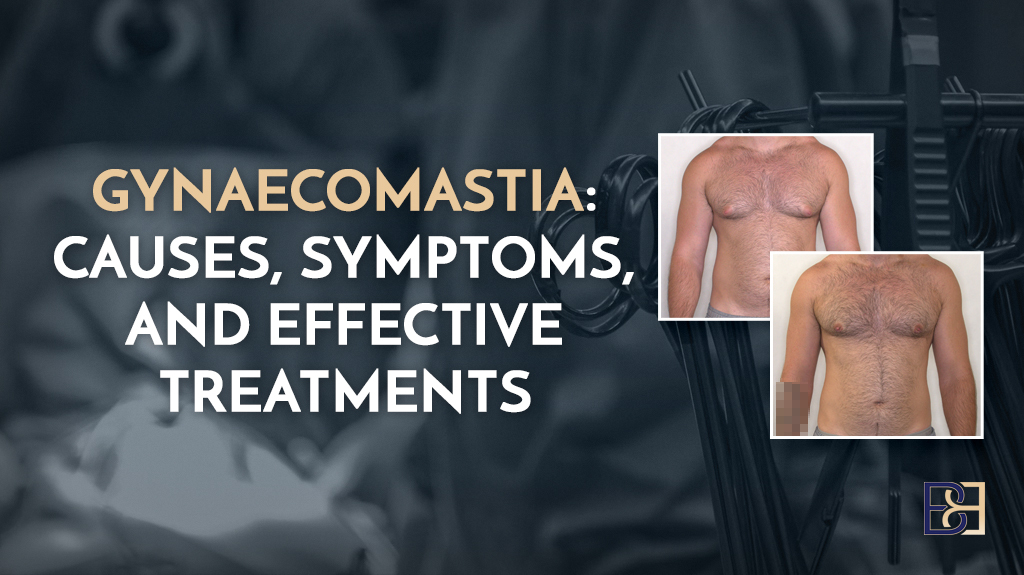
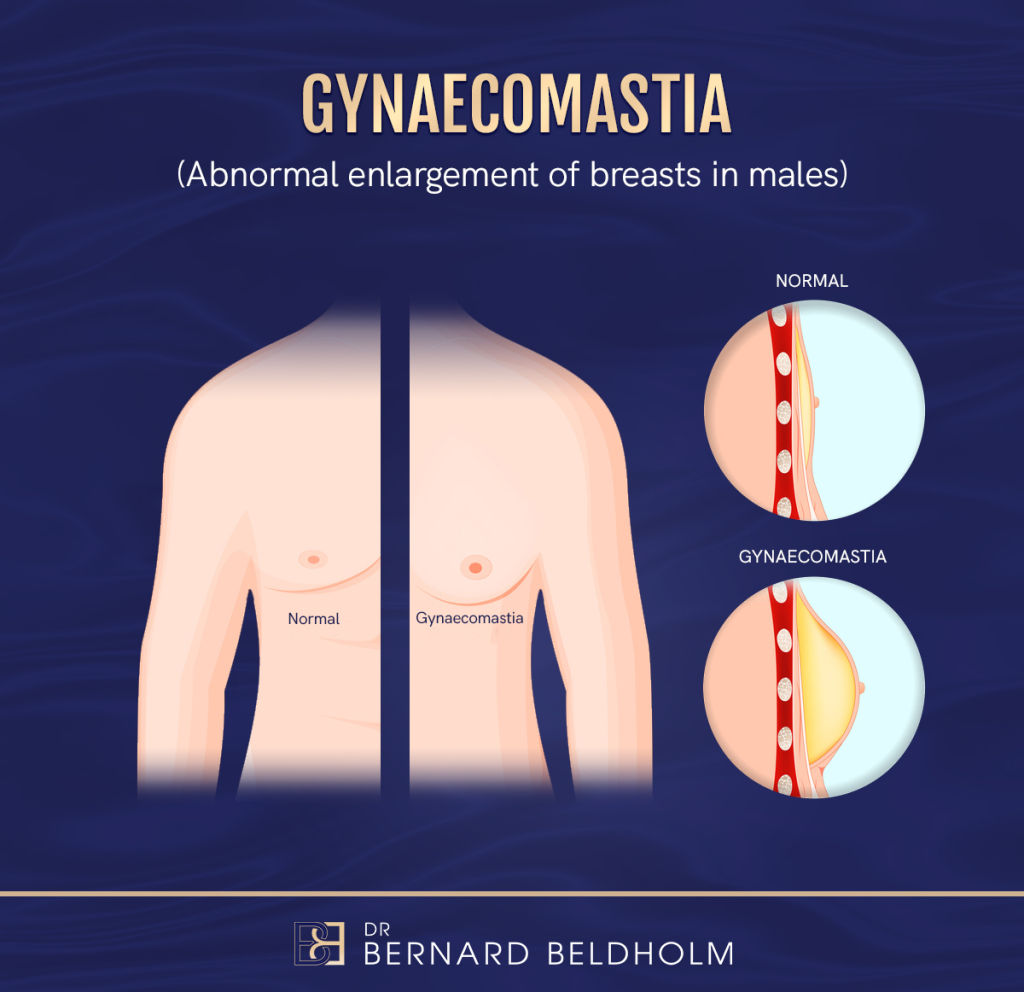
Gynaecomastia is the enlargement of male breast tissue and is commonly classified into grades based on the patient and complexity of the condition. From enlarged breasts with elastic skin to ptotic breasts with inelastic skin, gynaecomastia affects men of all ages and all stages of life.
