According to an article, Classification and Management of Gynecomastia: Defining the Role of Ultrasound-Assisted Liposuction, written by Rod J. Rohrich, M.D., et al., medical management has had limited success for the treatment of gynaecomastia, with excisional surgical techniques becoming the accepted standard. However, with such important physical and psychological impacts and an incidence as high as 65% in the male population, recommendations for evaluation and treatment remained arbitrary.
Book your appointment online now
Why New System Was Developed
For this reason, Dr Rohrich felt it necessary to develop a new diagnostic algorithm with an emphasis on a comprehensive history and physical examination, minimising the need for unnecessary diagnostic testing.
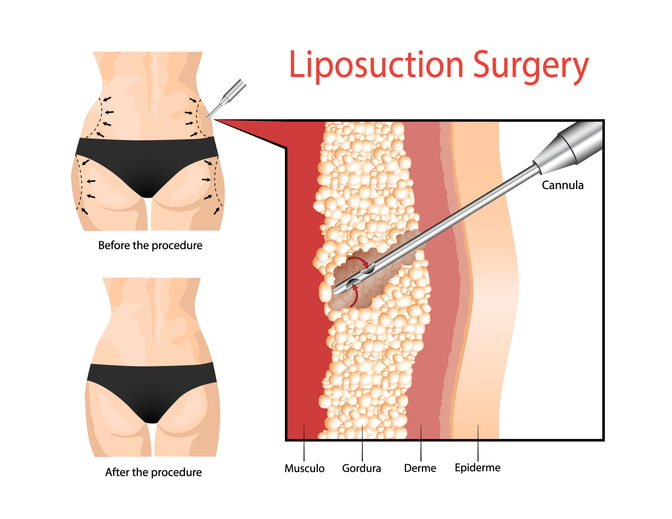
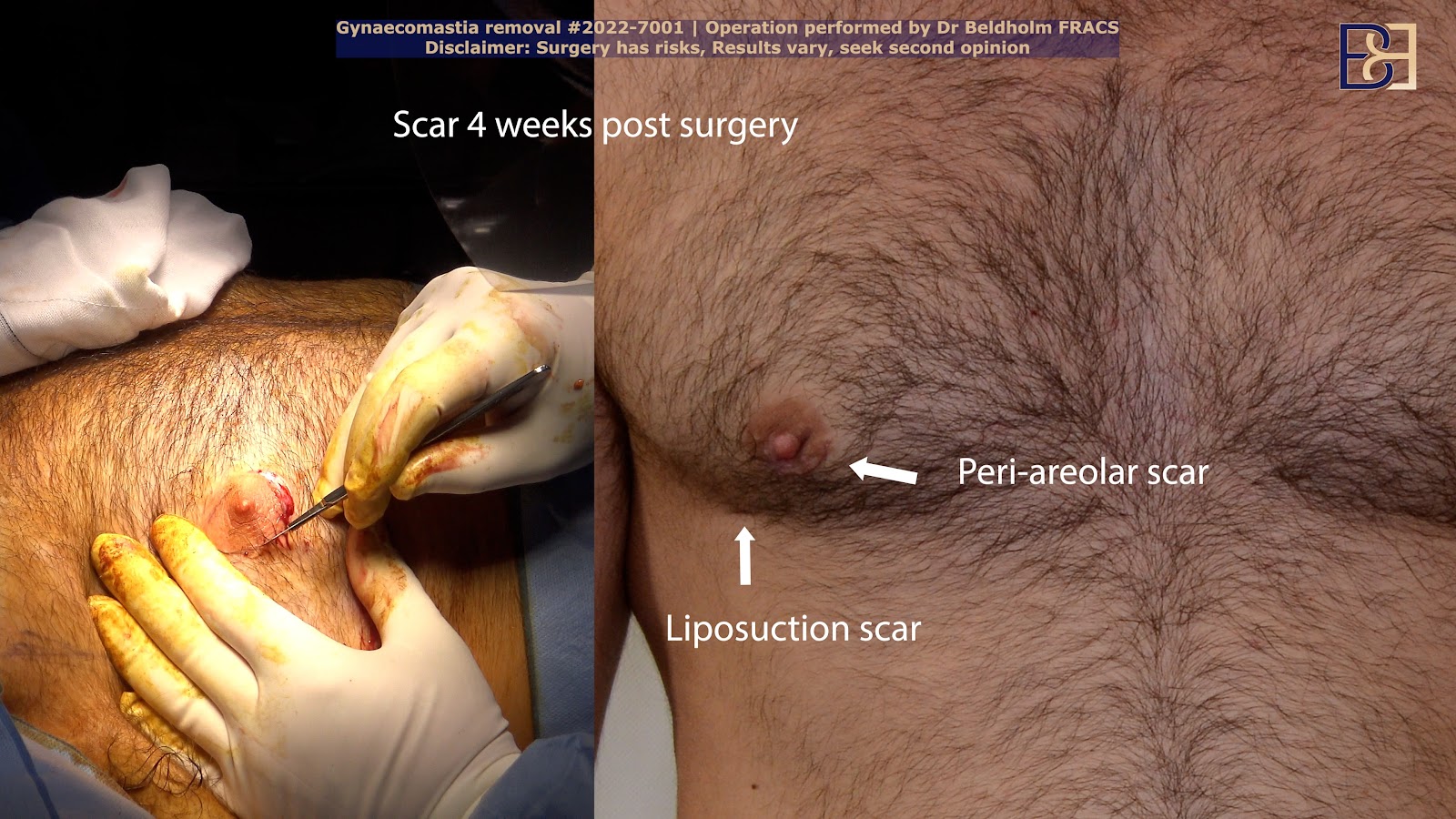
In the article, the authors noted that because excisional techniques subject patients to large, visible scars, ultrasound-assisted liposuction would be a more effective method for the treatment of gynaecomastia.
Particularly efficient in the removal of the dense, fibrous male breast tissue while offering advantages in minimal external scarring, a new system of classification and graduated treatment to treat gynaecomastia based on glandular tissue versus fibrous hypertrophy and degree of breast ptosis (skin excess) was proposed.
Patient Study
From 1987 to 2000, the University of Texas Southwestern Department of Plastic Surgery studied over 60 patients with gynecomastia, demonstrating an overall success rate of 86.9% using suction-assisted lipectomy and ultrasound-assisted liposuction. Using ultrasound-assisted liposuction exclusively, no additional treatment was used in 53 of the 61 patients, with staged excision of remaining breast tissue and skin required for only 8 of the most severe cases (four with grade III disease and four with grade IV) to optimise results.
