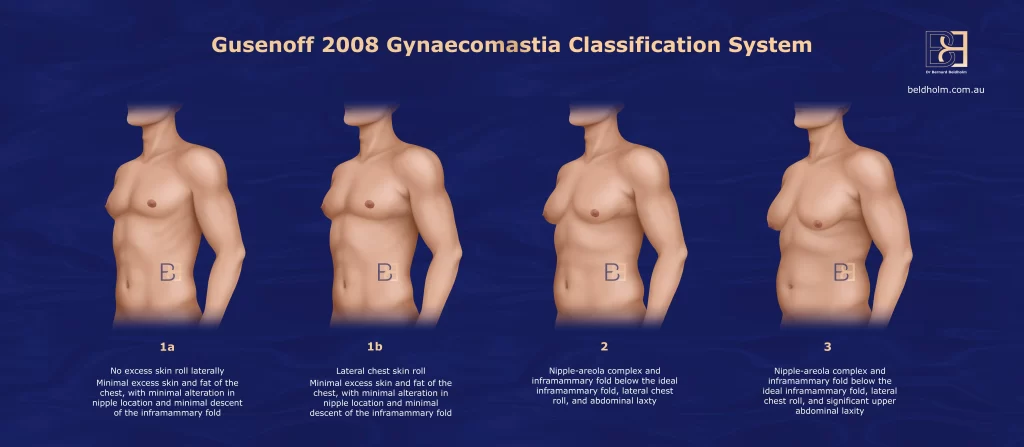
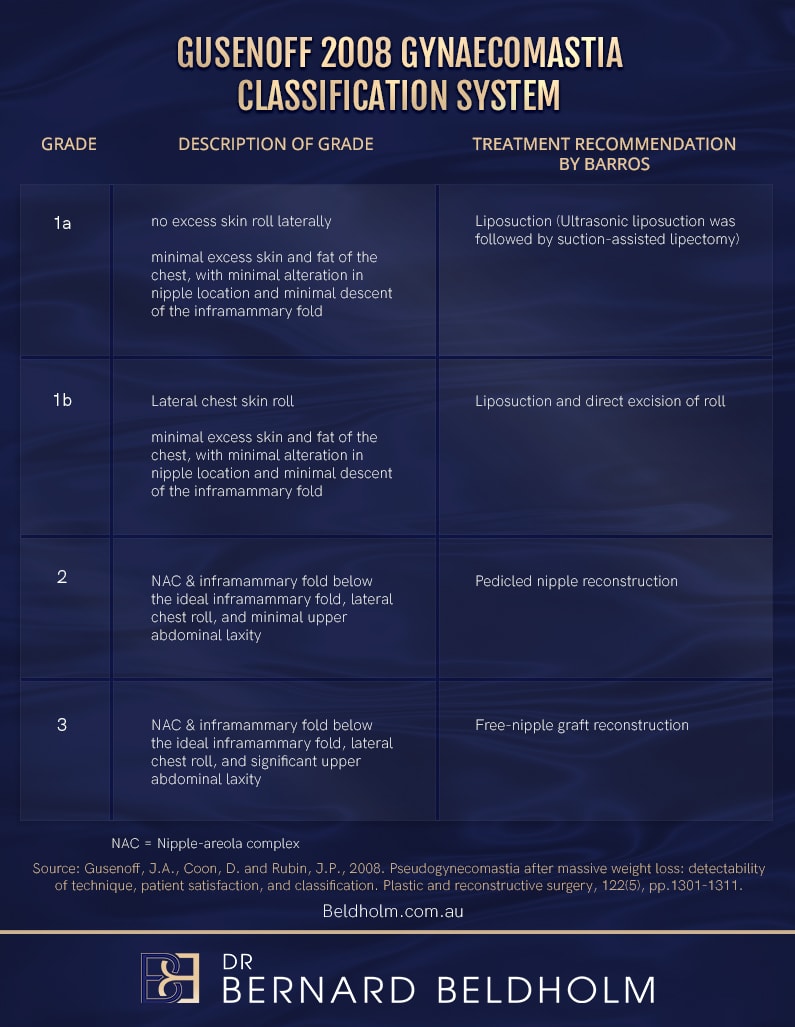
Developed by Jeffrey A. Gusenoff to classify gynecomastia based on the severity of breast tissue enlargement, skin excess, and the degree of ptosis, the Gusenoff Gynaecomastia Classification System is particularly focused on guiding surgical treatment for patients, providing a clear framework for surgeons to choose the appropriate technique based on the severity of the condition.
