Combining subcutaneous mastectomy with suction-assisted lipectomy (liposuction) to treat gynaecomastia is a proven method, targeting both firm glandular and excess fatty breast tissue. This article explains how this combination works, its benefits, and what to expect during treatment and recovery.
Book your appointment online now
Key Takeaways
- Gynaecomastia, characterized by the benign enlargement of male breast tissue, often requires medical intervention if persistent, with emotional and psychological implications considered in treatment decisions.
- The combination of subcutaneous mastectomy and suction-assisted lipectomy (VASER liposuction) surgical outcomes for gynaecomastia.
- Effective postoperative recovery and maintenance of results hinge on adopting a healthy lifestyle and regular monitoring of hormone levels, ensuring sustained and surgical outcomes.
Understanding Gynaecomastia
Gynaecomastia is primarily caused by an imbalance in the oestrogen and androgen ratio in males, often triggered by factors such as:
- hormonal imbalances
- weight gain
- anabolic steroid use
- certain medications
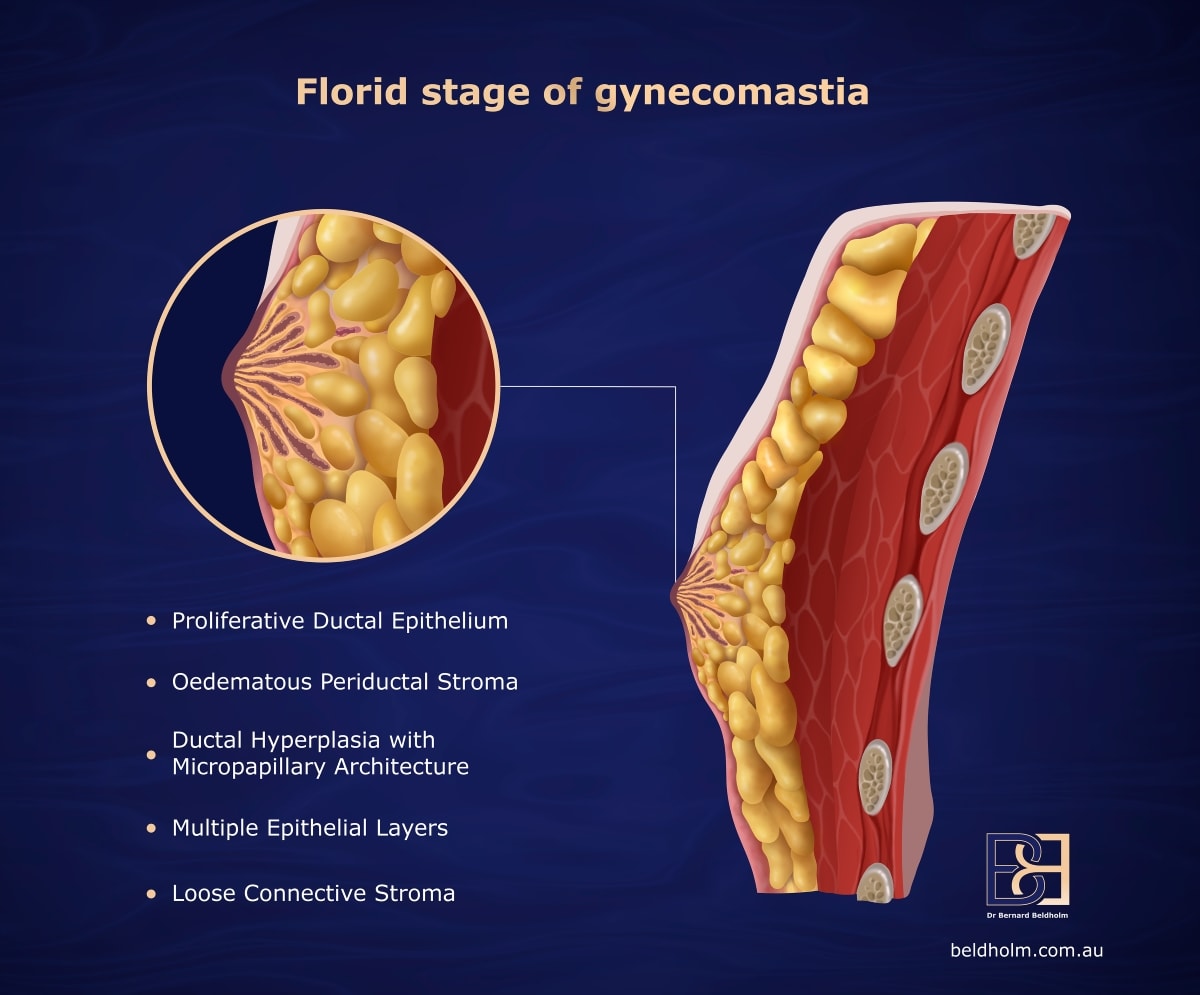
This condition leads to the benign enlargement of male breast tissue, marked by an increase in glandular breast tissue rather than fat. These hormonal shifts are especially common during adolescence and aging, making gynaecomastia a widespread concern among men of various age groups.