Classification Systems
Over the years, several classification systems have been developed to help surgeons determine the grade of the cognition and the best treatment possible.
Book your appointment online now
Why Classification Systems Were Created
Classification systems for gynaecomastia, were developed for several reasons:
1. Differentiating Between True Gynaecomastia and Pseudogynaecomastia
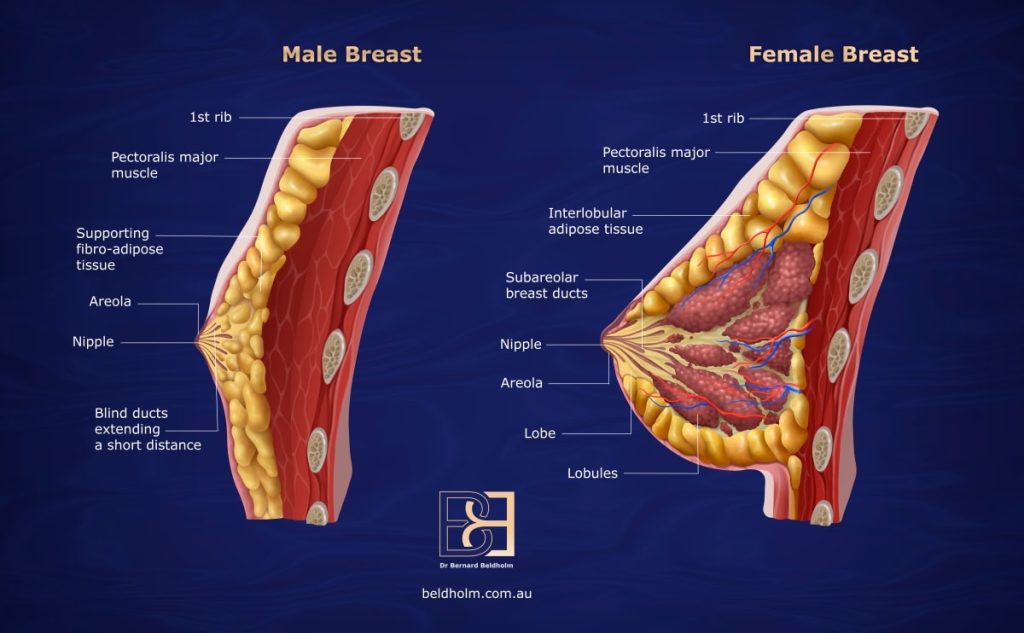
True Gynaecomastia is caused by an overdevelopment of glandular breast tissue that is often triggered by a hormonal imbalance, causing oestrogen levels to become elevated relative to testosterone. The chests of men with this condition become more prominent due to the growth of glandular tissue beneath the nipple, leading to a feminine appearance. For some men, the condition resolves on its own; however, for others, advanced treatments may be required.
Pseudogynaecomastia, on the other hand, is caused by an accumulation of fat in the chest area, which is often related to weight gain or obesity.
The chests of men with this condition experience a breast enlargement that is much softer and more diffuse, as it is more consistent with fatty deposits. Though some exercises that tone the chest help some men with this condition, the most effective way to treat pseudogynaecomastia is with suction-assisted lipectomy (liposuction).
Though physicians often determine which type of gynaecomastia a patient is experiencing with physical exams and/or ultrasound, the vast majority of men with the condition have both excess fat and glandular tissue.
2. To Create Grading Systems Standardised Diagnoses and Treatment Plans Among Surgeons
Gynaecomastia can have various underlying causes, including puberty, ageing, medication side effects, and hormonal imbalances. Classification systems assist surgeons to categorise the condition by providing standardised diagnoses and treatment plans.
Grading Systems, such as the Ratnam grading scale, classify the severity of gynaecomastia based on the degree of tissue enlargement and skin excess. This helps guide whether surgical intervention is needed and which type of surgery is appropriate suction-assisted lipectomy (liposuction), excision, or a combination.
3. To Streamline Communication Between Specialists
Surgeons, endocrinologists, and other healthcare providers need a clear, standardised way of communicating the condition’s severity, underlying causes, and treatment recommendations. Classification systems provide this common language, ensuring that patient care is coordinated efficiently.
4. To Optimise Surgical Outcomes
By using standardised classification systems, surgeons can better plan for individualised treatment. Some systems help decide whether to perform suction-assisted lipectomy (liposuction), excision of glandular tissue, or skin tightening procedures, depending on the type of gynaecomastia and the patient’s specific anatomy.
5. To Prevent Misdiagnosis and Unnecessary Interventions
Not all cases of male breast enlargement are due to gynaecomastia. By using classification systems, physicians can avoid unnecessary surgeries or treatments by identifying cases of pseudogynaecomastia or conditions like breast cancer in males.
These systems may assist in improving diagnostic accuracy, supporting appropriate treatment decisions, and helping to reduce the risk of unnecessary interventions.