This section covers one of the numerous classification systems for gynaecomastia, originally developed by Gusenoff to give a precise understanding of this grading approach. However, Dr. Beldholm uses a unique grading system in his practice, which he believes provides assessment and treatment recommendations. For a full overview of available gynaecomastia grading systems, refer to Dr. Bernard Beldholm’s article: Dr. Bernard Beldholm’s Comprehensive Summary of Gynaecomastia Surgery Grading Systems.
Key Elements of the Gusenoff Gynaecomastia Classification System
- Breast Volume: Enlarged breast tissue (glandular or fatty)
- Skin Excess: Degree of redundant skin
- Ptosis (Nipple Position): Degree of ptosis based on the nipple’s position relative to the IMF (inframammary fold).
Book your appointment online now
Gusenoff Gynaecomastia Classification System
The Gusenoff Gynaecomastia Classification Grading System is divided into four grades, which consider both the glandular tissue hypertrophy and the degree of skin laxity (ptosis) associated with gynecomastia, allowing for better matching of surgical techniques to the patient presentation.
Grade 1a of the Gusenoff Gynaecomastia Classification System
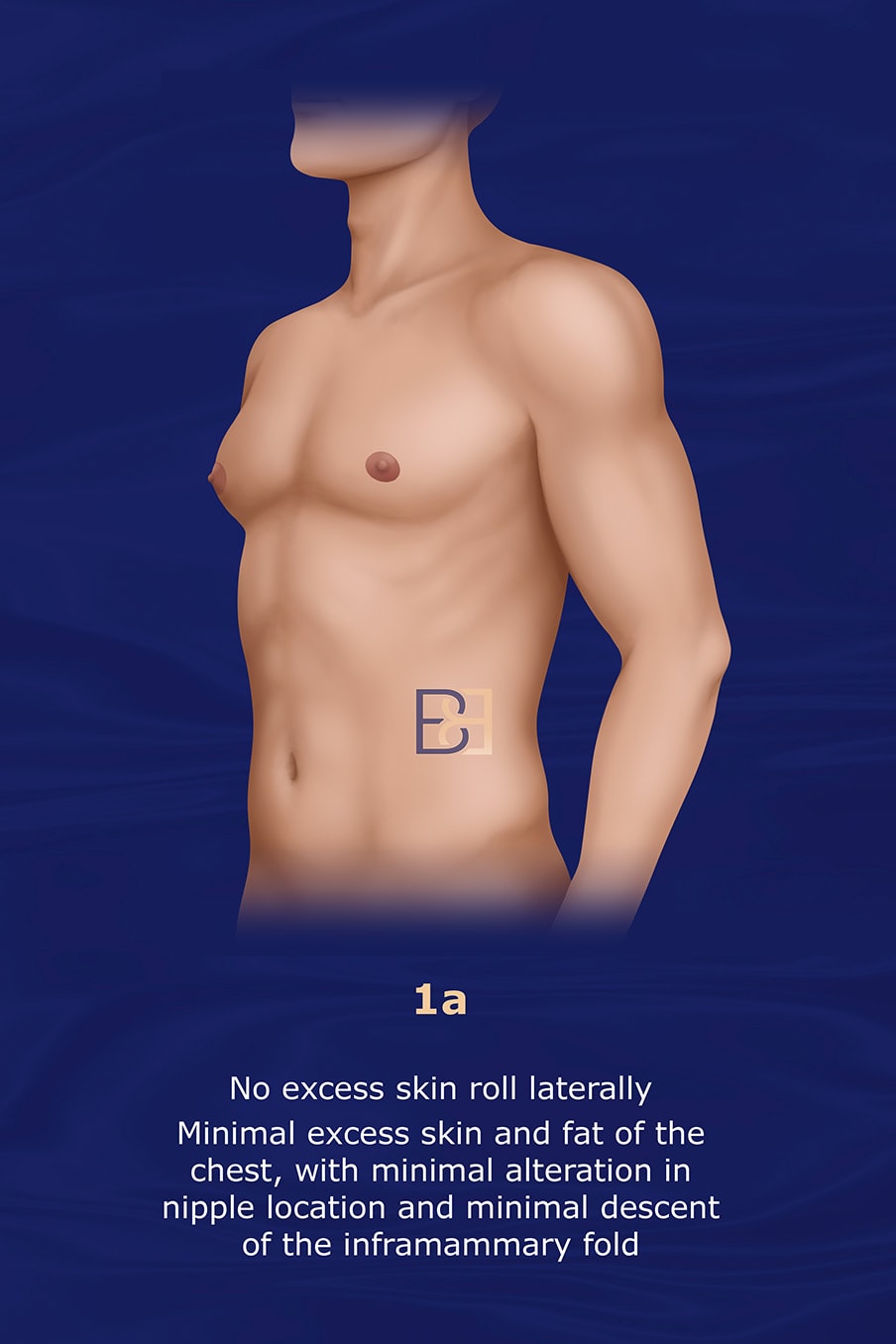
- No excess skin roll laterally
- Minimal excess skin and fat on the chest
- Minimal alteration in nipple location in one or both breasts
- Minimal descent of the inframammary fold
Grade 1b Gusenoff Gynaecomastia Classification System
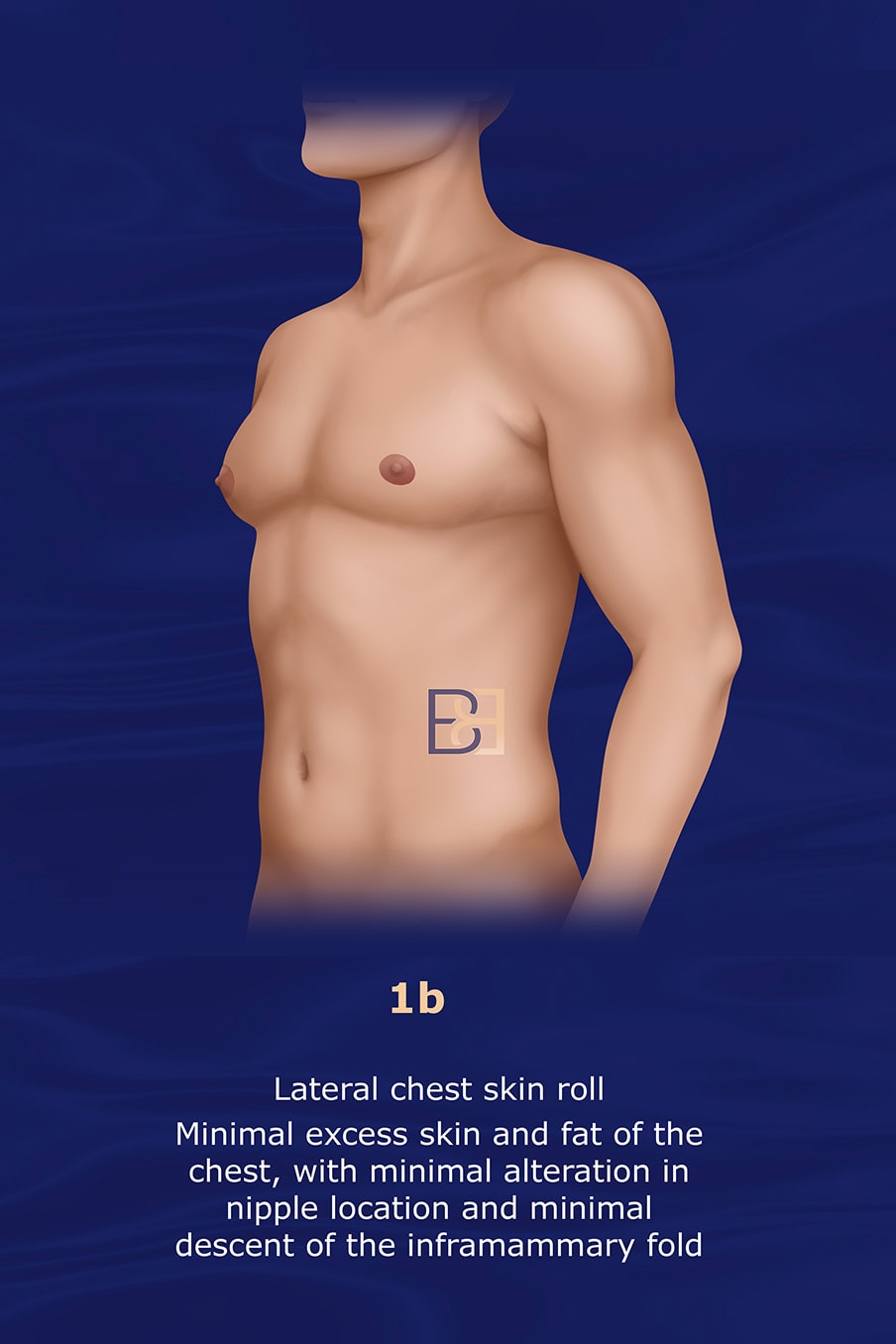
- Lateral chest skin roll on one or both breasts
- Minimal excess skin and fat on the chest
- Minimal alteration in nipple location
