A 30 year old male, who suffered with gynaecomastia for six years, presented with a hard, rubbery feeling under his nipple, causing him severe discomfort. I performed a subcutaneous mastectomy for bilateral gynaecomastia or excess breast tissue, the operation included suction-assisted lipectomy (VASER Liposuction). This operation removes excess breast tissue.
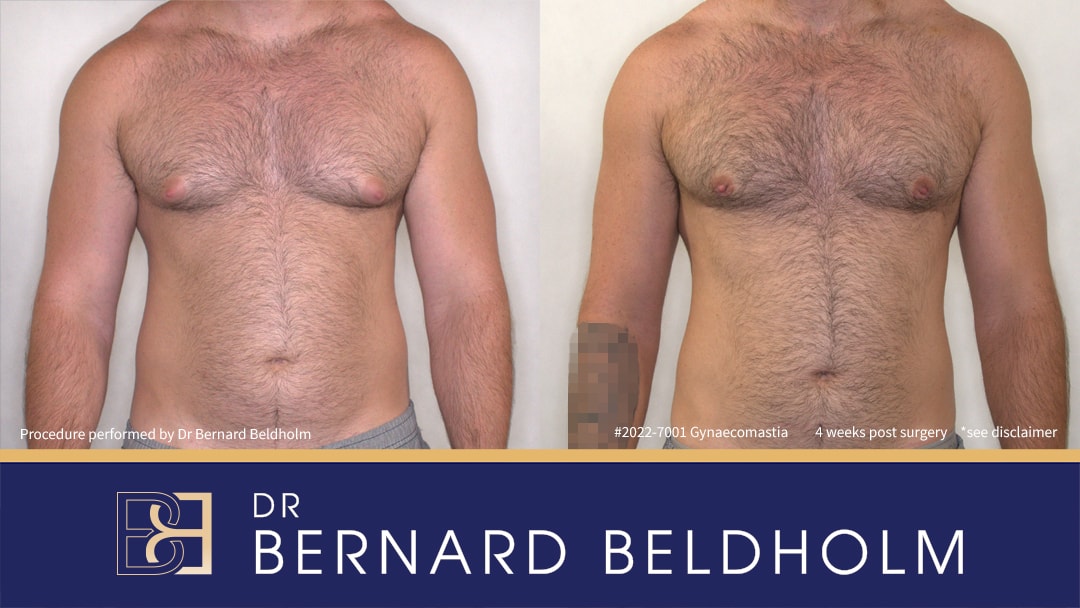
Tattoo blurred (right arm in post surgery image) for privacy
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Book your appointment online now
Indications to Remove Excess Breast Tissue in This Patient
A 30-year-old male experiencing discomfort presented with a firm, rubbery feeling beneath the nipples. This condition persisted for 6 years despite attempts to lose weight through diet and exercise.