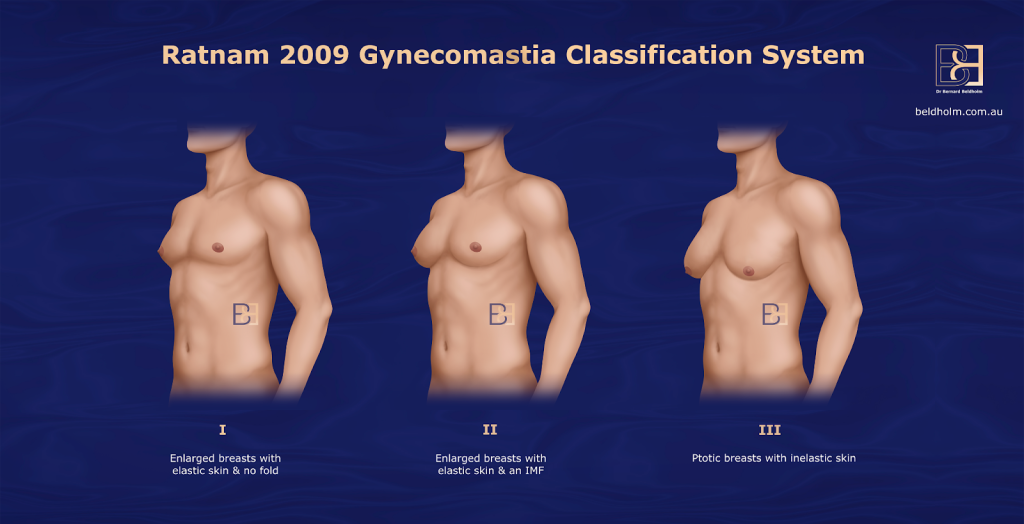
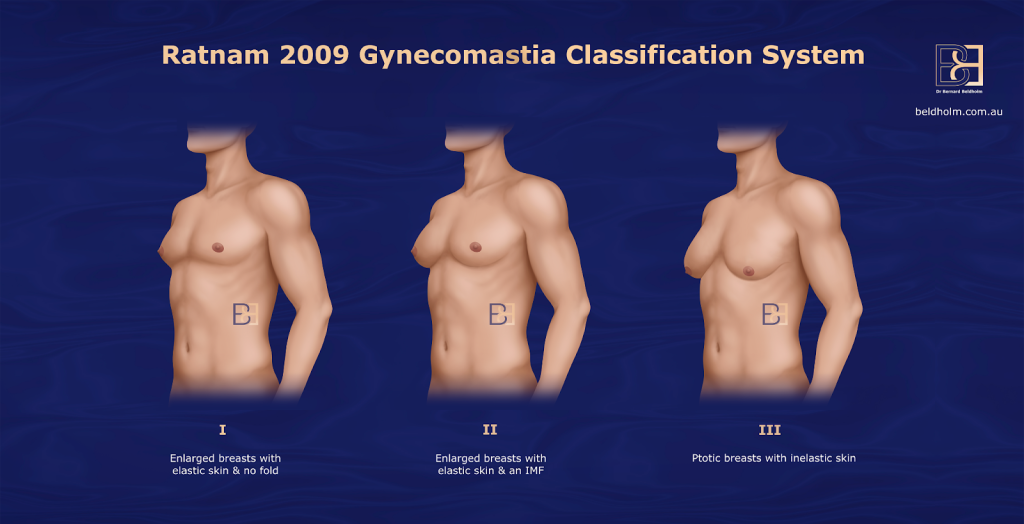
Ratnam Gynaecomastia Classification
Acknowledging that it is not uncommon for patients to be dissatisfied after their gynaecomastia surgery, a study was conducted over the course of 3 years (January 2005 to December 2007) by B. Venkata Ratnam, MBBS, MS(Orth), MCh(Plast) Plastic surgeon involving 42 participants, each with their own pre-existing conditions, level of gynaecomastia severity, and age, among other factors. The study concluded that four individual causes of patient dissatisfaction following treatment for gynaecomastia were identified and their probable causes were analysed. They included:
- Residual gynaecomastia
- Persistence of an IMF sharply demarcating the chest from the abdomen
- Persistence of loosely hanging breast skin
- Unsightly scars
Based on these findings, a new classification and treatment protocol was developed.