- Minimal descent of the inframammary fold
Grade 2 Gusenoff Gynaecomastia Classification System
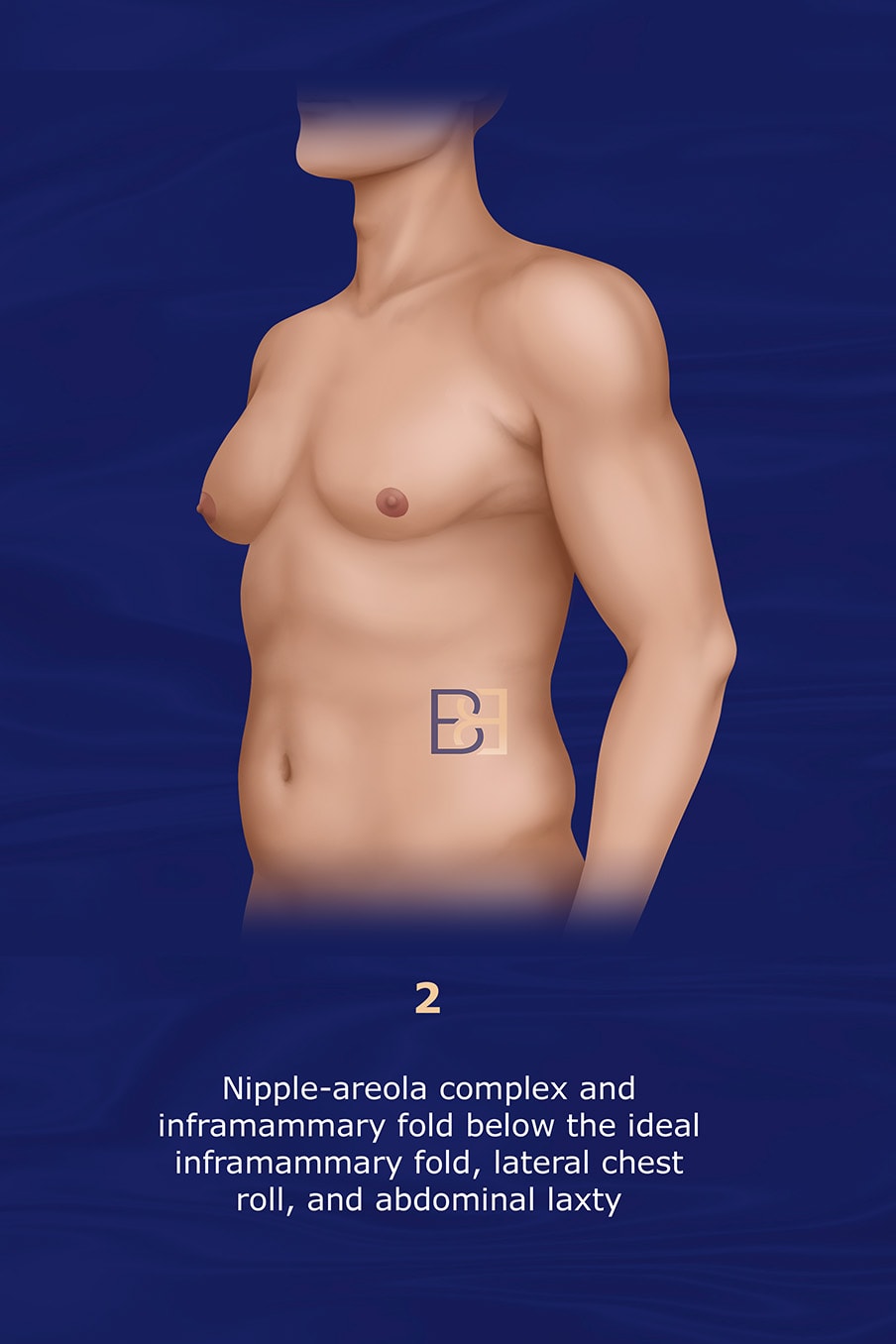
- Nipple-areola complex (NAC) and inframammary fold below the ideal inframammary fold
- Lateral chest roll on one or both breasts
- Abdominal laxity
Grade 3 Gusenoff Gynaecomastia Classification System
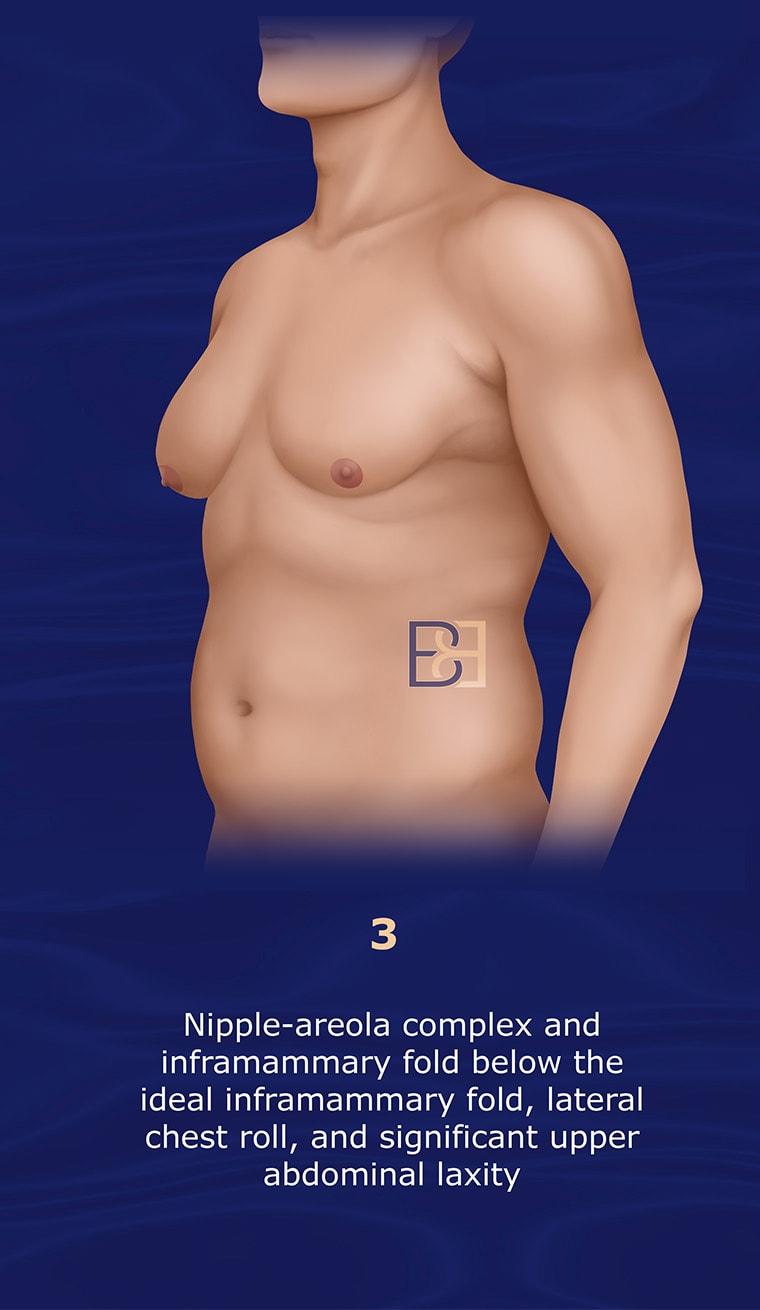
- Nipple-areola complex (NAC) and inframammary fold below the ideal inframammary fold
- Lateral chest roll
- Significant abdominal laxity
Gusenoff Treatment Considerations
Treatment for gynaecomastia varies depending on the grade according to the Gusenoff 2008 Gynaecomastia Classification System. Here’s a breakdown of potential treatments for each grade:
Gusenoff Treatment Considerations Grade 1A
