Need details on the post pregnancy abdominoplasty MBS item number? As of July 2022, MBS Item 30175 covers this surgery for muscle separation after pregnancy. Learn more about eligibility, documentation, and benefits here.
Key Takeaways
- MBS Item 30175, introduced for post-pregnancy abdominoplasty, helps mothers with muscle separation (diastasis recti) affecting their health.
- Eligibility requires medical necessity, documented muscle separation, and failed conservative treatments; a GP referral and imaging are crucial.
- Abdominoplasty can alleviate symptoms like back pain and urinary incontinence, with Medicare offering a $828.90 (2024) rebate for qualifying surgeries.
Introduction to the MBS Item for Post Pregnancy Abdominoplasty

Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Book your appointment online now
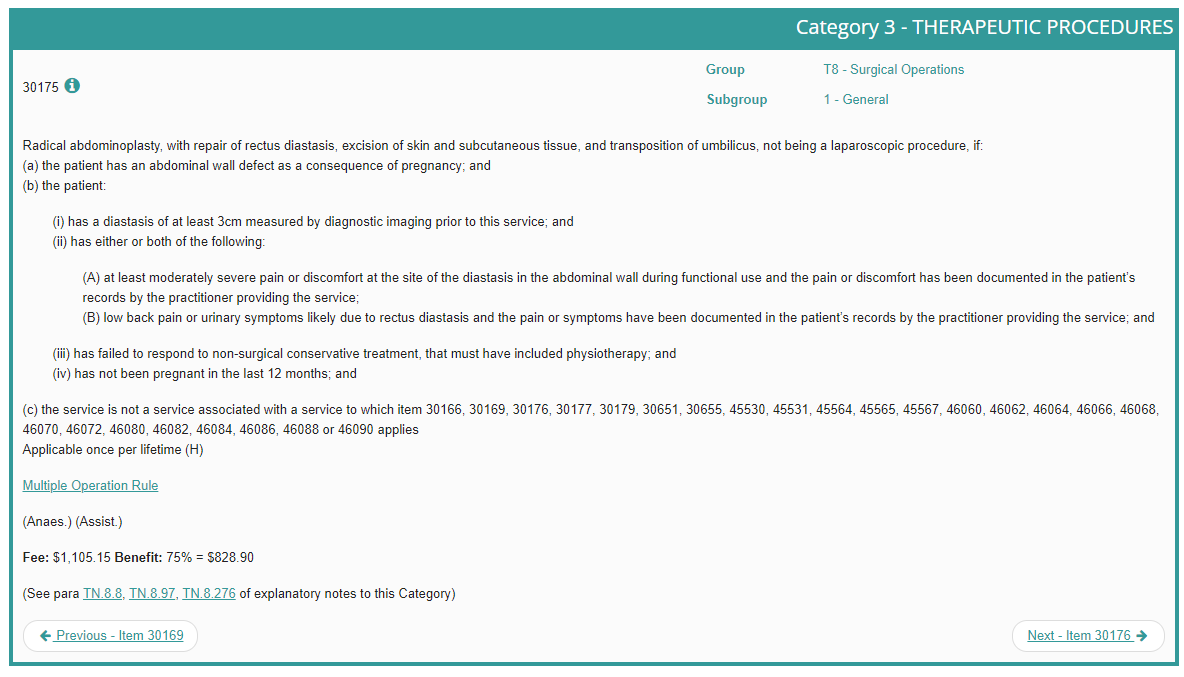
The Medicare Benefits Schedule (MBS) is a comprehensive list of medical services covered by the Australian government, each with an associated item number to qualify for rebates. As of 1 July 2022, a new item number, MBS Item 30175, has been introduced specifically for post-pregnancy abdominoplasty. This new item focuses on the muscle separation that many women experience after pregnancy, known as diastasis recti.
With over $6 million in funding allocated to support eligible mothers, this initiative aims to help those struggling with significant muscle separation and its related symptoms. Introducing this new item number marks a significant step towards acknowledging and focusing on the physical challenges postpartum women face.
The MBS Item 30175 is not just another number; it’s a lifeline for many mothers who have been battling the aftermath of pregnancy. Understanding this new item and how it works can make a world of difference in your post-pregnancy recovery journey.
Eligibility Criteria for MBS Item 30175
Medicare coverage under the new MBS item number requires the abdominoplasty to be medically necessary and not solely for cosmetic purposes. This item specifically targets women with muscle separation due to pregnancy.
Patients must meet specific eligibility criteria: a documented case of diastasis recti with at least a 3 cm separation confirmed by diagnostic imaging, at least 12 months post-pregnancy, and unsuccessful conventional treatments.
A GP referral, detailing the patient’s symptoms and requesting an ultrasound of the rectus wall is crucial. This documentation establishes the necessity of the procedure and ensures all medical criteria are met.