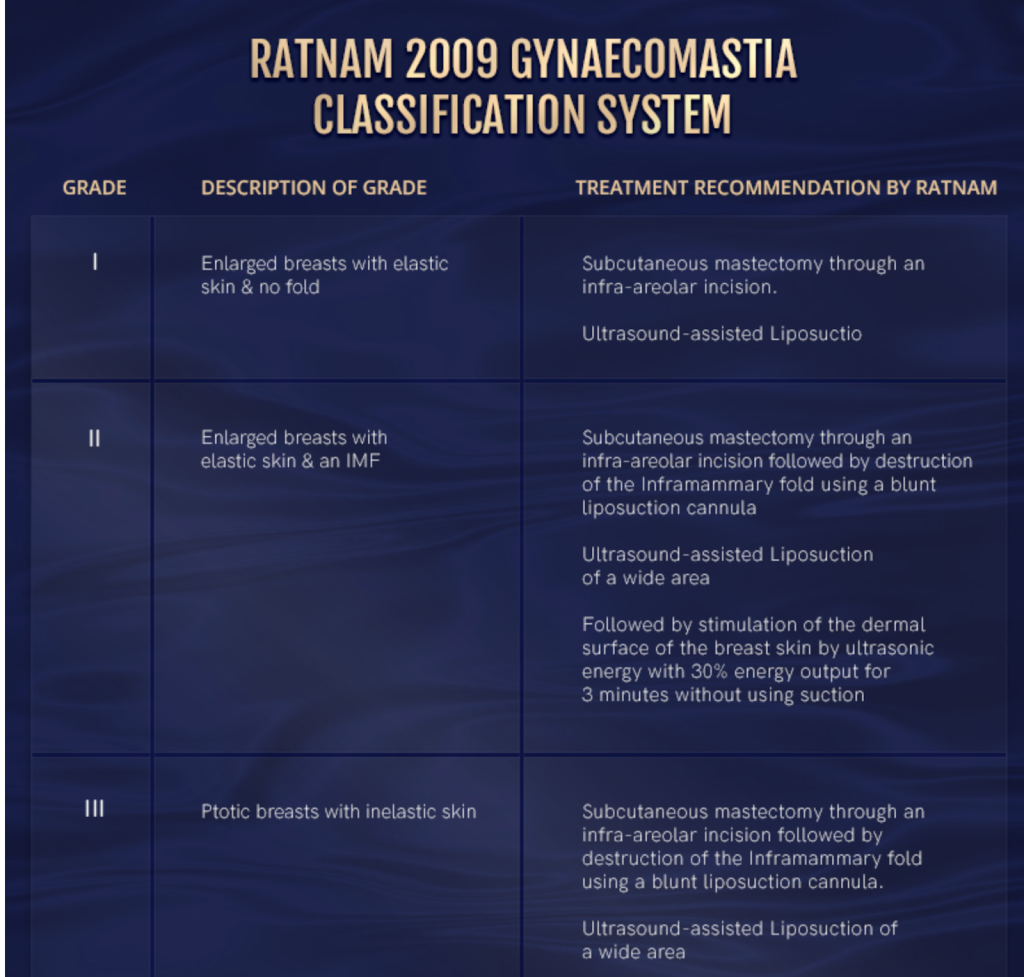
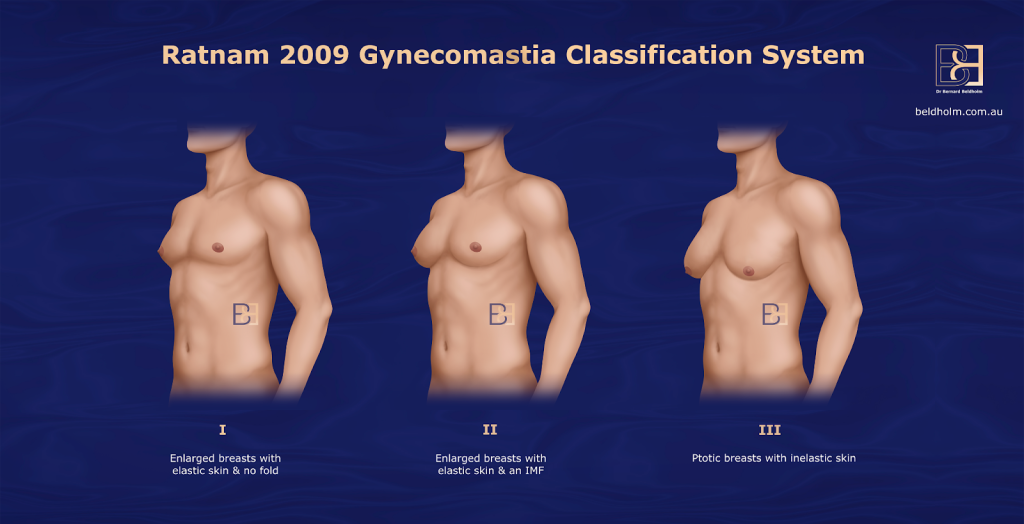
The Ratnam (plastic surgeon in India) classification, developed in 2009, helps guide surgeons in tailoring their surgical approach based on the severity of the condition, with increasing complexity as the grade progresses. This system focuses on the amount of excess glandular tissue and skin, helping surgeons determine the best approach for treatment.
By considering the amount of tissue and skin excess, the system aims to achieve more aesthetically pleasing and symmetrical results, while also minimising scarring and other complications.
Ratnam 2009 Gynaecomastia Grading System
Grade I (Minor Gynaecomastia)
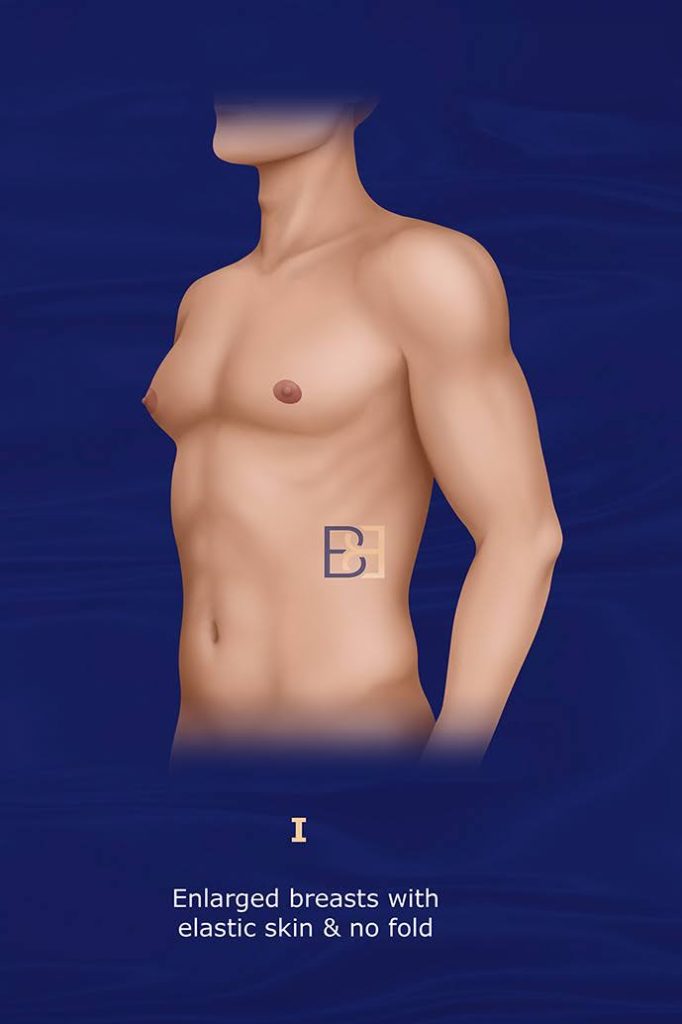
Presentation:
Enlarged breasts with elastic skin and no fold
Treatment:
- Subcutaneous mastectomy through an infra-areolar incision.