On examining the glandular tissue, he had a moderately firm gland that extended past the areola. There was only minimal excess fatty tissue present in this patient.
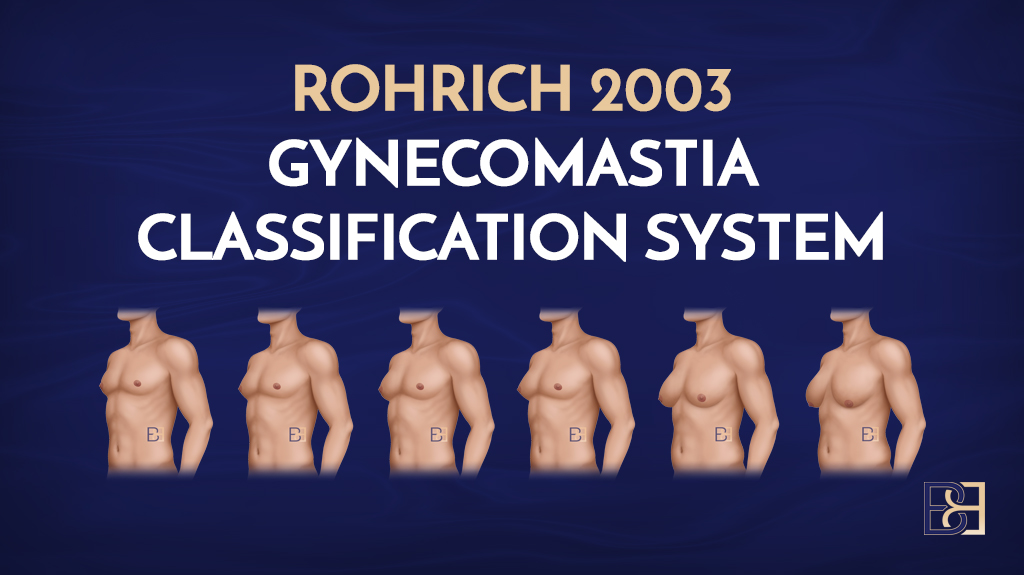
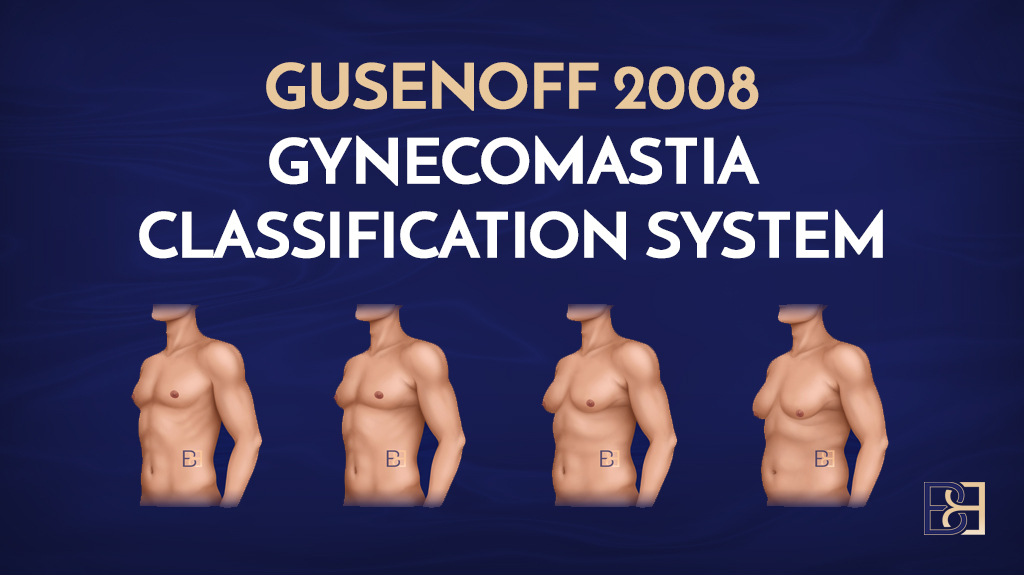
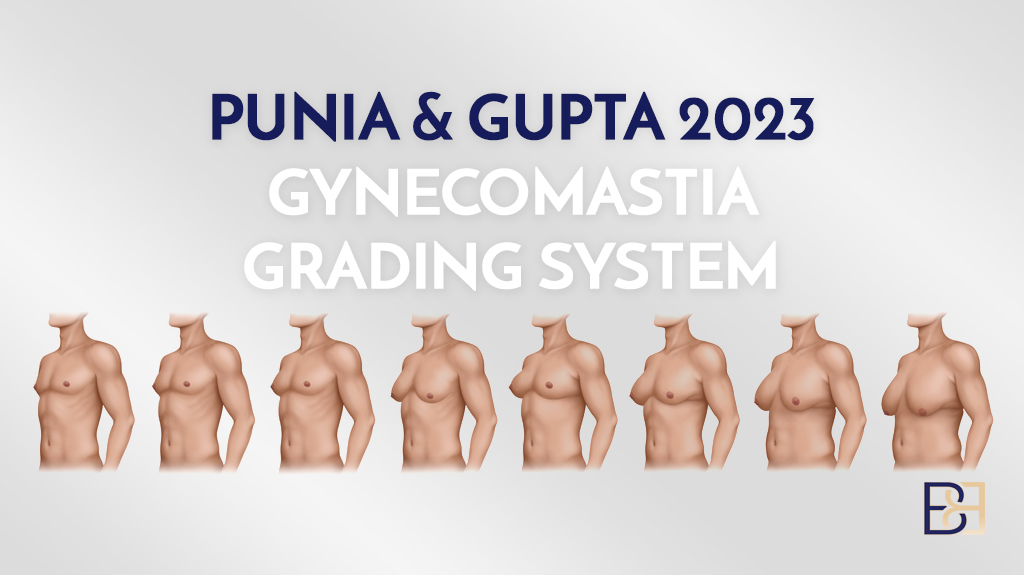
I classified his grade of gynaecomastia as grade BB 2a according to the Beldholm gynaecomastia classification system.
Histology Report of the Glandular Tissue
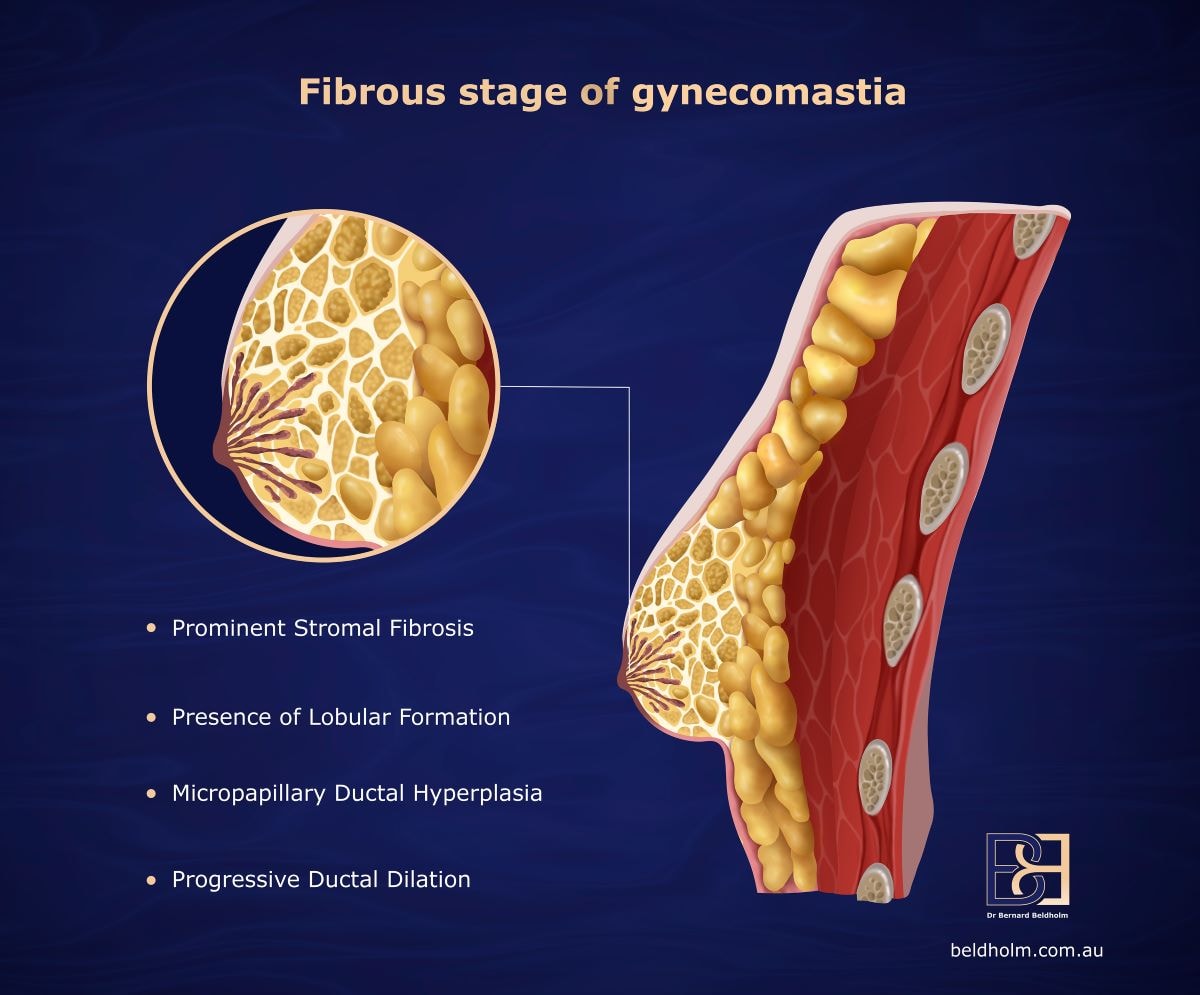
Dr. Beldholm always sends the tissue removed with the surgery for gynaecomastia to a pathologist for examination to rule out conditions such as male breast cancer. This patient had fibrous stage of gynaecomastia.