Involving only minor breast enlargement without excess skin, Grade IA is often treated with suction-assisted lipectomy (liposuction) alone to remove excess fatty tissue or glandular excision if glandular tissue is present. Treatment includes ultrasonic and suction-assisted lipectomy followed by secondary excisional techniques.
Gusenoff Treatment Considerations Grade 1B

Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Treatment for this grade, which includes moderate enlargement with skin excess, is suction-assisted lipectomy (liposuction) or glandular excision combined with skin tightening procedures. Minor skin excision techniques (such as periareolar incisions) may be used to avoid extensive scarring. Treatment includes ultrasonic and suction-assisted lipectomy along with direct excision of the lateral chest roll as well as secondary excisional techniques for residual deformity.
Gusenoff Treatment Considerations Grade 2
Grade 2 pseudogynecomastia was treated with a dermoglandular pedicled reconstruction. The authors advocated an elliptical excision of chest skin with the preservation of the nipple on a thinned, broadbased dermal pedicle.
Gusenoff Treatment Considerations Grade 3
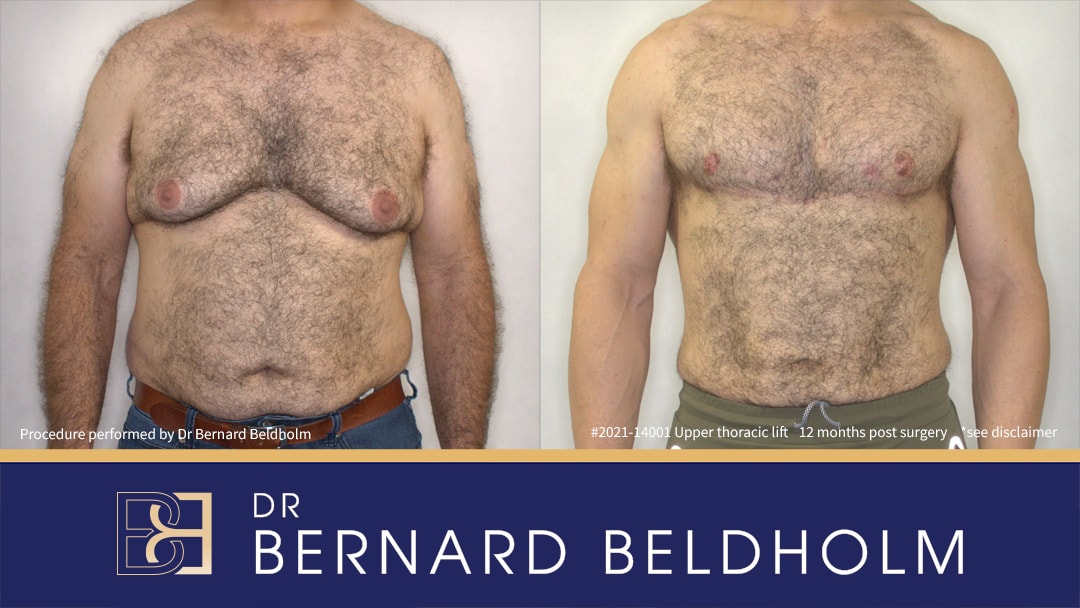
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Due to the extent of resection, grade 3 pseudogynecomastia is treated with free-nipple grafting. The superior incision line is determined by downward retraction of the chest tissues to the desired location of the final scar. The inferior margin of resection is estimated by a pinch test conducted when the patient is standing preoperatively. The entire region is resected, including the chest deformity, lateral chest roll, and upper abdominal excess.