- Ultrasound-assisted liposuction.
Grade II (Moderate Gynaecomastia)
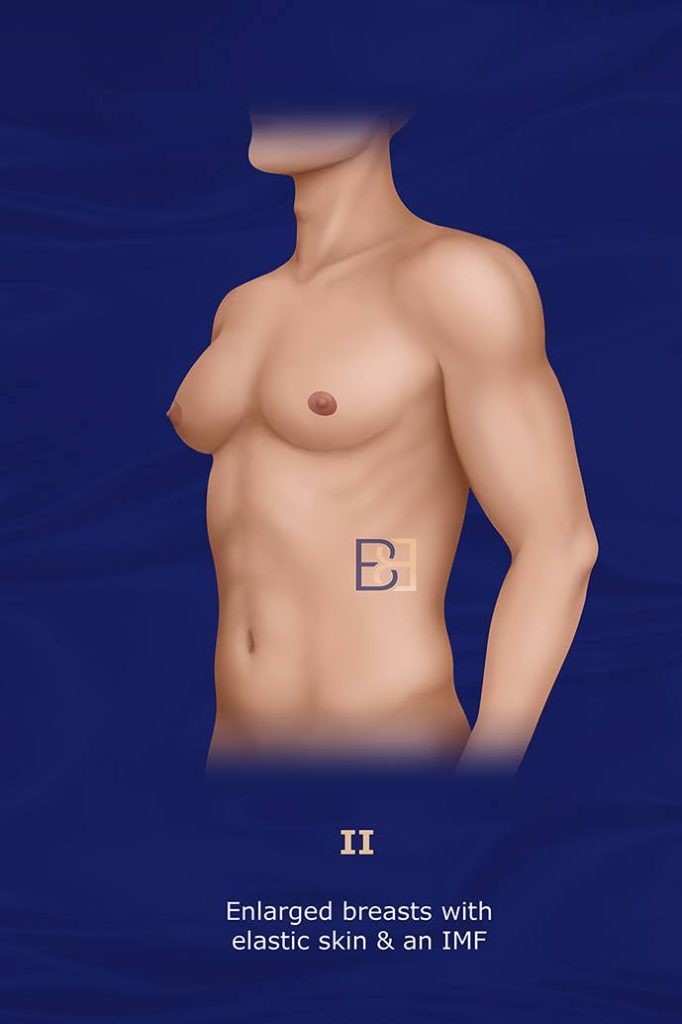
Presentation:
Enlarged breasts with elastic skin and IMF (Inframammary Fold)
Treatment:
- Subcutaneous mastectomy through an infra-areolar incision
- Destruction of the Inframammary fold using a blunt liposuction cannula.
- Ultrasound-assisted liposuction of a wider area.
- Stimulation of the dermal surface of the breasts using ultrasonic energy at 30% output for 30 minutes without suction.
Grade III (Severe Gynaecomastia)
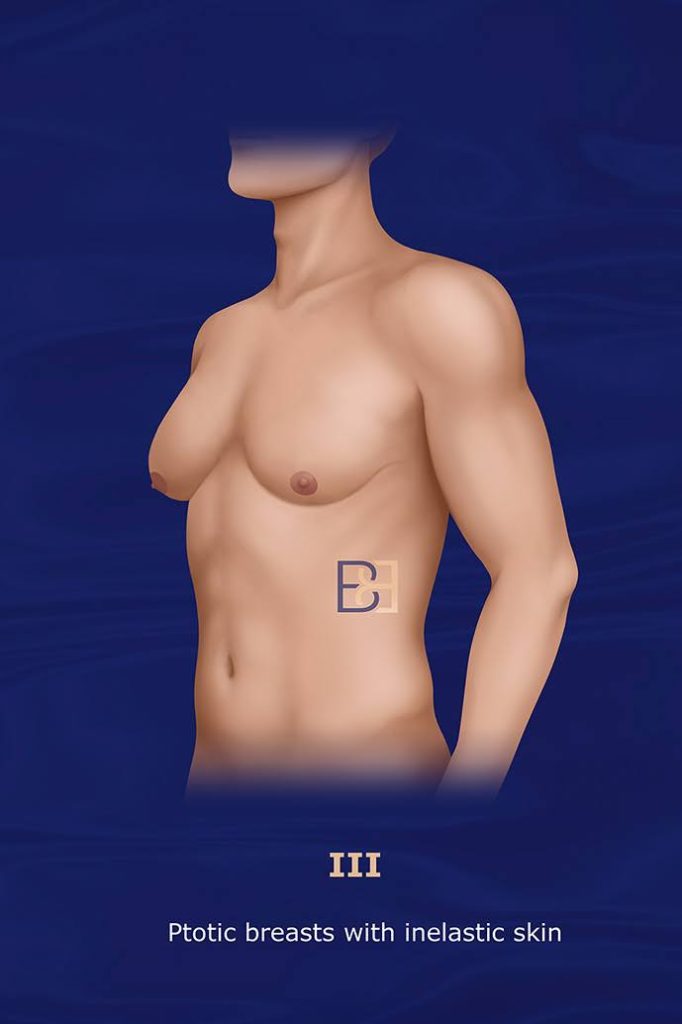
Presentation:
Ptotic breast enlargement with inelastic skin and significant skin excess, resembling female breasts (macromastia).