MACROSCOPIC FINDINGS of the glandular tissue
- RIGHT BREAST TISSUE: The specimen consisted of a piece of fibroadipose breast tissue without overlying skin measuring 52x50x21mm and weighing 21g. The cut surface showed uniform fibroadipose breast tissue. No focal lesions were seen.
- LEFT BREAST TISSUE: The specimen consisted of a piece of fibroadipose breast tissue without overlying skin measuring 63x48x34mm and weighing 31g. The cut surface shows uniform fibroadipose breast tissue. No focal lesions were seen.
MICROSCOPIC FINDINGS of the glandular tissue
- RIGHT BREAST TISSUE : Sections showed breast tissue with numerous ducts including few
dilated ducts and patchy apocrine metaplasia. There was no evidence of
in situ or invasive malignancy. - LEFT BREAST TISSUE: Sections showed breast tissue with numerous ducts and patchy apocrine
metaplasia. There was no evidence of in situ or invasive malignancy.
Dr Beldholm’s Approach to Subcutaneous Mastectomy Including suction-assisted lipectomy (VASER Liposuction) for Stage 2a Gynaecomastia
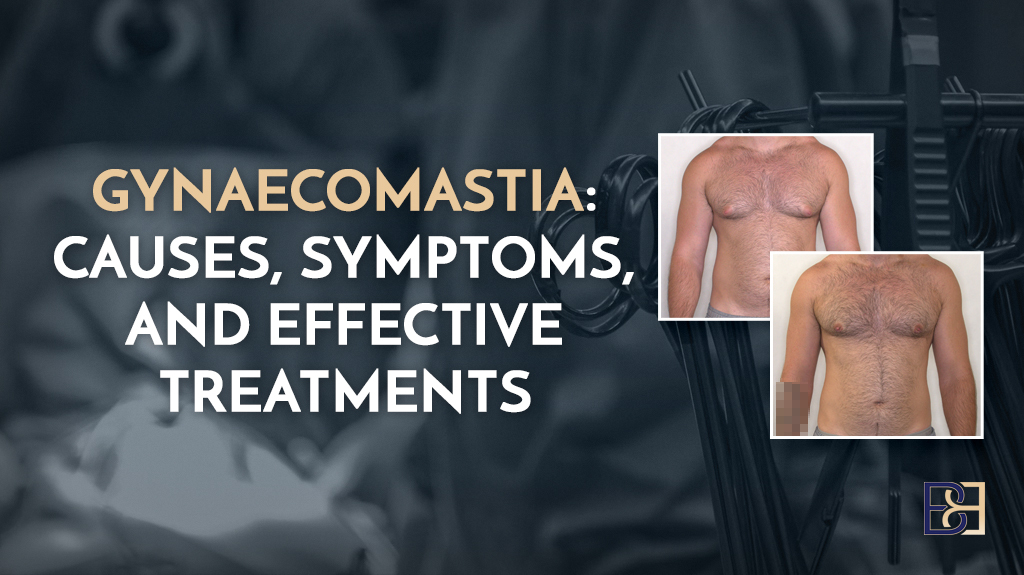
Gynaecomastia affecting men of all ages, from adolescence to senior years, experts say as many as 50% of men experience symptoms of gynaecomastia.
Characterised by the enlargement of breast tissue in males, the condition is commonly caused by an enlarged chest gland and an imbalance of the hormones oestrogen and testosterone. While the condition, which can affect either one breast or both breasts, is often harmless, it may cause discomfort or emotional distress.
Fortunately, various treatments, including certain drugs, lifestyle changes, non-surgical regimens, and surgery are available to treat this issue, making a more masculine chest appearance possible.
Male breast reduction surgery, a procedure that’s been improving the lives of many men suffering with this condition.
What Causes Gynaecomastia?
Men develop gynaecomastia for a variety of reasons, with hormonal changes being the most prevalent cause. Commonly caused by an imbalance between oestrogen and testosterone levels, however, understanding the underlying cause is crucial for determining the appropriate treatment for gynaecomastia. For more information about the causes and symptoms of gynaecomastia and available treatments, read my article, Gynaecomastia: Causes, Symptoms, and Effective Treatments.