Common symptoms of gynaecomastia include lumps in the breasts, excess fat, and a palpable, tender, firm, mobile, disc-like mound of tissue under the nipple. Beyond physical discomfort, gynaecomastia often leads to significant emotional distress, embarrassment, and social anxiety. For many, the condition can affect daily interactions, making effective treatment essential. Studies have shown a marked decrease in embarrassment and social anxiety following successful treatment.
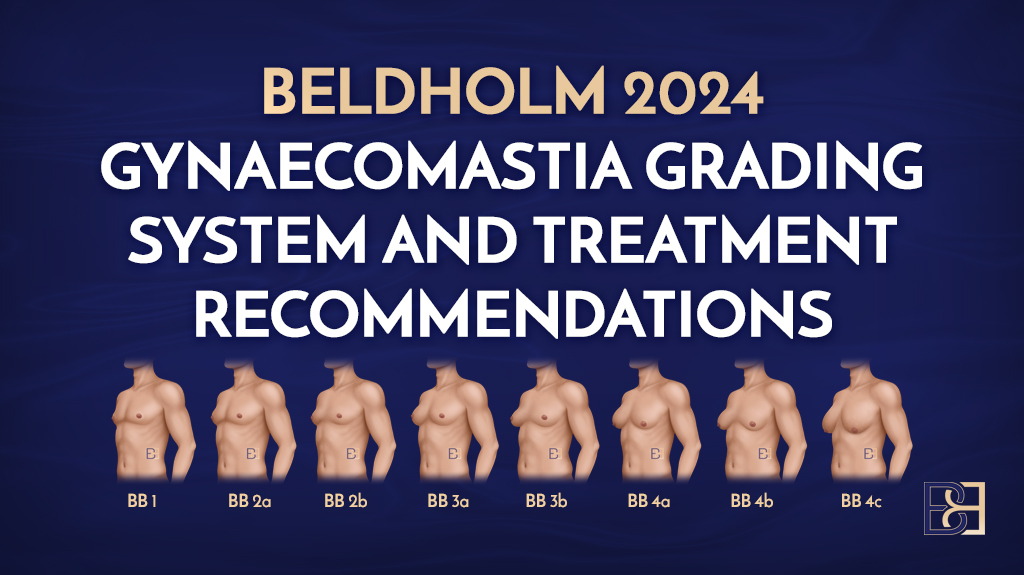
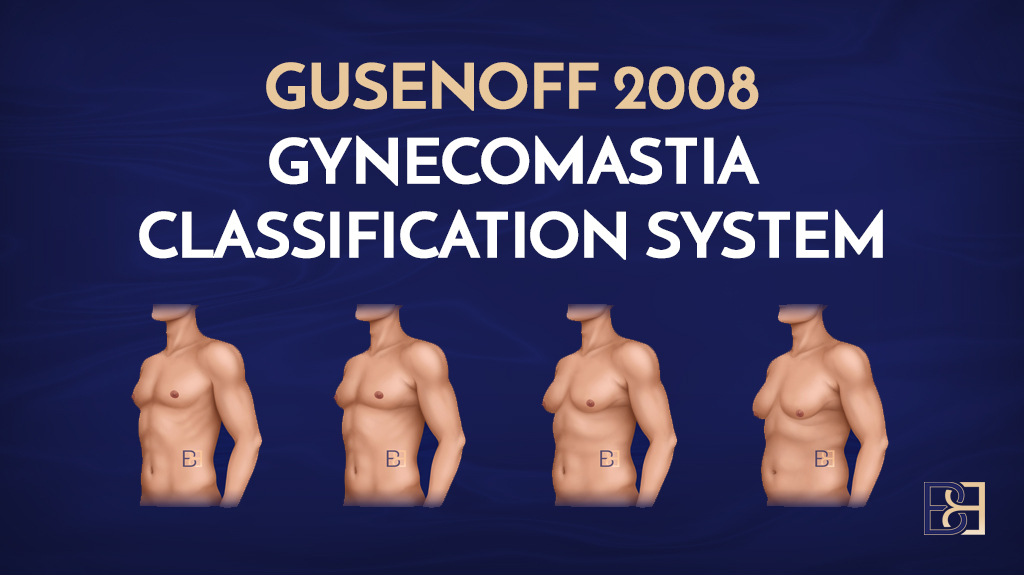
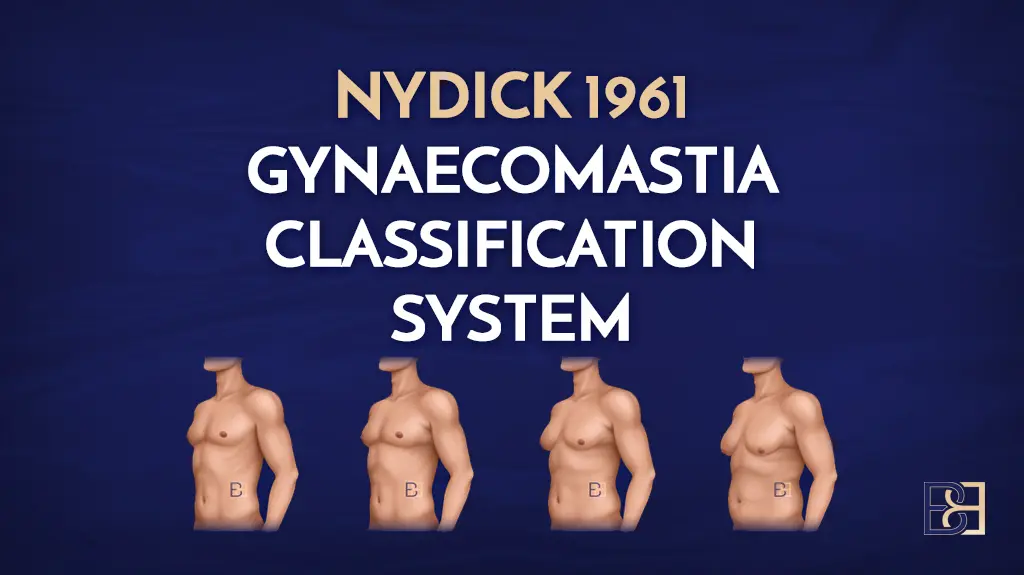
While some cases of gynaecomastia resolve on their own, particularly in adolescents, persistent cases may require medical intervention. Treatment is typically pursued when the condition is severe, persistent, or causes significant emotional or psychological issues. Understanding the different grades of gynaecomastia, from mild (BB Grade 1) to severe (BB Grade 4), helps in determining the appropriate treatment approach, whether it be surgical or non-surgical.
Subcutaneous Mastectomy: A Surgical Approach
Subcutaneous mastectomy is a surgical approach that involves removing a significant portion of breast tissue while preserving the nipple-areolar complex. Various techniques, including semicircular and transareolar methods, are employed in subcutaneous mastectomy, each presenting unique advantages and challenges. Complications can include haematomas, nipple necrosis, and aesthetic dissatisfaction, sometimes necessitating further corrective procedures. Despite these potential issues, the integration of suction-assisted lipectomy (VASER liposuction) with subcutaneous mastectomy has shown surgical outcomes to be successful. The combination of subcutaneous mastectomy and suction-assisted lipectomy (VASER liposuction) treatment results for gynaecomastia, offer efficacy.
Suction-assisted lipectomy (VASER liposuction) in Gynaecomastia Treatment
Suction-assisted lipectomy (VASER liposuction) plays a crucial role in the treatment of gynaecomastia. This technique utilises ultrasound technology to break down fat cells, making them easier to remove. Suction-assisted lipectomy (VASER liposuction) is more targeted compared to traditional methods, efficiently breaking down fat while minimising complications such as irregularities and unevenness. Patients also benefit from reduced bruising and shorter recovery times.

Typically performed under general anesthesia, suction-assisted lipectomy (VASER liposuction) reduces both surgery and recovery durations. This method is particularly beneficial for patients with excess fat tissue in the chest, aiding in achieving a more contoured and aesthetically pleasing result.
Combining suction-assisted lipectomy (VASER liposuction) with glandular tissue removal offers comprehensive solutions tailored to individual patient needs.
Combining Subcutaneous Mastectomy with Suction-assisted Lipectomy (VASER liposuction)
Integrating subcutaneous mastectomy with suction-assisted lipectomy (VASER liposuction) provides significant benefits for patients suffering from gynaecomastia. This combination is especially beneficial for those with excess fat tissue, as it allows for precise contouring of the chest area, leading to better treatment outcomes.