Advantages of the Gusenoff Classification System

Surgical Focus
The classification is particularly helpful for surgeons in deciding the appropriate surgical technique based on the extent of gynaecomastia and skin laxity.
Emphasis on Ptosis
One of the key features of this system is its emphasis on ptosis, which is critical in guiding the extent of skin excision and nipple repositioning.
Surgical Outcomes
By categorizing patients into distinct grades, the system ensures more tailored surgical planning, reducing the risk of over- or under-treatment.
Disadvantages of the Gusenoff Classification System
Focused on Severe Cases
The system is primarily surgical in nature and may not be as useful for non-surgical management of early-stage gynaecomastia or patients seeking less invasive options.
Complex Procedures for Higher Grades
For patients with Grade III or IV gynecomastia, the surgical procedures can be complex and may require advanced techniques for optimal outcomes.
Limited Differentiation
The Gusenoff system may lack granularity for differentiating between various tissue compositions (fat versus glandular tissue). Gynaecomastia cases often present unique tissue distributions, which can affect treatment approaches. The system’s focus primarily on skin excess and ptosis may overlook other anatomical nuances, limiting its precision in guiding surgical planning.
Subjectivity in Classification
Like many grading systems, the Gusenoff system can introduce subjective interpretation among surgeons. Variations in individual assessment of tissue laxity and skin quality can lead to inconsistent classifications across practitioners, potentially impacting treatment consistency and outcomes.
Focus on Severe Cases
The Gusenoff system is more useful in cases with significant ptosis or skin redundancy but may offer limited guidance for mild gynecomastia. As the system is primarily surgical in nature, it is not useful for non-surgical management of early-stage gynaecomastia or patients seeking less invasive options.
Limited Guidance for Post-Weight Loss Patients
The classification was developed to treat traditional gynaecomastia and may not adequately account for the complex presentation of gynaecomastia in massive weight-loss patients. These patients often have unique challenges with extensive skin laxity and variable tissue composition, which the Gusenoff system does not fully treat.
Dr Beldholm’s Opinion of Gusenoff Grading System

- Though varying from patient-to-patient, most post-weight loss patients have limited benefit from non-invasive treatments such as suction-assisted lipectomy (liposuction) as their skin is generally inelastic and will not pull back to the new shape.
- The pedicle technique leaves too much excess tissue and has a tendency to leave the male chest with a round, less-than-masculine appearance.
- The study was not large enough to reach many new conclusions.
Final Thoughts
The Gusenoff 2008 Gynecomastia Classification System is a practical and surgeon-oriented grading tool, particularly useful in evaluating and planning surgical treatments for patients with moderate to severe gynaecomastia. Its emphasis on both breast volume and ptosis allows for a more personalised approach to treatment, ensuring that the surgical intervention matches the severity of the condition. However, its utility is more limited in non-surgical management or milder cases of gynaecomastia.
An increasing number of male patients are presenting for treatment of male chest deformity after massive weight loss. The authors prefer to preserve the nipple-areola complex on a dermoglandular pedicle. They sought to identify detectability of technique, assess patient progress, and outline a treatment algorithm for this population.
Resources
- Pories, W. J., Swanson, M. S., MacDonald, K. G., et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann. Surg. 222: 339, 1995.
- Santry, H. P., Gillen, D. L., and Lauderdale, D. S. Trends in bariatric surgical procedures. J.A.M.A. 294: 1909, 2005.
- Samuel, I., Mason, E. E., Renquist, K. E., Huang, Y. H., Zimmerman, M. B., and Jamal, M. Bariatric surgery trends: An 18-year report from the international bariatric surgery registry. Am. J. Surg. 192: 657, 2006.