What is Gynaecomastia Surgery with VASER Liposuction (Suction-assisted lipectomy)?
Often a preferred treatment for gynaecomastia because it provides immediate and noticeable results, surgery for gynaecomastia, also known as male breast reduction, involves removing excess glandular tissue and fat to achieve a flatter chest profile. This surgery may also include suction-assisted lipectomy (VASER Liposuction).
Gynaecomastia surgery involves cutting out the chest gland and shaping a square, masculine chest using suction-assisted lipectomy (VASER Liposuction).
An effective way to treat enlarged male breasts is through surgery. After the surgical procedure itself, the chances of gynaecomastia recurring are low, with a rate of around 10% in the literature.
Two-Fold Benefits of Gynaecomastia Surgery
- The removal of the chest gland stops breast growth.
- The removal of excess fat with the use of suction-assisted lipectomy (VASER Liposuction) results in a flatter, and well-defined chest shape with a more masculine appearance.
*The reason I incorporate VASER Liposuction (Suction-assisted lipectomy) into the gynaecomastia procedure is that simply removing the gland can cause saucer deformity. Once the gland, which is located behind the nipple, is removed, the nipple may dent inward. By using liposuction and removing fat with VASER, I was able to reshape the tissue around the gland, and reduce the risk of saucer deformity. VASER also enables me to remove fat to define the pectoral muscles, resulting in a more defined, square shape, the hallmark of a masculine chest.
How I do it: Subcutanous Mastectomy (male breast reduction) for Gynaecomastia with suction-assisted lipectomy (VASER Liposuction) for Dr Beldholm’s Patient #2022-7001
Preparing the Patient for Gynaecomastia Surgery
Greeting in Anaesthetic Bay
I greeted my patient in the anesthetic bay to go over all the final details of his procedure. While the patient and I had plenty of time to discuss his wishes and expectations prior to the surgery day, many patients feel a bit nervous just before surgery. This meeting allowed the patient to voice any lingering concerns and ask me last-minute questions before the surgery began.
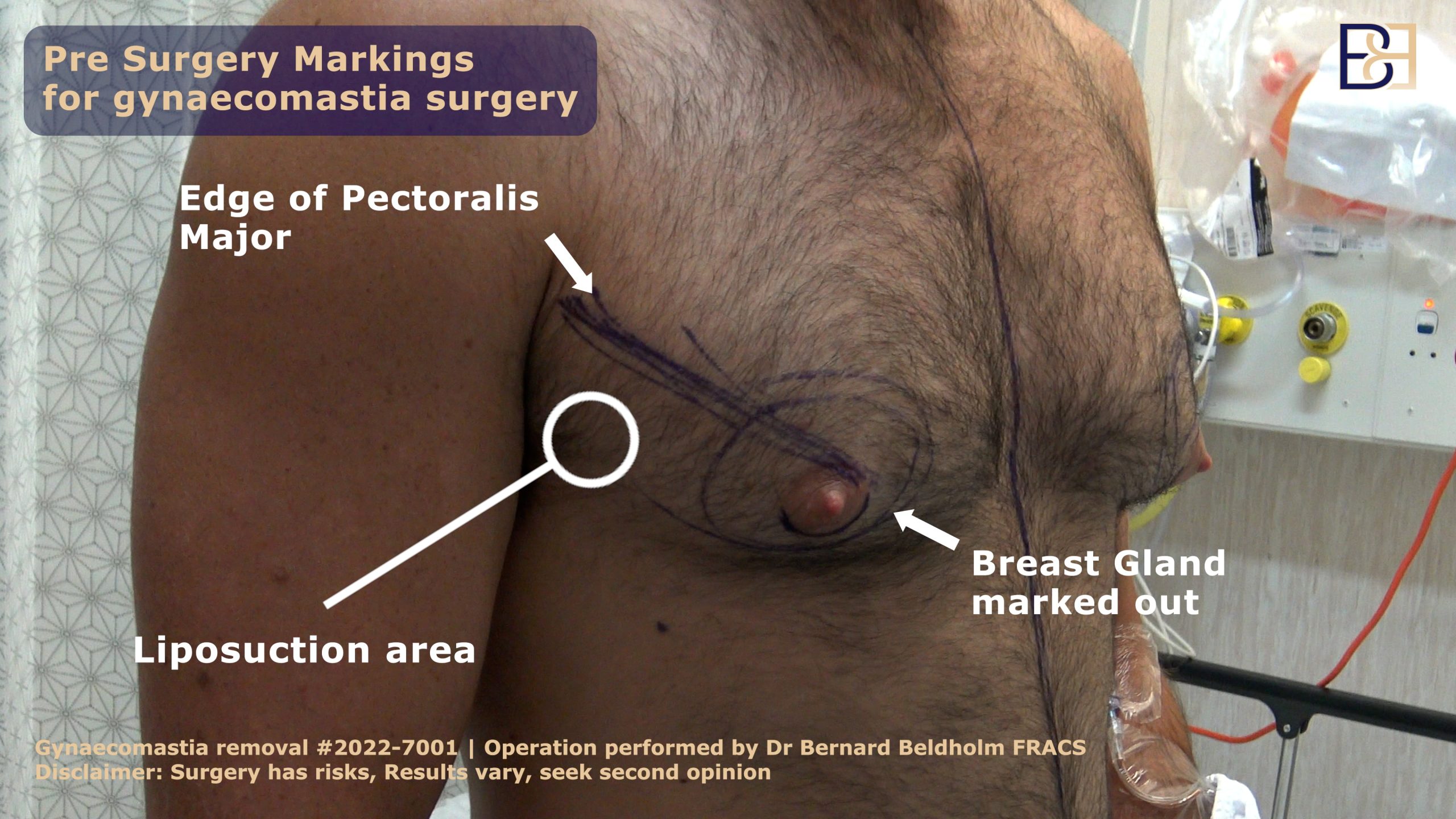
Initial Markings Made
Once I had some time to meet with the patient to alleviate any last minute concerns, I began prepping the patient by making initial markings, after which, the anaesthetist administered the pre-medication.