Based on the author’s 14 years of experience, a new classification system for gynaecomastia was developed, incorporating ultrasound-assisted liposuction. As a stand-alone treatment for less severe cases or in conjunction with surgical removal for higher levels of breast enlargement severity, Rohrich proposed that this was the most acceptable solution to treat gynecomastia.
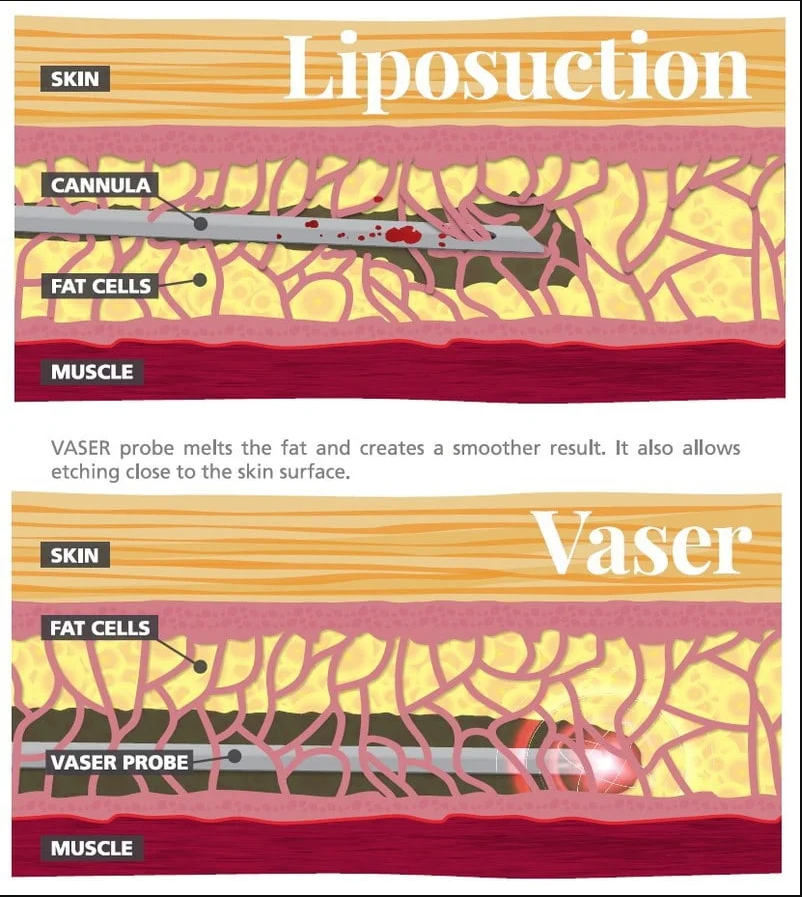
The authors noted that previous clinical classification systems, as suggested by Simon and Cohen et al., offered excellent guidelines for graduated management of gynecomastia based on degrees of lipodystrophy and skin excess in male breasts. Rohich, however, refined the ultrasound-assisted liposuction technique by incorporating a three-stage process of subcutaneous infiltration of a wetting solution followed by ultrasound-assisted liposuction.
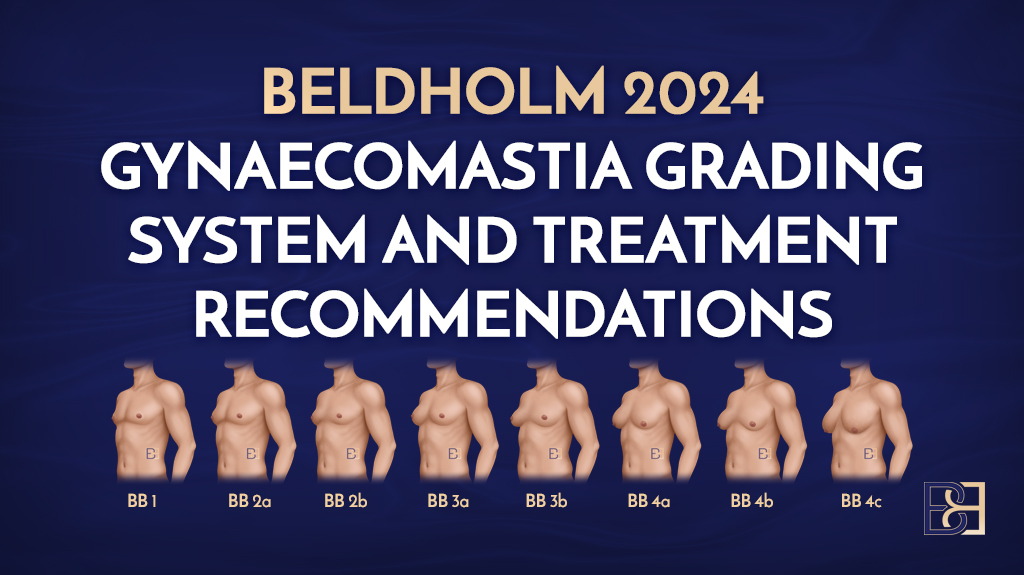
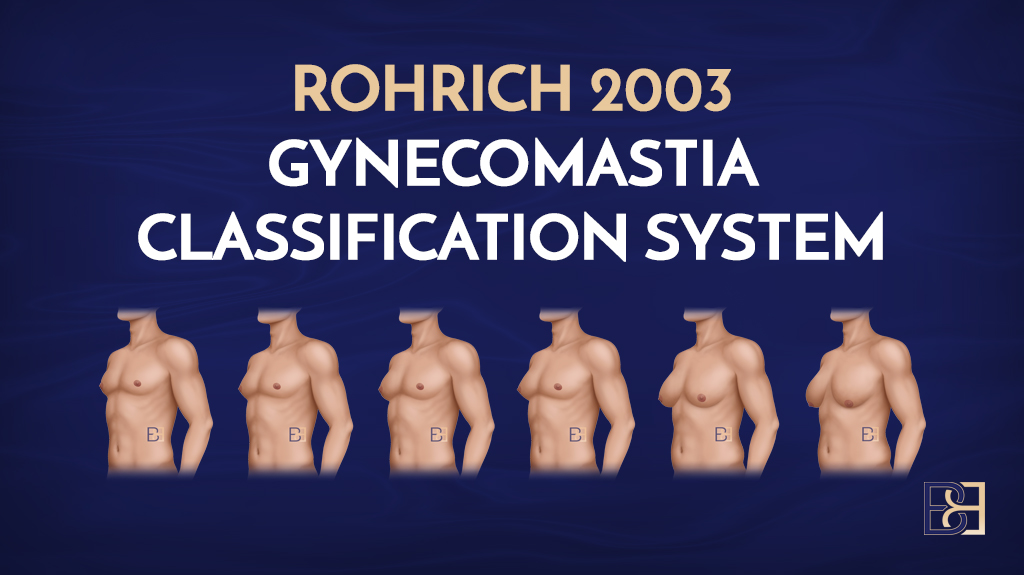
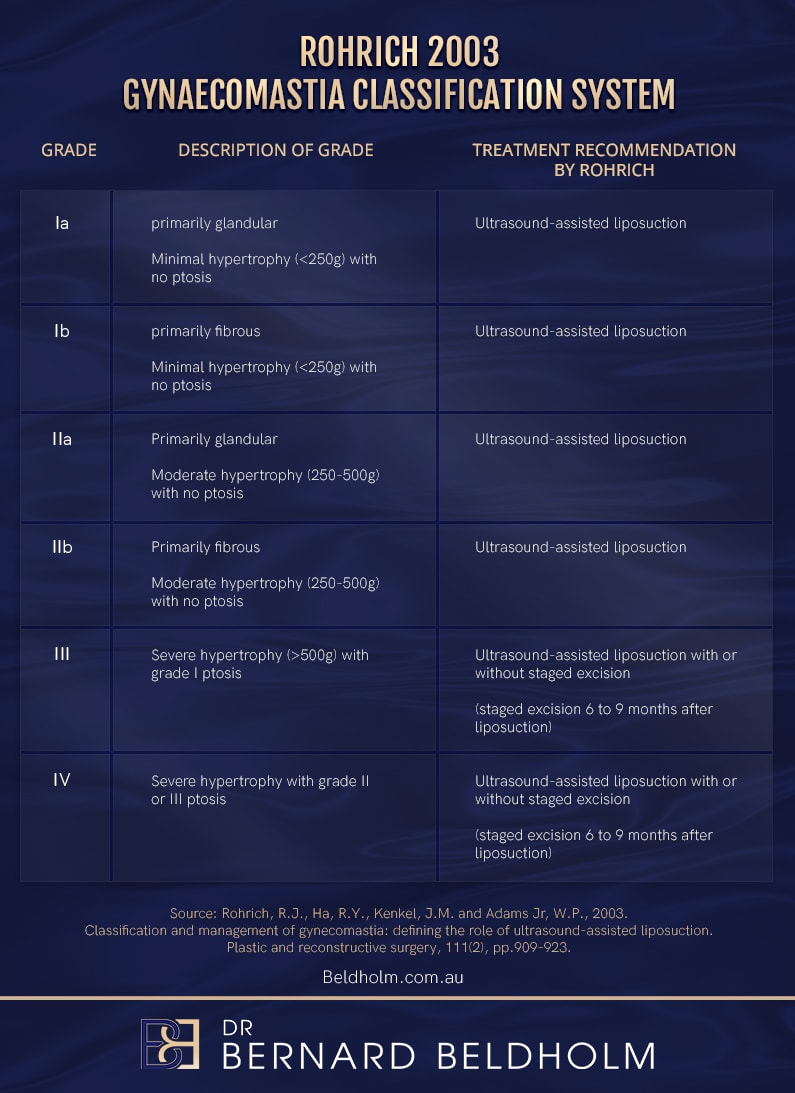
Rohrich offers a new classification system for gynaecomastia surgery and the preferred treatment for each grade,
