgery.
How Can I Tell If My Abdominal Muscles Are Torn?
A coning or doming of the ab muscles during physical exertion is one of the key signs of muscle separation. There are several other indications, including:
- Jelly-like texture around the belly button
- Difficulty lifting heavy objects
- Pelvic and hip pain
- Incontinence
- Lower back pain
- Visible bulge or pouch of loose skin around the belly button
- Poor posture
- Constipation
- Lack of core strength
- Pain during intercourse
Abdominal exercises play a crucial role in strengthening the muscles and supporting recovery. However, certain exercises can make ab separation worse and should be avoided. The best exercises will not make abdominal separation worse. Avoid undue strain by refraining from stomach crunches and sit-ups, especially during postpartum recovery.
Is VASER Liposuction-Assisted FDL Abdominoplasty Considered Major Surgery?
VASER Liposuction-Assisted FDL Abdominoplasty is considered major surgery because, not only does it remove significant amounts of excess skin, the body’s largest organ, but it alters the anatomical structure of the body, poses risk factors, is a complex procedure, involves the use of general anaesthesia, and requires a hospital stay.
Book your appointment online now
Take Away
In my opinion, a successful surgery procedure, such as VASER Liposuction (Suction Assisted Lipectomy) combined with FDL Abdominoplasty, is a great indication after significant weight loss. This combination technique, which involves a more aggressive approach to the removal of fat through the use of VASER liposuction (Suction Assisted Lipectomy), has resulted in the highest level of successful outcomes due, in part, to limited dissection.
For a more in-depth review of this procedure and how it will apply to your exact physical condition, areas of concerns, and individual circumstances, I invite you to book a consultation with me. During this session, I will answer all of your questions, show you my library of before and after patient photos, review where the procedure will take place, and discuss cost and other considerations. I will also conduct a physical examination to determine the best approach.