Operating Room
After the initial marketings were made, the patient was moved to the operating room. While laying on the operating table, the anaesthetist delivered the anaesthesia.
Anaesthesia and Intubation for Male Breast Reduction

As with all gynaecomastia procedures, this surgery was performed using a general anaesthetic. A highly trained anesthesiologist placed a mask over the patient’s mouth to provide oxygen while the surgery was being performed. A breathing tube was inserted to help the patient breathe during the operation. This process is known as intubation.
Once the patient was sedated and intubated, the operation began.
Suction-assisted lipectomy (VASER Liposuction) as Part of Male Breast Reduction Surgery
Suction-assisted lipectomy (VASER Liposuction) has 3 stages
- Injecting wetting solution
- VASER fragments excess fat
- Suction-assisted lipectomy to remove excess fat
Application of Wetting Solution
To make it easier to target fat cells with the VASER, I began this step by applying a wetting solution to the patient’s fatty chest tissue.
Next, I placed a thin cannula (hollow tube) through the skin and into the chest wall.
Vaser Liposuction (Suction-assisted lipectomy)

I use VASER, a handheld wand that melts fat with ultrasonic energy, liquefies solid fat until it becomes a consistency of melted butter. This makes removing the fat much easier, causing less bruising.
VASER gets hot while it goes to work melting away the excess chest fat. To protect the skin from heat damage from the VASER, I place a small plastic port into the skin.

Next, I insert the VASER probe through the skin, moving it back and forth to reach every fat cell.
The VASER probe comes in different sizes. The size chosen is based on how much chest fat needs to be removed. For this patient, I used a five-ring probe at a continuous 80% mode for 12 minutes on each side.