The Rohrich Gynecomastia Classification System for gynaecomastia surgery categorizes gynecomastia into four grades based on the amount and character of breast hypertrophy, the degree of ptosis, severity of glandular breast tissue enlargement, excess adipose tissue, and skin redundancy. This system provides a structured framework for evaluating the condition and selecting appropriate surgical approaches by incorporating ultrasound-assisted liposuction.
Here’s a breakdown of the grades:
Rohrich 2003 Gynaecomastia Classification System Grades
Grade I: Minimal Gynecomastia
- Characteristics:
- Minor glandular and adipose tissue enlargement in one or both breasts.
- No significant skin redundancy.
- Areola maintains normal positioning without ptosis.
- Surgical Approach:
- Suction-assisted lipectomy ( liposuction) or direct glandular excision is often sufficient.
Grade Ia
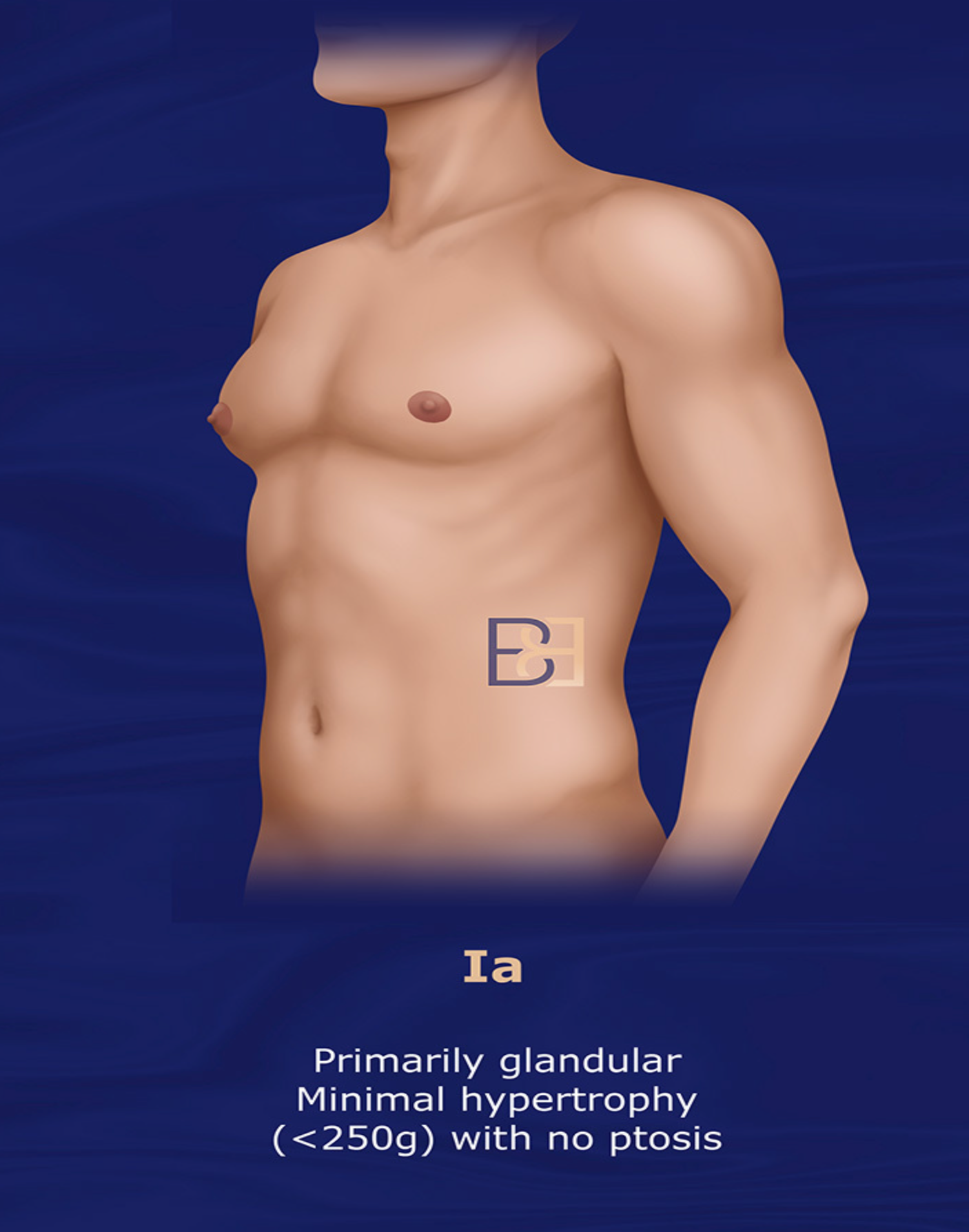
- Presentation: Primarily Glandular, Minimal Hypertrophy (<250g), No Ptosis, one or both breasts
- Surgical Approach:
- Suction-assisted lipectomy ( liposuction) or direct glandular excision is often sufficient.