Treatment:
- Subcutaneous mastectomy through an infra-areolar incision. Destruction of the Inframammary fold using a blunt liposuction cannula.
- Ultrasound-assisted liposuction of a wider area.
- Stimulation of the dermal surface of the breasts using ultrasonic energy at 30% output for 30 minutes without suction.
- Reduction of redundant skin sleeve by periareolar de-epithelization and purse-string closure of wounds around areola.
Advantages of the Ratnam Classification System
The Ratnam Classification System for gynaecomastia has several advantages over earlier classification systems, which make it particularly useful in modern clinical practice. Here are some of the key advantages:
1. More Comprehensive Assessment of Skin Redundancy
Earlier systems, such as the Simon Classification, focus primarily on the size of the glandular tissue and the degree of breast enlargement, not the amount of skin excess or ptosis as thoroughly.
By incorporating skin excess and its impact on surgical planning, the Ratnam system offers a more comprehensive assessment, which is especially important in moderate to severe cases (Grades II and III), where skin redundancy can significantly influence the choice of treatment.
2. Better Surgical Planning
Older systems that focus solely on gland size might not provide sufficient guidance for planning more complex surgeries that involve skin excision or repositioning.
Because the Ratnam system explicitly accounts for skin excess, it allows for better preoperative planning. Surgeons can tailor their approach, combining liposuction, gland excision, and skin tightening when necessary, leading to more refined and individualised treatment.
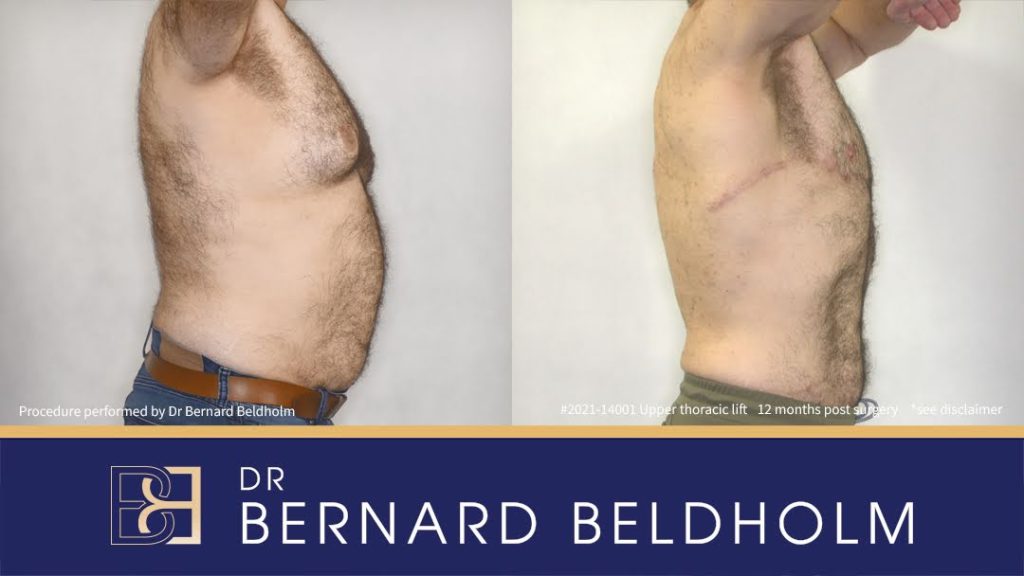
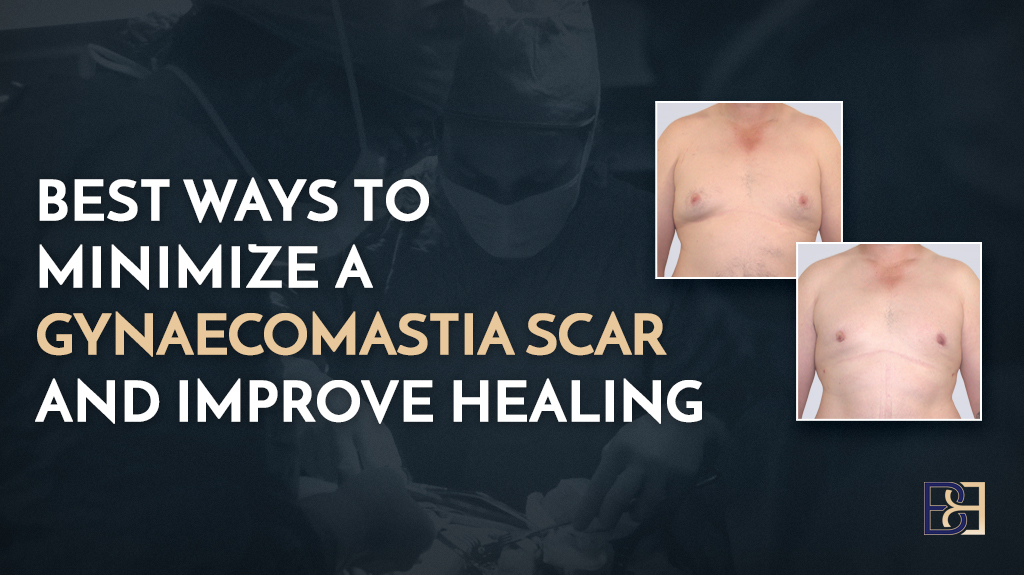
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
3. Management of Severe Cases
Some earlier systems may treat severe cases inadequately (i.e., large breasts with ptosis), which can lead to incomplete correction or poor aesthetic results.