The VASER is efficient for melting fatty tissue on and around the pectoralis major muscles and the lateral sides of the chest. This helped to achieve the squared, masculine look.
Once the fat melting was complete, I checked carefully to make sure everything looked symmetrical. I closely examined the pec muscles to ensure they appear defined and made minor adjustments with the VASER to ensure optimal results.
Though it is important to remove just the right amount of fat — not too much, not too little — my 15+ years of experience have shown that leaving a small padding of fat on the pec muscle results in a more natural, well-defined chest shape.

Breast Gland Removal
Starting with the right breast, the next step was to remove the chest gland. Because each breast has its own breast gland, the process was repeated on the other breast.
Once the gland is removed, it is unlikely to come back, which makes this surgery one of the most effective and successful gynaecomastia treatments. This is a huge relief for men, like this patient, who have struggled with gynaecomastia for years.
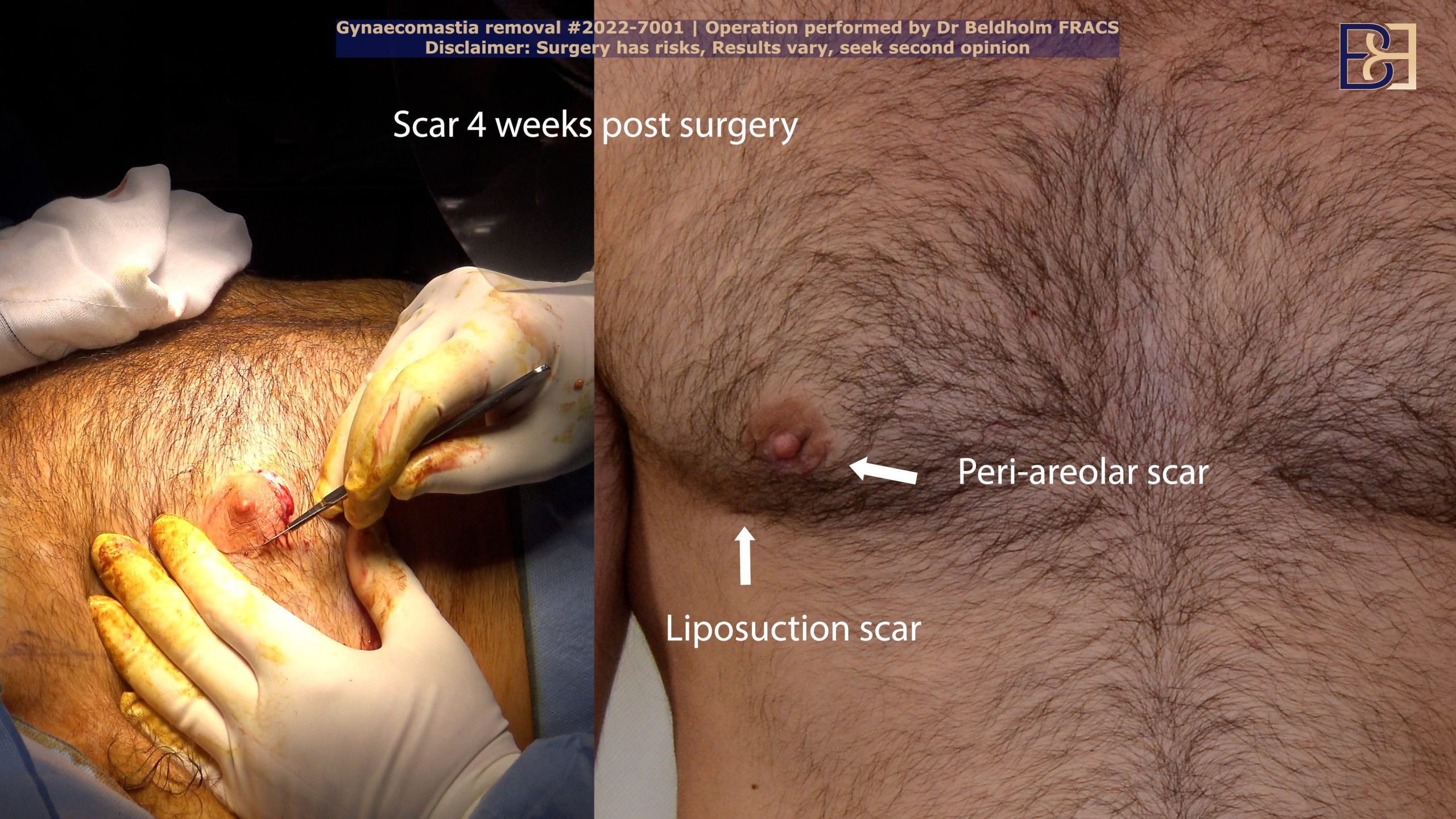
The Incision for Male Breast Reduction Surgery
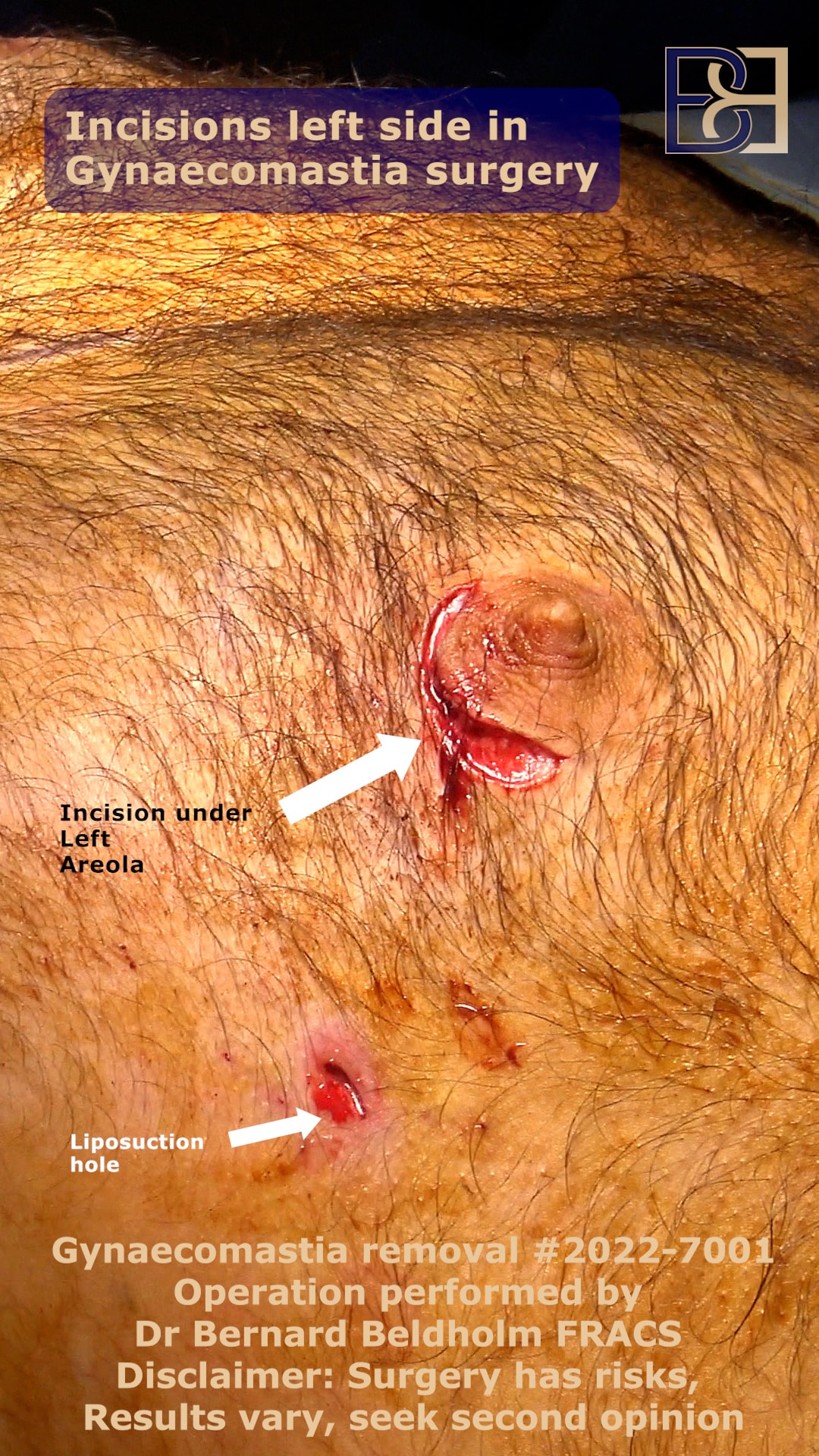
I started by making a small incision on the right breast, following the curve of the areola, just below the nipple. This disguises the scar once it heals. The nipple areola complex was lifted to give me a full view of the gland, located just behind the nipple.
Dissection for Male Breast Reduction Surgery

Next, I made small cuts to dissect the tissue that sits in front of the chest gland. This step, known as dissection, provides access to the gland so it can be removed.
Cutting Out the Gland

The next step of the surgery was removing the chest gland.