Grade Ib
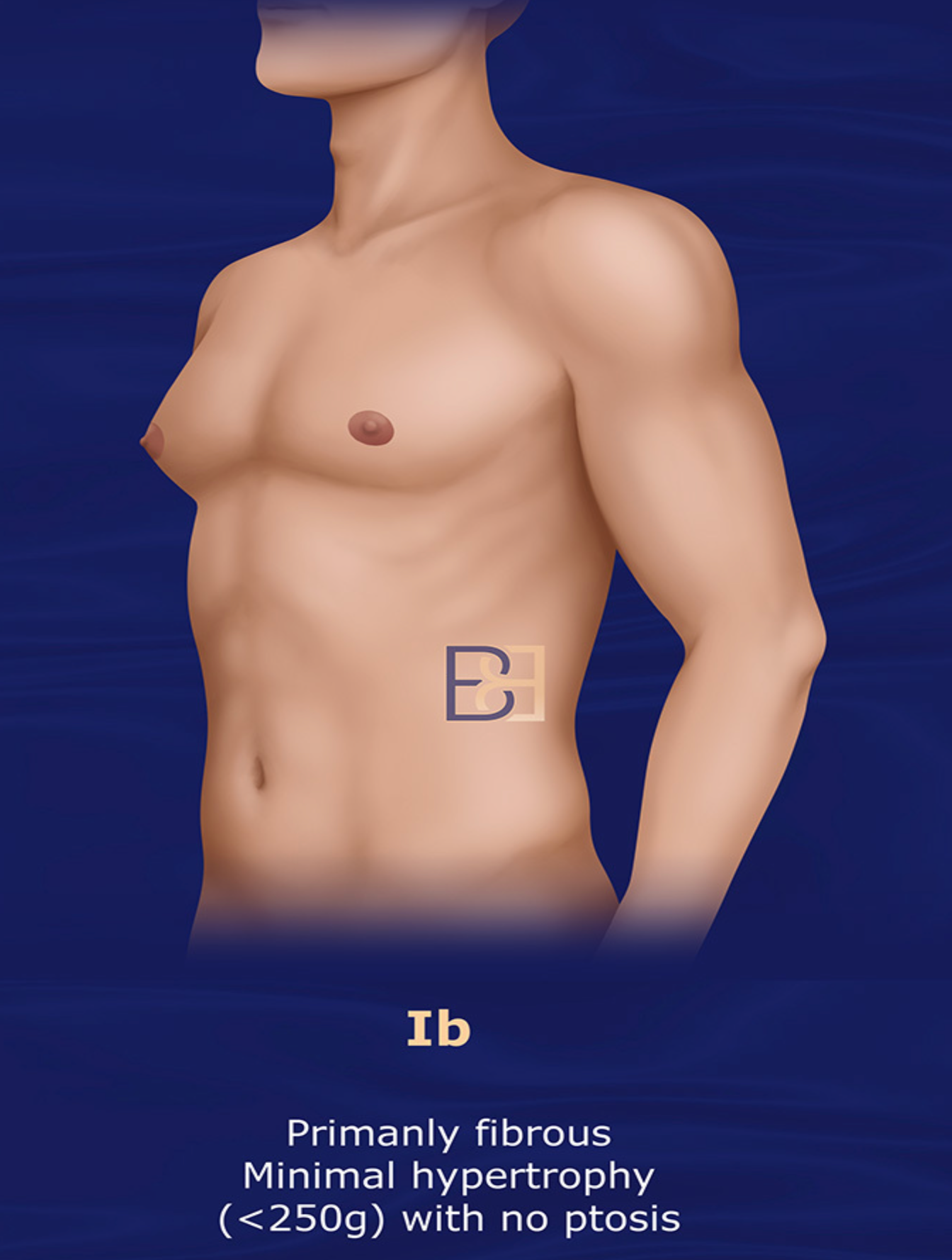
- Presentation:
- Primarily Fibrous, Moderate Hypertrophy (<250g), No Ptosis, in one or both breasts
- Surgical Approach:
- Ultrasound-assisted Liposuction
Grade II: Moderate Gynecomastia without Skin Redundancy
- Characteristics:
- Moderate enlargement of glandular and fatty tissue.
- No or minimal skin redundancy.
- Areola remains at its normal position.