The dual procedure effectively targets both glandular and adipose tissue, offering a tailored solution that meets individual patient needs.
For a detailed step-by-step guide on this procedure, please refer to my blog article “Surgical Treatment: Bilateral Suction-assisted Lipectomy (VASER Liposuction) Gynaecomastia Surgery for Grade BB 2a Gynaecomastia.”
Efficacy and Cosmetic Effect
Combining subcutaneous mastectomy with suction-assisted lipectomy provides a synergistic effect that significantly boosts the overall efficacy of gynaecomastia treatment. The dual approach allows for complete removal of glandular tissue along with excess fat, leading to a more definitive treatment outcome.
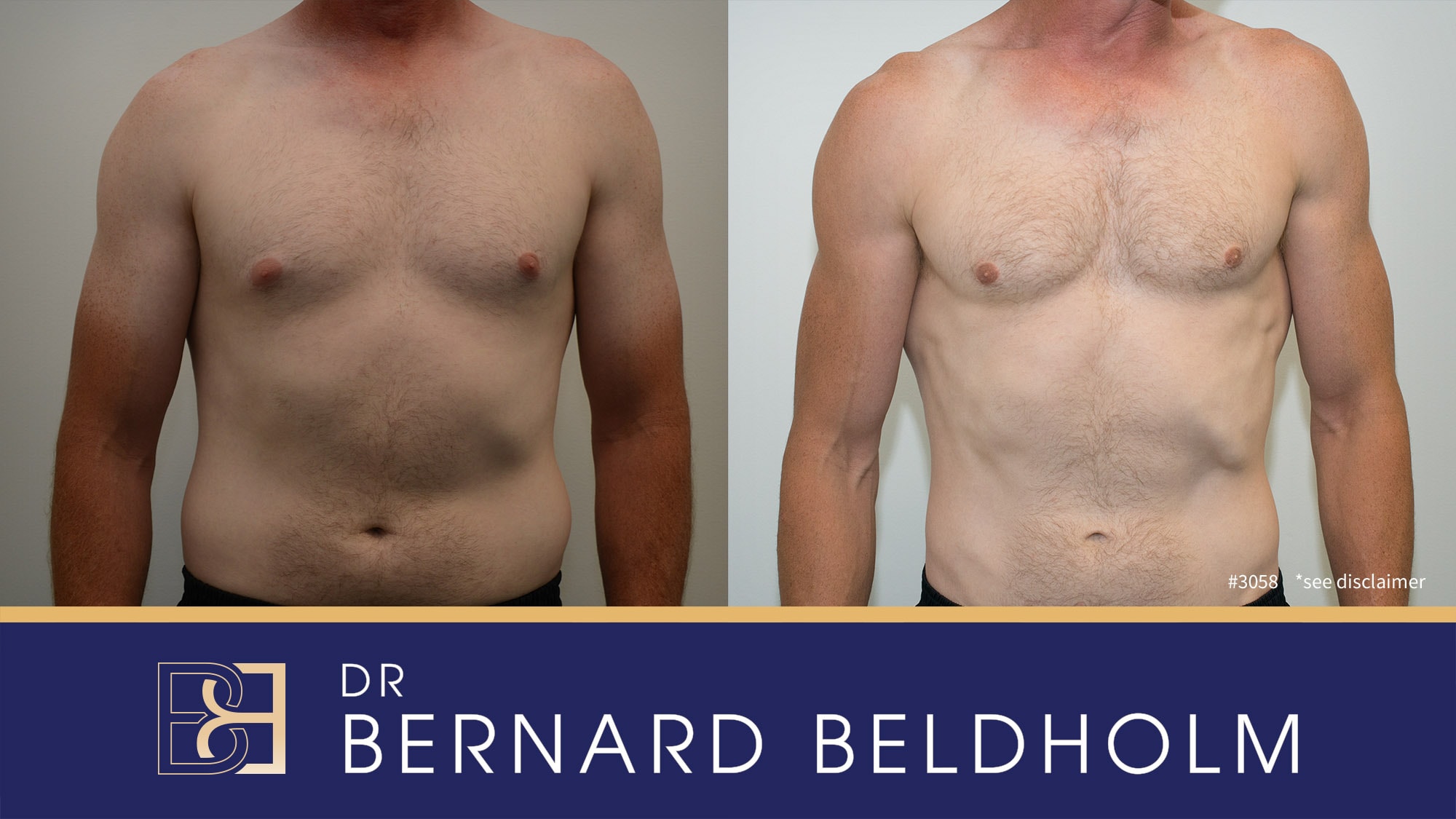
Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Suitable Candidates for surgical treatment of gynaecomastia
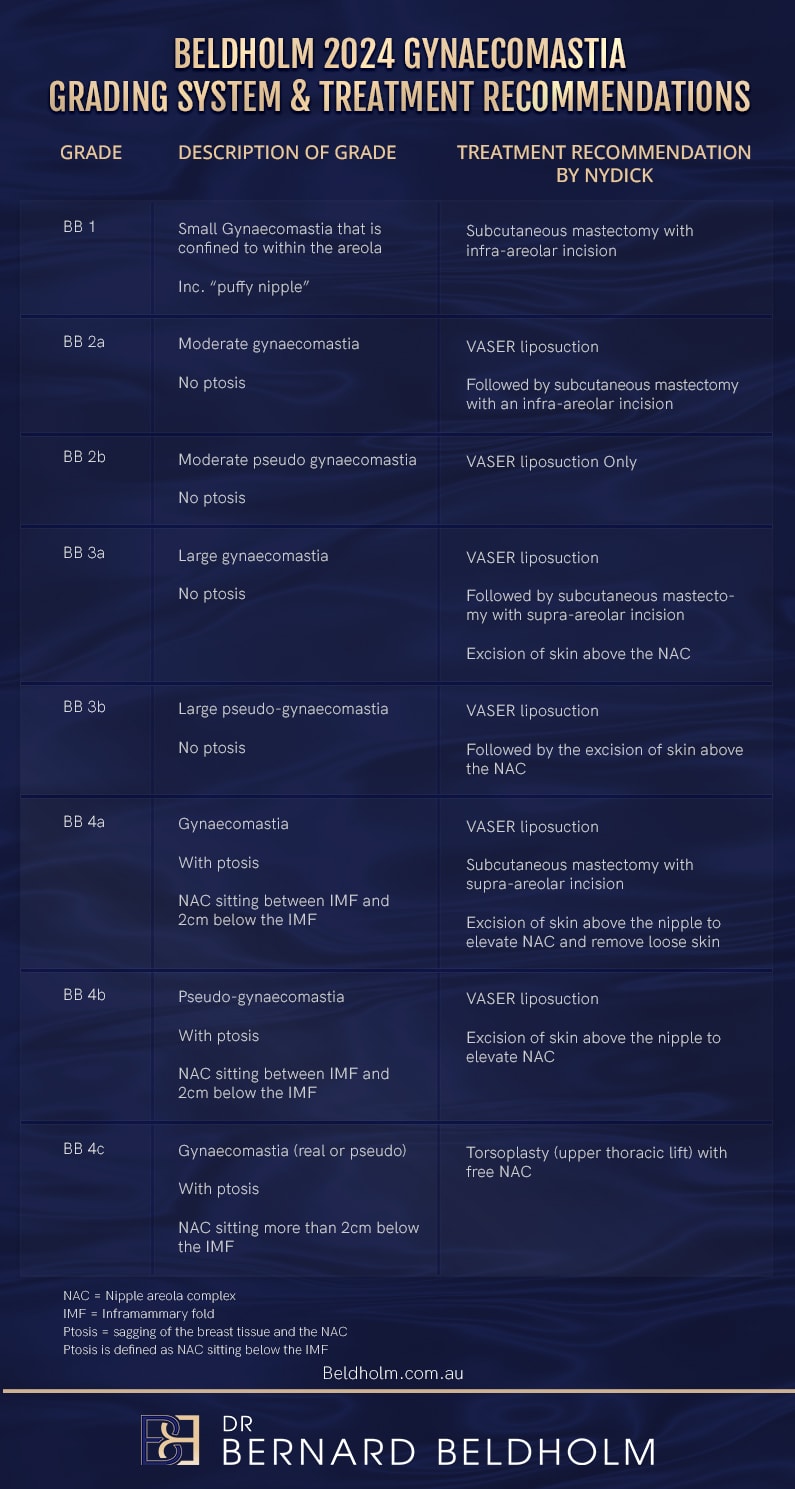
Candidates for the combined technique are typically those with significant breast enlargement and associated psychosocial distress, especially individuals who have not responded to non-surgical management. Ideal candidates are those with BB grade 2a, 3a and 4a gynaecomastia seeking a surgical correction. These patients often have good skin elasticity, which is important for achieving optimal results.