- American Society of Plastic Surgeons. 2006 Cosmetic Surgery GenderDistribution:Male: http://www.plasticsurgery.org/media/statistics/loader.cfm?url/commonspot/security/getfile.cfm&PageID23768. Accessed December 3, 2007. Braunstein, G. D. Gynecomastia. N. Engl. J. Med. 357: 1229,2007.
- Simon, B. E., Hoffman, S., and Kahn, S. Classification of gynecomastia. Plast. Reconstr. Surg. 51: 48, 1973.
- Rohrich, R., Ha, R., Kenkel, J., and Adams, W. P., Jr. Classifications and management of gynecomastia: Defining the role of ultrasound-assisted liposuction. Plast. Reconstr. Surg. 111: 909, 2003.
- Beckenstein, M. S., Windle, B. H., and Stroup, R. T., Jr. Anatomical parameters for nipple position and areolar diameter in males. Ann. Plast. Surg. 36: 33, 1996.
- Beer, G. M., Budi, S., Seifert, B., Morgenthaler, W., Infanger,M., and Meyer, V. E. Configuration and localization of the nipple-areola complex in men. Plast. Reconstr. Surg. 108: 1947,2001.
- Shulman, O., Badani, E., Wolf, Y., and Hauben, D. J. Appropriate location of the nipple-areola complex in males. Plast. Reconstr. Surg. 108: 348, 2001.
- Gusenoff, J. A., Messing, S., O’Malley, W, et al. Patterns of plastic surgical use after gastric bypass: Who can afford it and who will return for more. Plast. Reconstr. Surg. 122: 951, 2008.
- Hodgson, E. L., Fruhstorfer, B. H., and Malata, C. M. Ultrasonic liposuction in the treatment of gynecomastia. Plast.Reconstr. Surg. 116: 646, 2005.
- Tashkandi, M., Al-Qattan, M. M., Hassanain, J. M., Hawary,M. B., and Sultan, M. The surgical management of high-grade gynecomastia. Ann. Plast. Surg. 53: 17, 2004.
- Kornstein, A. N., and Cinelli, P. B. Inferior pedicle reduction technique for larger forms of gynecomastia. Aesthetic Plast.Surg. 16: 331, 1992.
- Persichetti, P., Berloco, M., Casadei, R. M., Marangi, G. F., Di Lella, F., and Nobili, A. M. Gynecomastia and the complete circumareolar approach in the surgical management of skin redundancy. Plast. Reconstr. Surg. 107: 948, 2001.
- Song, A. Y., Jean, R. D., Hurwitz, D. J., Fernstrom, M. H., Scott, J. A., and Rubin, J. P. A classification of contour deformities after bariatric weight loss: The Pittsburgh rating scale. Plast. Reconstr. Surg. 116: 1535, 2005.
- Hurwitz, D. J. Single-staged total body lift after massive weight loss. Ann. Plast. Surg. 52: 435, 2004.
- Mladick, R. A., Hunstad, J. P., Pitman, G. H., et al. Practice forum: Male body contouring. Aesthetic Surg. J. 26: 307, 2006.
- Gusenoff, J. A., Messing, S., O’Malley, W., et al. Temporal and demographic factors influencing the desire for plastic surgery after gastric bypass surgery. Plast. Reconstr. Surg. 121: 2120, 2008.
- Gorney, M. Cosmetic surgery in males. Plast. Reconstr. Surg. 110: 719, 2002.
- Pertschuk, M. J., Sarwer, D. B., Wadden, T. A., and Whitaker, L. A. Body image dissatisfaction in male cosmetic surgery patients. Aesthetic Plast. Surg. 22: 20, 1998.
- Song, A. Y., Rubin, J. P., Thomas, V., Dudas, J. R., Marra, K. G., and Fernstrom, M. H. Body image and quality of life in post massive weight loss body contouring patients. Obesity 14: 1626, 2006.
- Gusenoff, J.A., Coon, D. and Rubin, J.P., 2008. Pseudogynecomastia after massive weight loss: detectability of technique, patient satisfaction, and classification. Plastic and reconstructive surgery, 122(5), pp.1301-1311.