Grade IIa
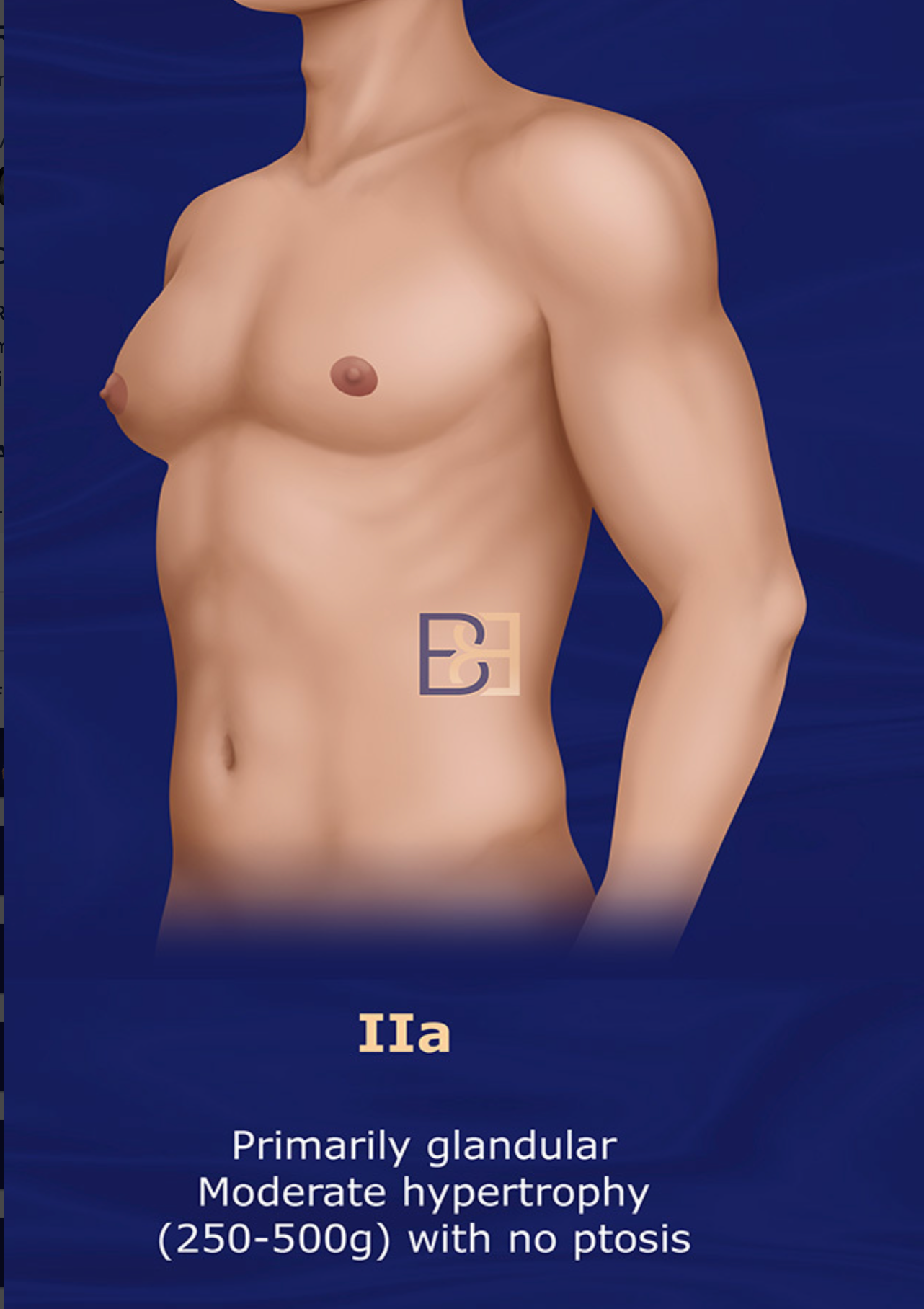
- Presentation:
- Primarily Glandular, Moderate Hypertrophy 250 – 500g), No Ptosis, in one or both breasts
- Surgical Approach:
- Ultrasound-assisted Liposuction
Grade IIb

- Presentation:
- Primarily Fibrous, Moderate Hypertrophy 250 – 500g), No Ptosis in one or both breasts
- Surgical Approach:
- A combination of Suction-assisted lipectomy ( liposuction) and glandular excision is typically required to achieve optimal contouring.
Grade III: Moderate Gynecomastia with Skin Redundancy
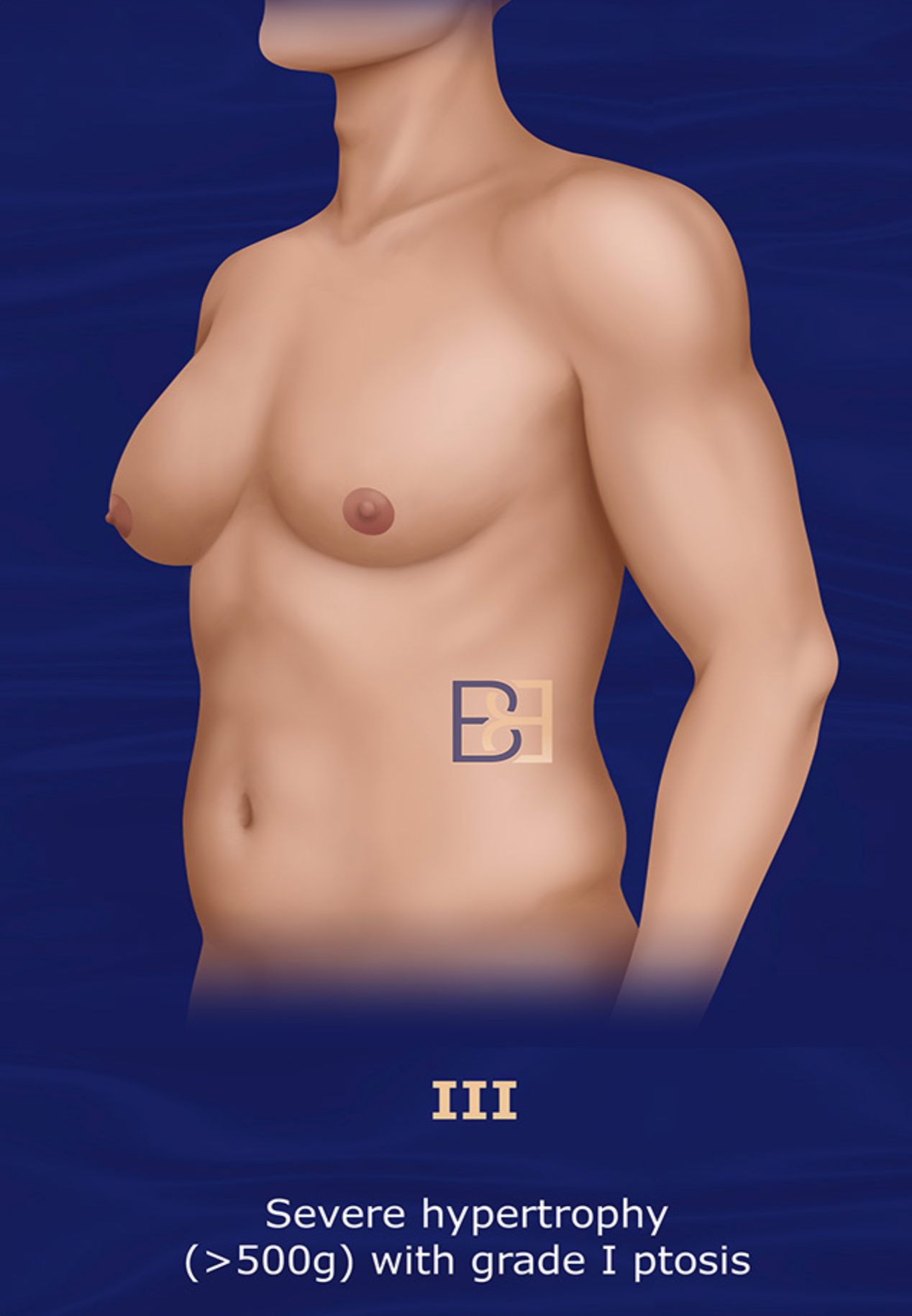
- Characteristics:
- Moderate to significant glandular and fatty tissue enlargement in one or both breasts.