BB Grade 2a is defined as:
- Moderate gynaecomastia
- No ptosis
- Dr Beldholm recommends Suction-assisted Lipectomy (VASER Liposuction), followed by subcutaneous mastectomy with an infra-areolar incision for this grade
BB Grade 3a is defined as:
- Large gynaecomastia
- No ptosis
- Dr Beldholm recommends Suction-assisted Lipectomy (VASER Liposuction), followed by subcutaneous mastectomy with supra-areolar incision. The skin above the areola is then removed in a semicircle to tighten the skin and lift the NAC
BB Grade 4a is defined as:
- Gynaecomastia with ptosis
- The nipple sits between the lower breastfold and 2cm below
- Dr Beldholm recommends Suction-assisted Lipectomy (VASER Liposuction), followed by subcutaneous mastectomy with supra-areolar incision. Excision of skin above the nipple to elevate NAC (Nipple areolar complex) and remove loose skin.
In my experience with performing these operations, the benefit of Suction-assisted Lipectomy (VASER Liposuction) is twofold: it removes fat and shapes the chest wall, lowering the chance of saucer deformity.
Health and realistic expectations are key criteria for candidates. Those considering this combined approach should maintain stable body weight and manage any underlying medical treatment conditions to ensure the best outcomes from the surgery.
Selecting suitable candidates ensures the combined procedure offers effective and satisfying results for those with gynaecomastia.
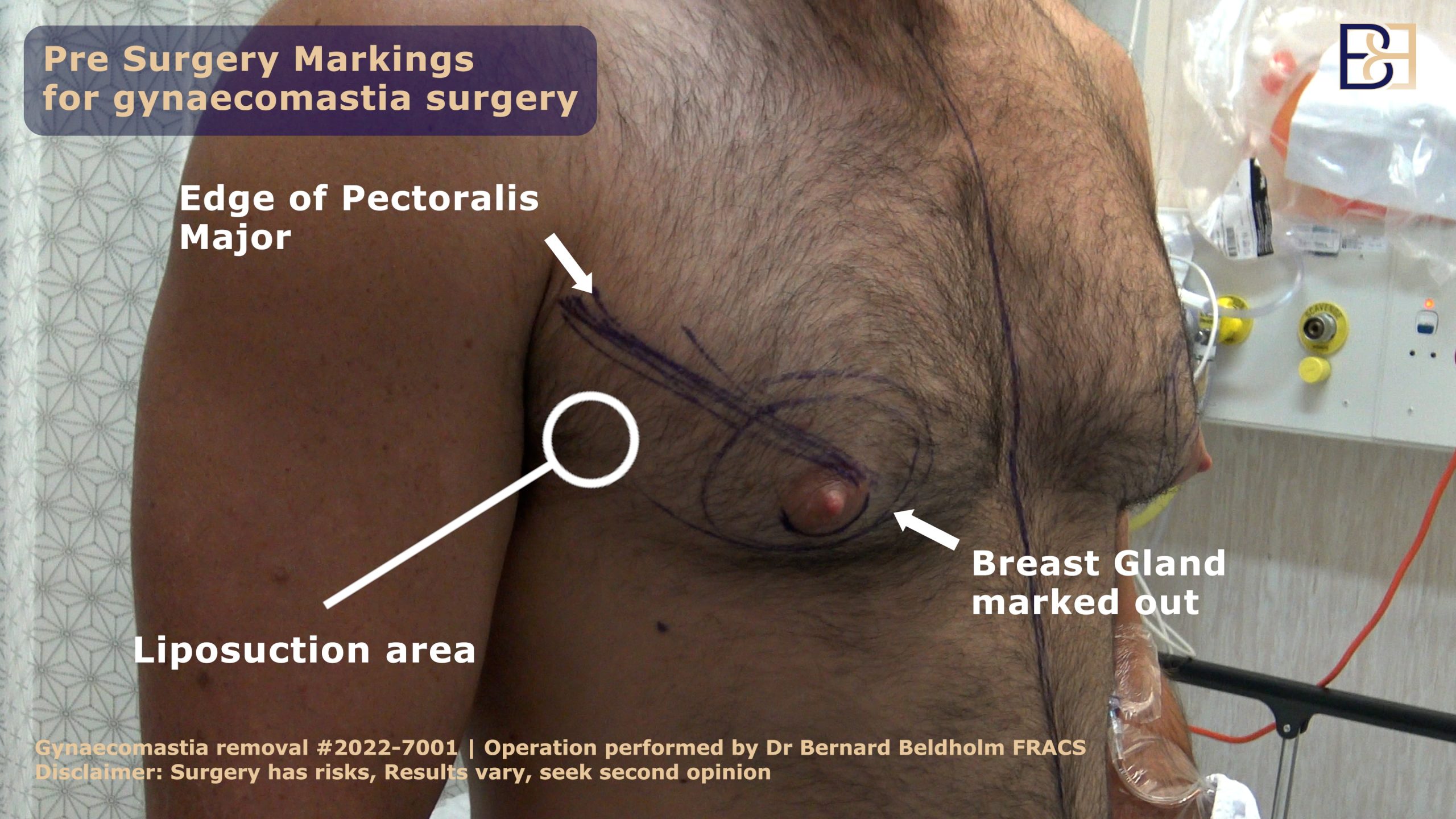
Preoperative Examination and Planning
Identifying true gynaecomastia involves a physical examination that can differentiate between glandular and fatty tissue. Ultrasound examinations are often used to confirm the presence of glandular tissue in suspected cases of gynaecomastia. A thorough medical history, including medication use, is crucial for understanding the potential causes of gynaecomastia and planning the appropriate treatment approach.