The Ratnam Classification system emphasises the need for more involved procedures in Grade III cases, such as skin excision and repositioning of the nipple-areola complex. These procedures are essential for treating the ptosis and excess skin common in severe gynaecomastia.
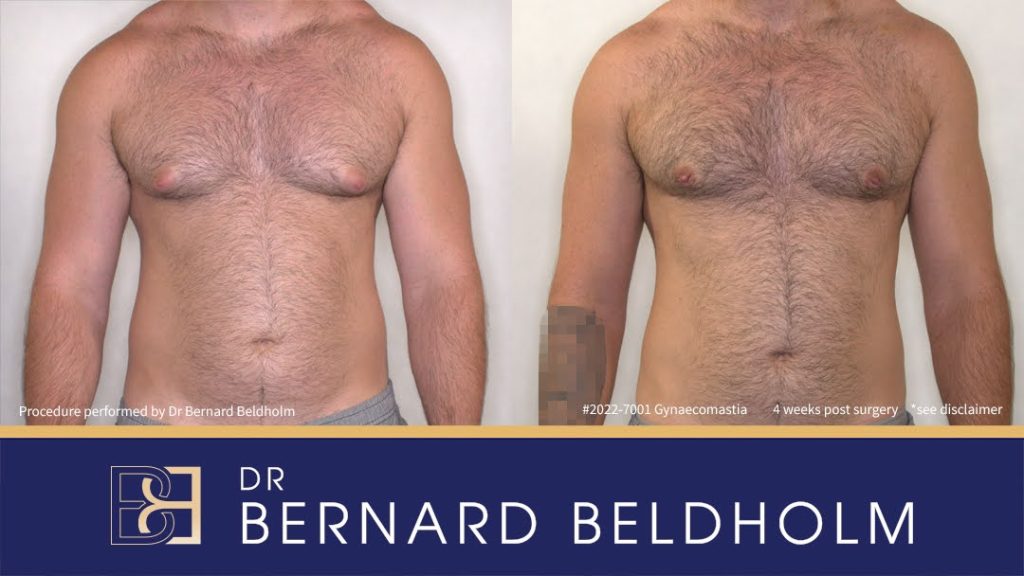
Tattoo blurred for privacy
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
4. Focus on Cosmetic Outcomes
Older systems may be more focused on clinical classification without necessarily guiding surgeons toward achieving optimal cosmetic outcomes.
The Ratnam system’s detailed focus on both glandular and skin components, achieving better outcomes with less visible scarring.
5. Streamlined and Straightforward
Most of the earlier classification systems are more complex or rigid in categorising gynaecomastia.
The Ratnam Classification provides a straightforward, yet detailed, three-grade scale that is practical for use in clinical practice. This approach helps streamline communication between providers and offers clear guidance for treatment selection.
6. Tailored to Modern Surgical Techniques
Many earlier Systems were developed before the use of advanced suction-assisted techniques or skin-tightening procedures. The Ratnam Classification accounts for modern surgical techniques, including the use of liposuction, glandular excision, and skin management, making it more adaptable to contemporary surgical solutions.
The Ratnam Classification System built upon older systems by integrating the assessment of skin redundancy, offering better surgical planning, particularly in severe cases, and facilitating a more personalised and aesthetically focused approach to gynaecomastia treatment.
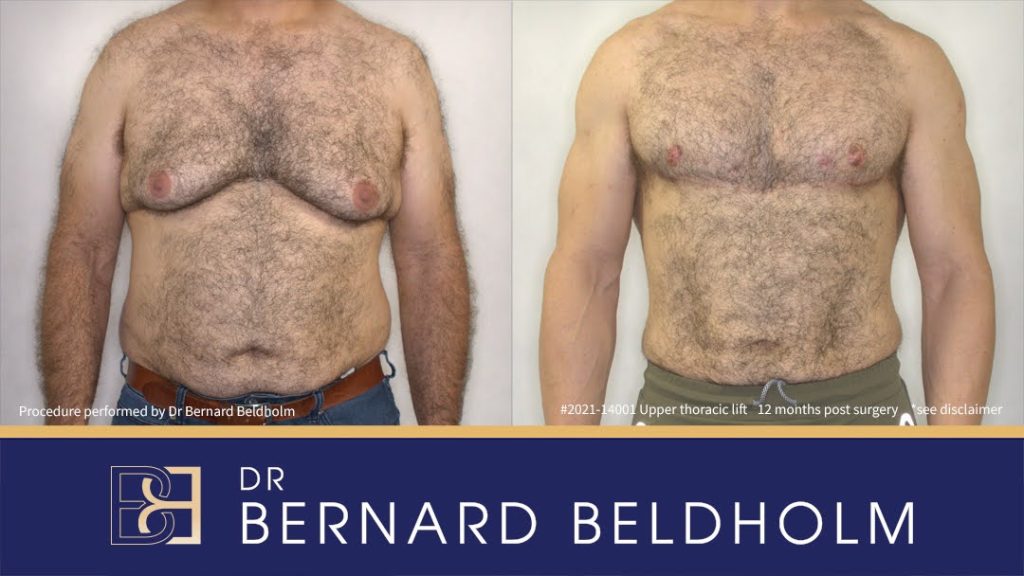
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Dr. Beldhom’s Thoughts on the Ratnam Classification System
Earlier systems, such as the Simon Classification, focus primarily on the size of the glandular tissue and the degree of breast enlargement, but do not address the amount of skin excess or sagging (ptosis) as thoroughly.