- Noticeable skin redundancy.
- Possible mild areolar ptosis.
- Presentation:
- Severe Hypertrophy (>500g), Grade 1 Ptosis in one or both breasts
- Surgical Approach:
- Ultrasound-assisted liposuction with or without staged excision. Staged excision surgical treatment 6 to 9 months after Suction-assisted lipectomy ( liposuction).
Grade IV: Severe Gynecomastia with Marked Skin Redundancy
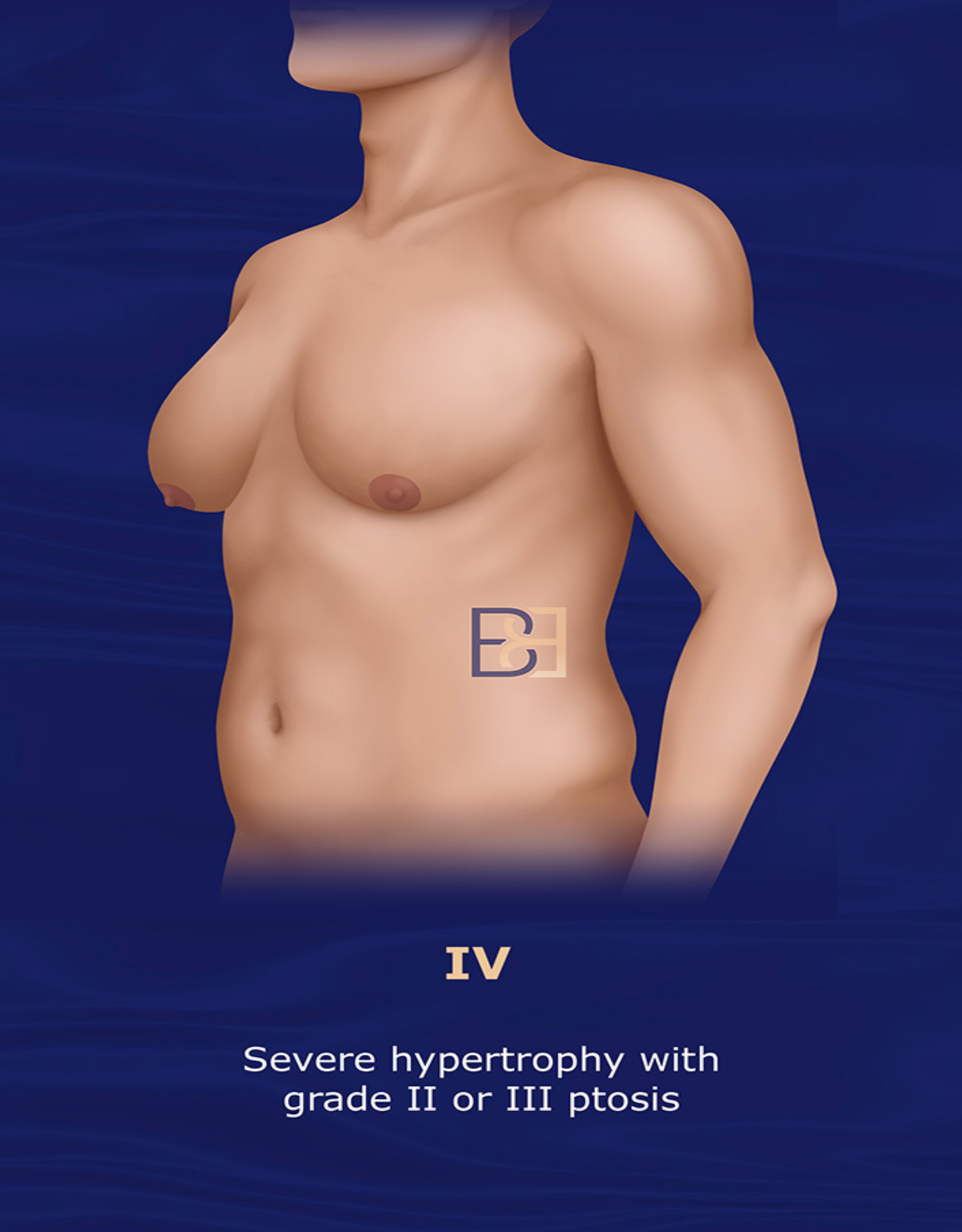
- Presentation:
- Severe Hypertrophy (>500g), Grade II or III Ptosis
- Characteristics:
- Severe enlargement of glandular and fatty tissue.
- Significant skin redundancy with marked ptosis.
- The chest may resemble a female breast in appearance.
- Surgical Approach:
- Ultrasound-assisted liposuction with or without staged excision. Staged excision 6 to 9 months after liposuction.
- Requires extensive tissue excision, Suction-assisted lipectomy ( liposuction), and significant skin tightening or lifting procedures.
NOTE: This classification helps surgeons customise treatment based on individual anatomical needs, ensuring effective management of gynecomastia across varying severities.