Standard laboratory tests, including hormone levels like testosterone, oestradiol, and luteinizing hormone, are necessary to assess any hormonal imbalances that may be contributing to the condition. Effective preoperative planning lowers complication rates, ensuring a smoother surgical and recovery process for patients.
The Surgical Procedure

The average duration of surgery is around 1.5 hours. This surgical technique involves a series of steps, including anesthesia, lipolysis solution injection, Suction-assisted Lipectomy (VASER Liposuction), and subcutaneous mastectomy.
The procedure begins with the administration of general anesthesia to ensure patient comfort.
Suction-assisted Lipectomy (VASER Liposuction) involves three main steps:
- Injection of a wetting solution containing local anesthetic and adrenaline
- VASER treatment
- Suction lipectomy
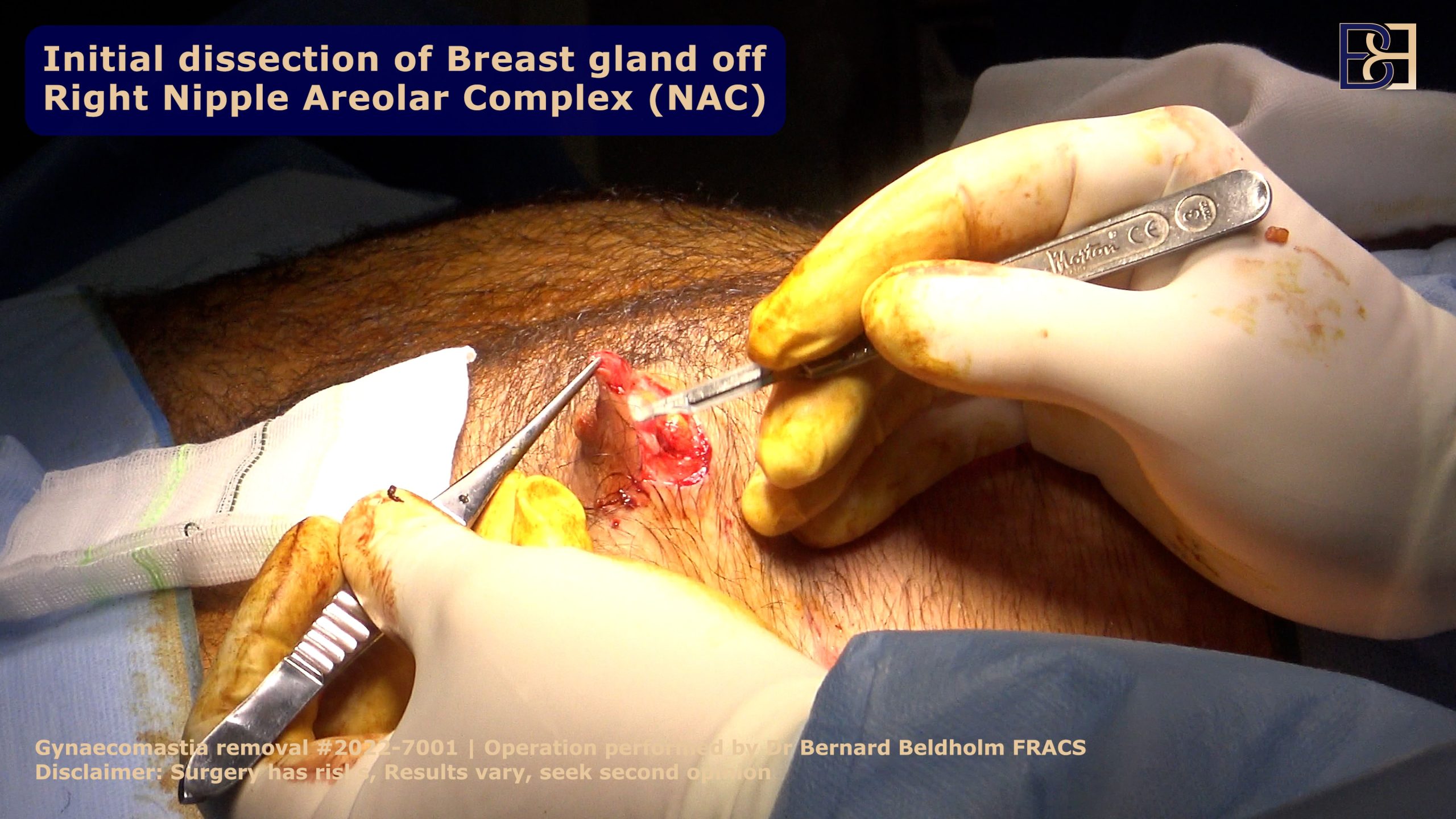
After Suction-assisted Lipectomy (VASER Liposuction) is completed, the breast gland is usually well defined. Depending on the need to remove skin, the incision is made either under the areola or above it. For more severe cases of gynaecomastia that may involve loose skin, the incision is made above the areola and a small amount of skin is removed to lift and tighten the areola and skin.