The gland, which is commonly hard, rubbery, and white in gynaecomastia patients, is easily detected. To remove the gland, I cut the tissue to separate it from the surrounding tissue.
The end of the gland, which is attached to subcutaneous tissue, is firmly tethered in place, with swollen breast tissue which took quite a bit of effort to remove. I was able to remove the gland only, leaving the tissue intact.
Closing the Incision for Male Breast Reduction Surgery
At this stage, the surgery was almost complete. Once the chest gland was removed, I closed the incision and reattached the nipple areola complex which is the dark skin surrounding the nipple, using a combination of stitches and dissolving sutures to close the wound.
Drain Placement

To prevent fluid buildup, drains are then placed into the chest. The drains, which are hollow tubes that pass through the skin to allow any fluid that collects at the wound site to drain, are removed the following day.
Bandages and Compression Garments Applied
The final step of surgery is bandaging the skin. This keeps the wound clean and free of infection. I also place a compression garment on the chest to provide constant pressure. This garment, which reduces swelling after gynaecomastia surgery, should be worn for several weeks.
Recovery
Once the surgery was complete, the patient woke up in the recovery room at the hospital. Like most men, the patient was able to go home from surgery the same day. I advised the patient that it is normal to feel sleepy for up to 24 hours after general anaesthesia, and I advised him to rest for the first day.
The next day, I met with the patient to remove the drains. I also examined the patient to ensure he was healing well.
Though recovery time varies from patient-to-patient, it normally takes several weeks to fully recover from gynaecomastia surgery. For this reason, the patient was advised to avoid strenuous exercise for up to six weeks.
You should be able to resume most activities within the first 10 days post-surgery, with the exception of heavy lifting and strenuous aerobic exercise.
FAQs Answered by Dr Beldholm
Are there risks related to gynaecomastia surgery?
No surgery is 100% risk-free. Though rare, gynaecomastia surgery carries a 1-3% risk of general complications, with the most common complication being superficial wound infections, occurring in approximately 1.3% of patients.
Some complications can be serious, however, and can even cause death. General complications of any operation include bleeding, blood clot, infection of the surgical site (wound), kidney failure, pulmonary embolus , and an allergic reaction to the materials or medication.
Specific Complications Include:
- Superficial wound complications was the most common complication at 1.3%
- Deep infections 0.2%
- Wound disruption (Dehiscence) 0.3%
- Overall medical complications 0.3%
- Sepsis (blood infection) 0.1%
- Bleeding requiring transfusion 0.1%
During our consultation, I will thoroughly discuss these potential complications.
Understanding the potential complications and how to manage them can help you navigate your surgical journey from preventing infections and managing scars to reducing surgical risks.
For a deeper dive into the potential risks related to this procedure, read my article Navigating Gynaecomastia Surgery Complications: What to Know
Should I get in shape before gynaecomastia surgery?
The answer to this question is “yes.” Incorporating both cardiovascular and strength training exercises can treat fat loss and muscular definition in the chest area. Cardiovascular exercises, such as running or cycling, combined with strength training, can effectively target chest fat and promote overall fitness. This approach helps achieve a more defined chest and overall health. For a more in-depth answer as to why physical fitness matters, how fat affects the surgery, and what you can do to prepare, read my article Should I Get into Shape Before Gynaecomastia Surgery? – A Comprehensive Guide.
What is the average cost of gynaecomastia surgery in Australia?
The average cost for gynaecomastia surgery in Australia ranges from $5,000 to $10,000, varying based on factors like surgery complexity & private insurance.
In 2022-23, private patients averaged around $3,700 in out-of-pocket costs after insurance contributions, though this can fluctuate based on individual insurance policies and procedure specifics.
What does Dr. Beldholm’s surgeon fee include?
When having surgery, there are usually several fees that need to be taken into account. Once you have seen Dr. Beldholm in the rooms, our patient coordinator will help you finalise these costs and guide you as needed.
Costs for subcutaneous mastectomy include:
- Surgical fee
- Hospital fee
- Anaesthetist fee
- Assistant fee
Dr Beldholm’s surgical fee covers the surgical operation, one compression garment, post-op appointments for 12 months, and LED light treatments.
Does Medicare cover gynaecomastia surgery?
Gynaecomastia is an abnormal increase in breast tissue in men, resulting in enlarged male breasts. Because surgery for male breast reduction surgery to reduce this excess breast tissue and glandular breast tissue can provide relief.
It is important to note that Medicare Australia will only cover gynaecomastia surgery if it is deemed medically necessary and classified as reconstructive plastic surgery. This includes cases with significant physical discomfort, psychological distress, or conditions like male breast cancer.
Medicare does not cover the hospital fee at private hospitals, so you will need to handle that cost yourself. If you have private health coverage, it should cover the hospital cost if you are on the correct plan.
Eligibility for Medicare rebates varies based on individual circumstances, often causing confusion regarding coverage. Clarifying these nuances is important for those considering the surgery, affecting both financial and medical planning. To help clear up some of the confusion surrounding this topic, I have created a comprehensive guide: Medicare Australia: Does It Cover Gynaecomastia Surgery?
What is the MBS item number for gynaecomastia surgery?
The MBS item number for gynecomastia surgery is 31525 and 31526.
What criteria must be met to qualify for MBS Item 31525 for gynaecomastia?
You need to show that the surgery is medically necessary or reconstructive, have chronic pain or significant breast size, and have dealt with gynaecomastia for over a year.
What scarring will result from gynaecomastia surgery?