Advantages of Rohrich’s Ultrasound-Assisted Liposuction
Ultrasound-Assisted Liposuction offers a range of advantages, including precision, reduced trauma, and elevated aesthetic results. While it may not be suitable for all cases (e.g., those requiring significant glandular tissue removal), it is an excellent option for treating gynaecomastia with a fatty component.
Ultrasound-Assisted Liposuction (UAL) offers several advantages for the treatment of gynecomastia, making it a popular choice in certain cases.
Below are the key benefits:
1. Effective Fat Emulsification
UAL uses ultrasonic energy to liquefy fat before removal, making it easier to extract even dense or fibrous fat tissues, which are common in gynecomastia.
2. Precision in Fat Removal
The targeted nature of ultrasound allows for precise fat removal, reducing the likelihood of uneven contours.
3. Reduced Trauma to Surrounding Tissues
Compared to traditional liposuction, UAL minimizes damage to blood vessels, nerves, and connective tissues, leading to less bruising and swelling postoperatively.
4. Enhanced Contouring
UAL facilitates smoother contouring, particularly in areas where gynecomastia presents with tough or fibrous tissue.
5. Skin Retraction Support
The heat generated by the ultrasound waves can stimulate collagen production, promoting mild skin tightening, which is beneficial for patients with moderate skin laxity.
6. Combined Treatment Capability
UAL can be used in combination with other techniques, such as glandular tissue excision, to treat both fatty and glandular components of gynecomastia comprehensively.
NOTE: Always consult with an experienced surgeon to determine if UAL is the best approach for your specific condition.
Disadvantages of Rohrich’s Ultrasound-Assisted Liposuction System for the Treatment of Gynaecomastia
Ultrasound-Assisted Liposuction can be an effective treatment for gynecomastia, but it also has some disadvantages that should be considered:
1. Risk of Burns
Because ultrasound energy generates heat, skin burns, tissue damage, or internal injuries may result, if not performed carefully.
2. Prolonged Surgery Time
UAL procedures often take longer compared to traditional Suction-assisted lipectomy ( liposuction) due to the additional steps involved in emulsifying the fat.
3. Increased Cost
Specialized equipment and expertise required for UAL make it more expensive than traditional Suction-assisted lipectomy ( liposuction) or other techniques for gynecomastia treatment.
4. Risk of Uneven Fat Removal
While UAL is designed to target specific areas, improper technique or excessive fat removal can lead to irregular contours or asymmetry in the chest.
5. Potential for Nerve and Tissue Damage
The energy from ultrasound waves can inadvertently affect surrounding tissues, leading to numbness, altered sensation, or delayed healing.
6. Limited Skin Tightening
UAL is primarily effective for fat removal, but it may not significantly tighten loose skin, which can be an issue in patients with poor skin elasticity.
7. Higher Risk of Seromas
UAL may lead to a higher incidence of seromas (fluid-filled pockets) compared to traditional liposuction.
8. Postoperative Pain and Swelling
Patients undergoing UAL may experience greater postoperative pain, swelling, or bruising due to the energy used in the procedure.
9. Dependency on Surgeon Skill
UAL requires a skilled surgeon with expertise in using ultrasound technology to minimize risks and achieve optimal results. Inexperienced practitioners may increase complications.
10. Not Suitable for All Cases
- UAL may not be effective for treating fibrous or glandular tissue commonly found in gynaecomastia; excisional surgery might still be necessary in such cases.
Causes of Gynaecomastia
The cause of gynaecomastia (the enlargement of male breast fat and excess skin), is commonly the result of a hormonal imbalance in the hormones oestrogen (which stimulates breast tissue growth) and androgens like testosterone (which inhibit breast tissue growth). A condition that can occur at any age and may have various underlying causes, hormonal, medical, and lifestyle factors may cause gynaecomastia. Here’s an overview of common causes:
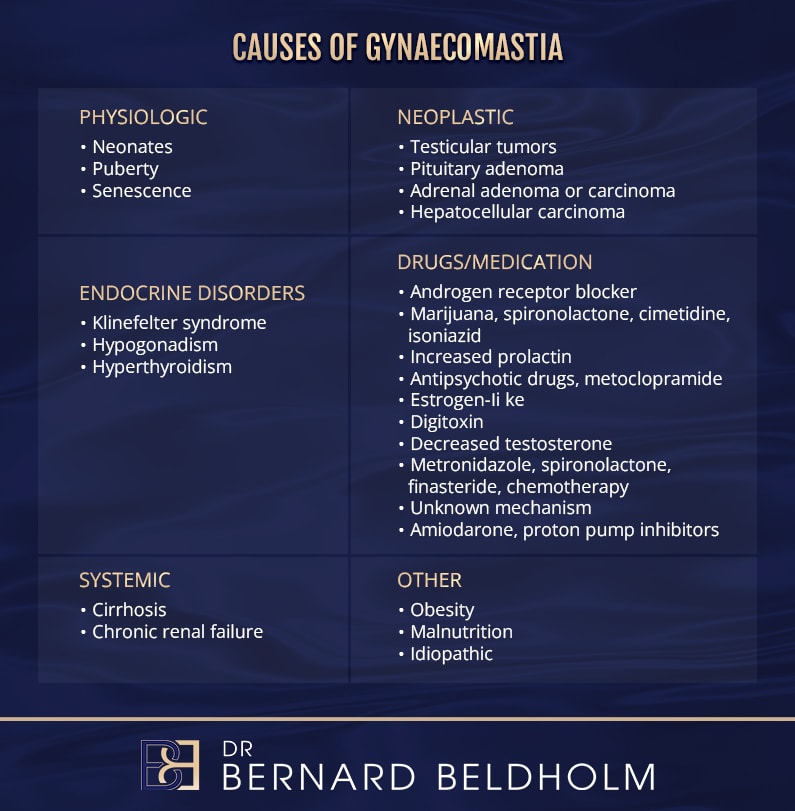
1. Hormonal Imbalances
- Puberty: Temporary hormonal fluctuations during puberty can lead to gynaecomastia, which often resolves without treatment.
- Ageing: Natural decline in testosterone levels and relative increases in estrogen can trigger gynaecomastia in older men.
- Endocrine Disorders: Conditions such as hypogonadism (low testosterone production) or hyperthyroidism (excess thyroid hormones) disrupt hormonal balance.