By incorporating skin excess and its impact on surgical planning, the Ratnam system offers a more comprehensive assessment, which is especially important in moderate to severe cases (Grades II and III), where skin redundancy can significantly influence the choice of treatment.
Dr Beldholm Overall Opinion of the Ratnam Study
- The treatments that they offered for skin reduction was circular reduction of the areola with no other radical excision offered. Gynaecomastia patients with significantly ptotic breasts and loose skin are likely to not be adequately treated with a circular excision of skin.
- There is no mention of “puffy nipple” or small gynaecomastia that can be treated by excision only.
- The classification of an IMF fold as being abnormal in a male I find anatomically incorrect. In a normal male without defined muscles there may not be a fold. However in a muscular male there is a fold. Trying to remove the fold will make these men look worse.
- There is not enough of a sample to be able to conclude what the authors concluded.
Book your appointment online now
Resources
- Nydick M, Bustos J, Dale JH Jr, Rawson RW. Gynecomastia in adolescent boys. JAMA 1961;178:449–454.
- Simon BE, Hoffman S, Kahn S. Classification and surgical correction of gynecomastia. Plast Reconstr Surg 1973;51:48–52.
- Deutinger M, Freilinger G. Gynecomastia: attempt at a classification and surgical results. Handchir Mikrochir Plast Chir 1986;18:239–241 (in German).
- Rosenberg GJ. Gynecomastia: suction lipectomy as a contemporary solution. Plast Reconstr Surg 1987;80:379–386.
- Rohrich RJ, Ha RY, Adams WP, Mladick RA. Classification and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plast Reconstr Surg 2003;111:909–925.
- Mladick RA. Gynecomastia. Aesthetic Surg J 2004;24:471–479.
- Filho DH, Arruda R, Alonso N. Treatment of severe gynecomastia (Grade III) by resection of periareolar skin. Aesthetic Surg J 2006;26:669–673.
- Webster JP. Mastectomy for gynecomastia through a semicircular intra-areolar incision. Ann Surg 1946;124:557–575.
- Pitman GH. Breast and chest wall. In: Pitman GH, editor. Liposuction and aesthetic surgery. St. Louis: Quality Medical Publishing; 1993. P.197–209.
- LaTrenta GS, Hoffman LA. Breast reduction. In: Rees TD, LaTrenta GS, editors. Aesthetic plastic surgery, 2nd ed. Philadelphia: W.B. Saunders Company; 1994. p. 926–1002.
- Spear SL. Gynecomastia (commentary). In: Spear SL, editor. Surgery of the breast: principles and art, 1st ed. New York: Lippincott-Raven; 1998. p. 841.
- Cordova A, Moschella F. Algorithm for clinical evaluation and surgical treatment of gynaecomastia. J Plast Reconstr Aesthet Surg 2008;61:41–49.
- Rosenberg GJ. Gynecomastia. In: Spear SL, editor. Surgery of the breast: principles and art, 1st ed. New York: Lippincott-Raven; 1998. p. 831–841.
- Rohrich RJ, Beran SJ, Kenkel JM, editors. Ultrasound-assisted liposuction. St. Louis: Quality Medical Publishing; 1998. p. 312–321.
- Rohrich RJ, Beran SJ, Kenkel JM, editors. Ultrasound-assisted liposuction. St. Louis: Quality Medical Publishing; 1998. p. 142–143.
- Benelli L. A new periareolar mammoplasty: the “round block” technique. Aesthetic Plast Surg 1990;14:93–100.
- Benelli LC. Periareolar Benelli mastopexy and reduction: the “round block.” In: Spear SL, editor. Surgery of the breast: principles and art. 1st ed. New York: Lippincott-Raven; 1998. p. 685–696.
- Davidson BA. Concentric circle operation for massive gynecomastia to excise the redundant skin. Plast Reconstr Surg 1979;63:350–354.
- Smoot EC 3rd. Eccentric skin resection and purse-string closure for skin reduction with mastectomy for gynecomastia. Ann Plast Surg 1998;41:378–383.
- Persichetti P, Berloco M, Casadei RM, Marangi GF, Di Lella F, Nobili AM. Gynecomastia and the complete circumareolar approach in the surgical management of skin redundancy. Plast Reconstr Surg 2001;107:948–954.
- Mathes SJ, Seyfer AE, Miranda EP. Congenital anomalies of the chest wall. In: Mathes SJ, editor. Plastic surgery, 2nd ed. Philadelphia: Saunders Elsevier; 2006. p. 527–533.
- Lista F, Ahmad J. Power-assisted liposuction and the pull-through technique for the treatment of gynecomastia. Plast Reconstr Surg 2008;121:740–747.
- Ratnam, B.V., 2009. A new classification and treatment protocol for gynecomastia. Aesthetic Surgery Journal, 29(1), pp.26-31