The sub-cutanous mastectomy is then performed by removing the breast glandular tissue though the areolar incision.
Drains are generally used for this operation.
Postoperative Care and Recovery
The typical recovery after gynaecomastia surgery is between 10 days to 2 weeks, with most patients able to return to work and resume light activities by the end of the first week. Initially, patients are advised to avoid strenuous movements to ensure proper healing. After two weeks, many men can start to resume normal daily activities, although vigorous exercise should still be postponed.
Most patients are cleared for normal exercise by the 3-4 week mark, with most swelling and bruising resolved by this time. Pain and tightness are common for the first 2-3 days post-surgery, but these can be effectively managed with pain medication. Compression garments are recommended to minimise swelling and aid in the healing process.
Potential risks include bruising, bleeding, fluid collections, visible scarring, infections, deep vein thrombosis, and contour irregularities.
See our article on “Effective Gynaecomastia Surgery Recovery Time: Tips & Timeline” for more information on recovering from gynaecomastia surgery.
Long-term Results and Maintenance
Maintaining the long-term results of gynaecomastia surgery requires a commitment to healthy lifestyle choices. A diet high in fruits and vegetables, along with proper hydration, supports overall health and helps in preventing hormonal fluctuations. To achieve sustained benefits, individuals need to keep their weight stable while adopting a nutritious diet.
Engaging in regular physical exercise is essential for maintaining the results of gynaecomastia surgery. Incorporating regular physical activity into daily routines not only helps maintain the effects of the treatment but also promotes overall well-being.
Monitoring hormone levels and making healthy lifestyle choices can help sustain long-term results and ensure continued success with the surgical outcomes.
Dr Beldholm’s Final Words
Combining subcutaneous mastectomy with Suction-assisted Lipectomy (VASER Liposuction) offers a comprehensive and effective treatment for gynaecomastia. This approach not only focuses on the physical aspects of the condition but also significantly elevates cosmetic outcomes, leading to higher patient success. By understanding the procedures, benefits, and necessary postoperative care, individuals can make informed decisions about their treatment. Ultimately, this combined technique provides a promising solution for those seeking to alleviate the physical and emotional burdens of gynaecomastia.
Frequently Asked Questions
What is the purpose of gynaecomastia surgery?
The purpose of gynaecomastia surgery is to remove excess breast tissue in men resulting from hormonal imbalances, thereby resulting in a flatter and more male chest appearance.
What conditions can lead to gynaecomastia?
Gynaecomastia can arise from hormonal imbalances, weight gain, the use of anabolic steroids, and specific medications. It is crucial to be aware of these factors to manage this condition effectively.
What is the recovery timeline after gynaecomastia surgery?
The recovery timeline after gynaecomastia surgery typically spans 10 days to 2 weeks. Most patients can return to work and engage in light activities within a week.
What are the potential risks of gynaecomastia surgery?
Gynaecomastia surgery carries risks such as bruising, bleeding, fluid collections, visible scarring, infections, deep vein thrombosis, and contour irregularities. It is essential to weigh these potential complications before proceeding with the procedure.
What lifestyle changes can help maintain long-term results after gynaecomastia surgery?
Maintaining long-term results after gynaecomastia surgery is essential to maintain a stable weight, adopt healthy lifestyle choices, and regularly monitor hormone levels. These practices will support your recovery and help preserve the surgical outcome.