2. Medications
Certain drugs can interfere with hormonal regulation, causing gynaecomastia. Examples include:
- Anti-androgens
- Anabolic Steroids
- Medications for Heart Conditions
- Antipsychotics and Antidepressants
- Chemotherapy and Anti-HIV Drugs
3. Underlying Health Conditions
- Liver Disease: Chronic liver diseases (e.g., cirrhosis) can lead to hormonal imbalances.
- Kidney Disease: Hormonal alterations in patients undergoing dialysis.
- Tumors: Tumors in the testicles, adrenal glands, or pituitary gland can cause abnormal hormone production.
- Obesity: Increased aromatase activity in fat tissue converts testosterone to estrogen, contributing to gynaecomastia.
4. Lifestyle and Substance Use
- Alcohol: Chronic alcohol consumption disrupts hormone production.
- Recreational Drugs: Substances like marijuana, amphetamines, heroin, and methadone can lead to gynaecomastia.
- Dietary Supplements: Overuse of certain herbal products or supplements (e.g., those containing tea tree or lavender oils) may mimic estrogenic effects.
5. Idiopathic (Unknown)
In some cases, no clear cause is identified. This is referred to as idiopathic gynaecomastia.
Understanding the cause of gynaecomastia is essential for effective treatment. Diagnosis often includes a detailed medical history, physical examination, and, if needed, laboratory or imaging tests to rule out serious underlying conditions.
Dr Beldholm’s Final Thoughts

From a surgical point of view, I look at gynaecomastia as a chest with a female appearance in a male, regardless of the cause or category.
While Roerich’s grading system offers certain advantages, its disadvantages make it important for patients to carefully evaluate their options and choose a qualified surgeon.
The Rohrich Gynaecomastia Classification System provides a practical and structured approach to categorizing gynaecomastia cases based on severity and associated tissue characteristics. This classification aids surgeons in tailoring treatment strategies to each patient’s unique needs, optimising both aesthetic outcomes. By emphasising factors such as the extent of glandular and adipose tissue, skin elasticity, and areolar positioning, the system facilitates more precise surgical planning. As gynaecomastia treatment continues to evolve, the Rohrich system remains an invaluable tool in guiding clinical decision-making and advancing the field of male chest contouring.
For a deeper dive into grading systems for gynaecomastia, read my article, Dr. Bernard Beldholm’s Comprehensive Summary of Gynaecomastia Surgery Grading Systems.
To learn more about the surgery, whether you’re a candidate for the procedure, and the overall process in my article, Essential Insights on Gynaecomastia Surgery for Men, or book a consultation to learn if gynaecomastia surgery is right for you.
After performing a thorough examination and asking questions about your goals, concerns, expectations, and medical history, I will tell you about the benefits, risks, downtime, cost associated with the surgery, and answer all of your questions. This informative consultation takes place in a discreet, professional office environment, convenient to most localities.
Resources
- Webster, G. .V Gynecomastia in the Navy. The Military Surgeon November 1944.
- Carlson, H. E. Gynecomastia. N. Engl. .J Med. 303: 795, 1980.
- Nuttall, F. Q. Gynecomastia as a physical finding in normal men. .J Clin. Endocrinol. Metab. 48: 338, 1979.
- Williams, M. .J Gynecomastia: Its incidence, recognition and host characterization in 47 autopsy cases. Am. .J Med. 34: 103, 1963.
- Nydick, M,. Bustos, ,.J Dale, J. H,. and Rawson, R. W. Gynecomastia in adolescent boys. J.A.M.A. 178: 449, 1961.
- Cohen, .I K,. Pozez, .A,L. and McKeown, .J E. Gyneco- mastia. In E. H. Courtiss (Ed.), Mael Aesthetic Surgery. St. Louis: Mosby, 1991.
- Neuman, .J .F Evaluation and treatment of gynecom- astia. Am. Fam. Physician 5: 1835, 1997.
- Teimourian, B,. and Pearlman, R. Surgery for gyneco- mastia. Aesthetic Plast. Surg. 7: 155, 1983.
- Courtiss, .E H. Gynecomastia: Analysis of 159 patients and current recommendations for treatment. Plast. Reconstr. Surg. 79: 740, 1987.
- Rosenberg, G. .J Gynecomastia: Suction lipectomy as a contemporary solution. Plast. Reconstr. Surg: 80: 379, 1987.
- Rohrich, R. ,.J Beran, S. ,.J and Kenkel, .J M. Ultrasound- Asisted Liposuction. S.t Louis: Quality Medical Publish- ing, 1998,
- LaFranchi, .S H,. Parlow, .A ,F. Lippe, B. M., Coyotupa, ,.J and Kaplan, S. .A Pubertal gynecomastia and transient elevation of serum estradiol level. Am. .J Dis. Child 129: 927, 1975.
- Large, D. M,. Anderson, D. ,C. and Laing, .I Twenty- four hour profiles of serum prolactin during male puberty with and without gynaecomastia. Clin. Endo- crinol. (Ox/.) 12: 293, 1980.
- Farthing, M. J.,Green, .J R,. Edwards, .C R,. and Dawson, .A М. Progesterone, prolactin, and gynaecomastia in m e n with liver disease. Gut 23: 276, 1982.
- McFadyen, .I ,.J Bolton, .A ,E. Cameron, .E H., Hunter, W. M,. Raab, G,. and Forrest, .A P. Gonadal-pituitary hormone levels in gynaecomastia. Clin. Endocrincol. (Oxf.) 13: 7, 1980.
- Treves, .N Gynecomastia: The origins of mammary swelling of the male. Cancer 1: 1083, 1958.
- Glass, .AR,. and Berenberg, J. Gynecomastia after che- motherapy for lymphoma. Arch. Intern. Med. 139: 1048, 1979.
- Trump, D. ,L. Pavy, M. D,. and Staal, .S Gynecomastia in men following anti-neoplastic therapy. Arch. Intern. Med. 142: 51, 1982.
- Bannayan, G. ,A. and Hajdu, S. .I Gynecomastia: Clin- icopathologic study of 351 cases. Am. .J Clin. Pathol. 57: 431, 1972.
- Jackson, .A W., Muldal, S,. Ockey, .C H,. and O’Connor, P. .J Carcinoma of male breast in association with the Klinefelter syndrome. B.r Med. .J 1: 223, 1965.
- Simon, B. E., Hoffman, S,. and Kahn, .S Classification and surgical correction of gynecomastia. Plast. Recon- str. Surg. 51: 48, 1973.
Rohrich, R.J., Ha, R.Y., Kenkel, J.M. and Adams Jr, W.P., 2003. Classification and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plastic and reconstructive surgery, 111(2), pp.909-923