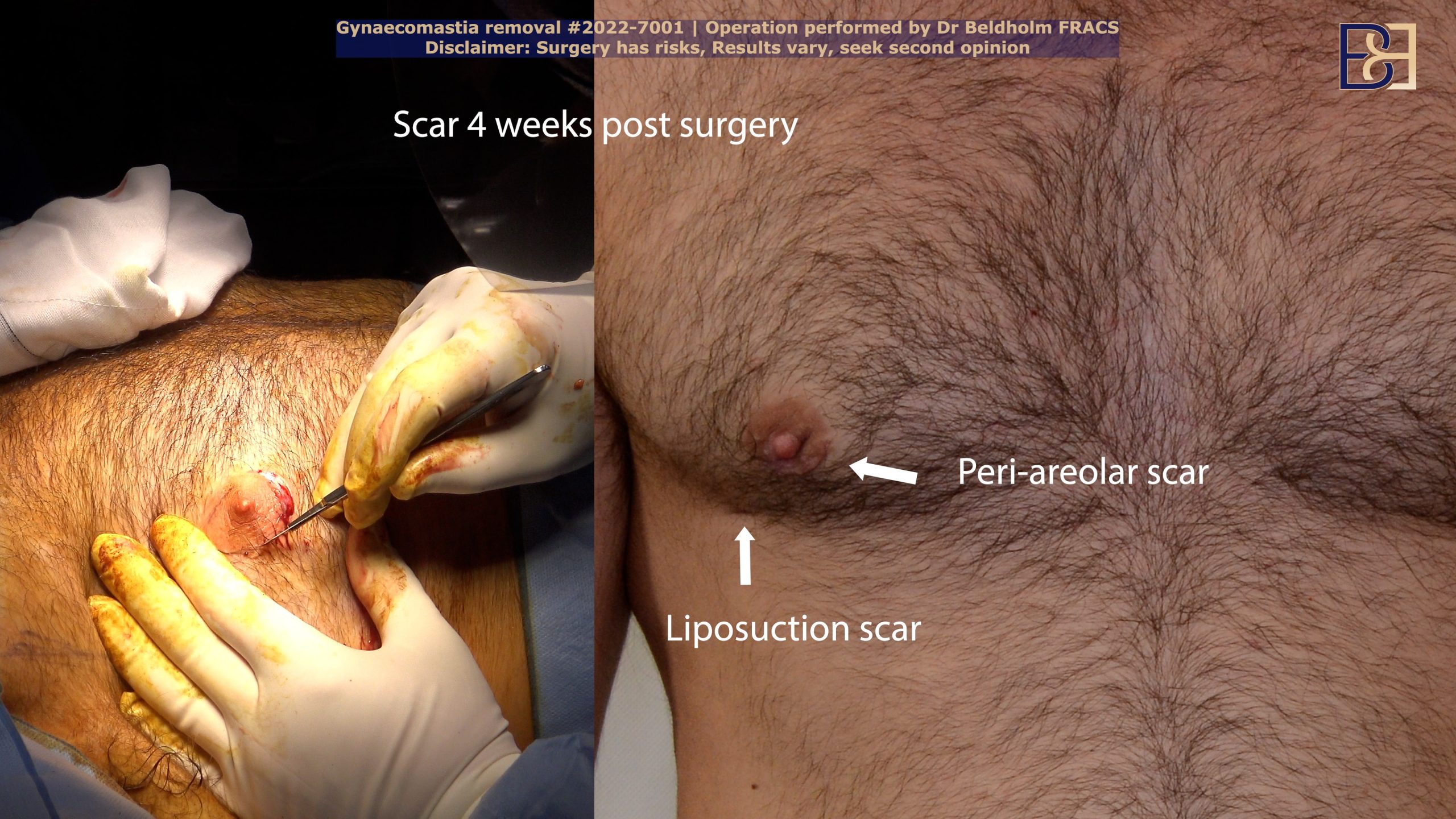
Scarring from this procedure is generally minimal, as the incisions are small and strategically placed to minimize visibility. The dark skin surrounding the areola may be reduced during the procedure.
How Long Do Male Breast Reduction Results Last?
While excess skin, tissue and/or fat are permanently removed during male breast reduction surgery, certain post-surgical lifestyle habits such as maintaining optimal general health can be employed to help reap the full benefits.
Book your appointment online now
Final Thoughts by Dr Bernard Beldholm, Specialist Surgeon who performs Gynaecomastia Surgery
The journey to a flatter chest is a marathon, not a sprint. So, if you are considering undergoing this procedure, it’s important to take it one step at a time and consult with your specialist surgeon whenever needed. Patients are advised to carefully consider the options and have realistic expectations about the results when deciding whether to undergo this procedure.
Vaser liposuction (Suction-assisted lipectomy) assisted gynaecomastia surgery is a minimally invasive procedure that can help.
Though the procedure can help, it may not completely eliminate or remove excess breast tissue or fat. The results may vary depending on the severity of the condition, individual contour irregularities, and the patient’s overall health.
It’s essential to consult with a specialist surgeon FRACS to discuss your options and determine if you’re a good candidate for the procedure. I have been a specialist surgeon performing treatment options such as gynaecomastia surgery in Lorn, New South Wales for over 15 years.
References
- https://www.google.com/url?q=https://www.medicalnewstoday.com/articles/83044&sa=D&source=docs&ust=1725634483711488&usg=AOvVaw3XU309bQcyvnAhhKAGhG-x
- Zavlin D, et al. “Complications and Outcomes After Gynecomastia Surgery: Analysis of 204 Pediatric and 1583 Adult Cases from a National Multi-center Database.” Aesthetic Plastic Surgery. 41(4):761-767, 2017 Aug.
- Nuzzi LC et al. “Psychosocial impact of adolescent gynecomastia: a prospective case-control study.”, Plastic & Reconstructive Surgery. 131(4):890-896, 2013 Apr.