Eligibility Criteria
The MBS Item Number 30175 descriptor states the patient must:
- Have diastasis recti as a result of pregnancy
- Wait at least 12 months after pregnancy to have the procedure
- Have at least a 3 cm separation of the rectus abdominis muscle
- Have failed to respond to conventional, non-surgical treatments for diastasis recti
- Have documentation of moderate-to-severe pain/discomfort and/or lower back pain or urinary incontinence as a result of their muscle separation
What kind of documented proof do I need?
- Diagnostic imaging may be needed to confirm a 3 cm or more separation between the abdominal muscles.
- A doctor should note whether the patient has physical discomfort or symptoms from the condition.
- The physician should also specify whether the muscle separation and related symptoms have not responded to conservative treatments such as:
- Medications
- Physiotherapy
- Lifestyle changes
- A lower back brace
Who decides if I am eligible?
Typically, a specialist surgeon makes the final call. The patient would receive a referral to a specialist surgeon from their GP. It is wise to keep records of any services provided by a physiotherapist, exercise physiologist or radiologist.
Symptoms Addressed by Post-Pregnancy Abdominoplasty
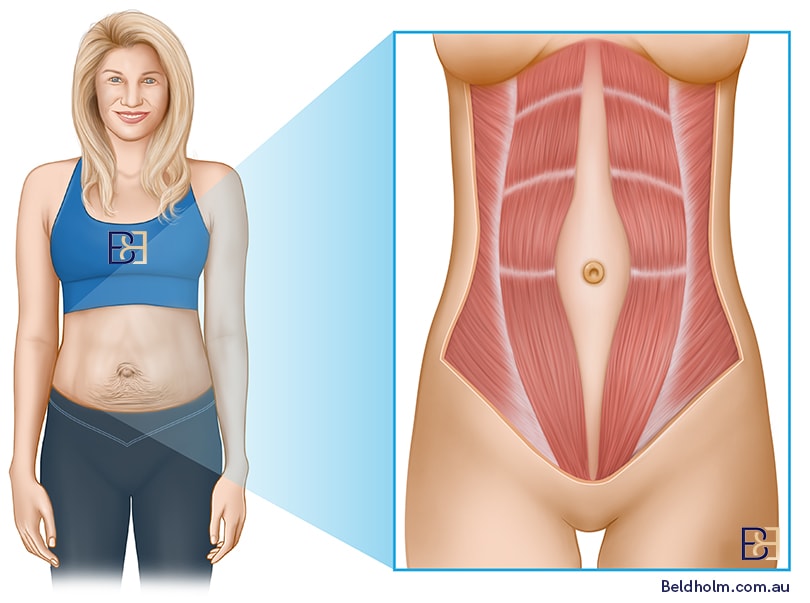
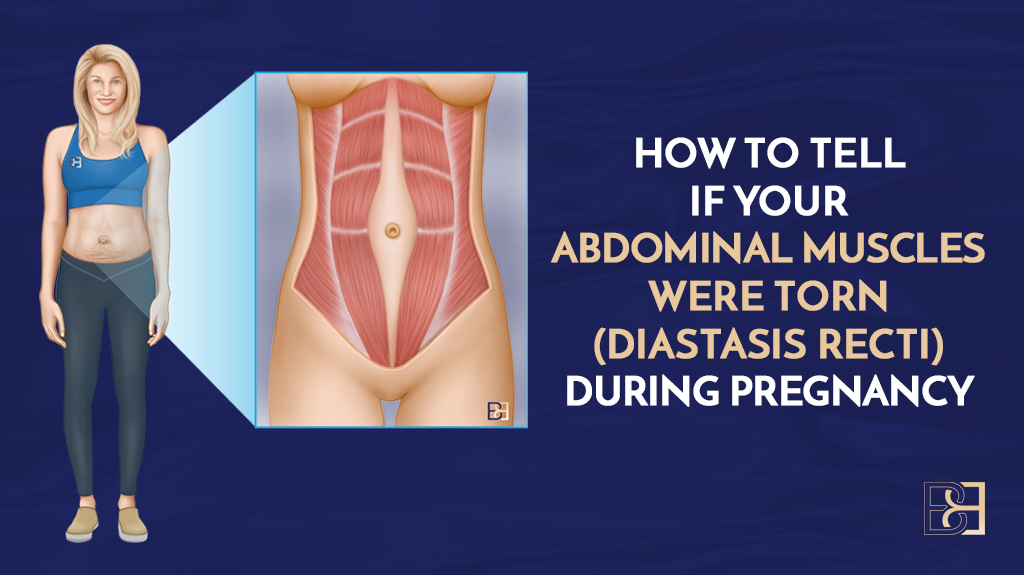
Diastasis recti, a condition affecting up to two-thirds of postpartum women, refers to the widening between the rectus abdominis muscles.
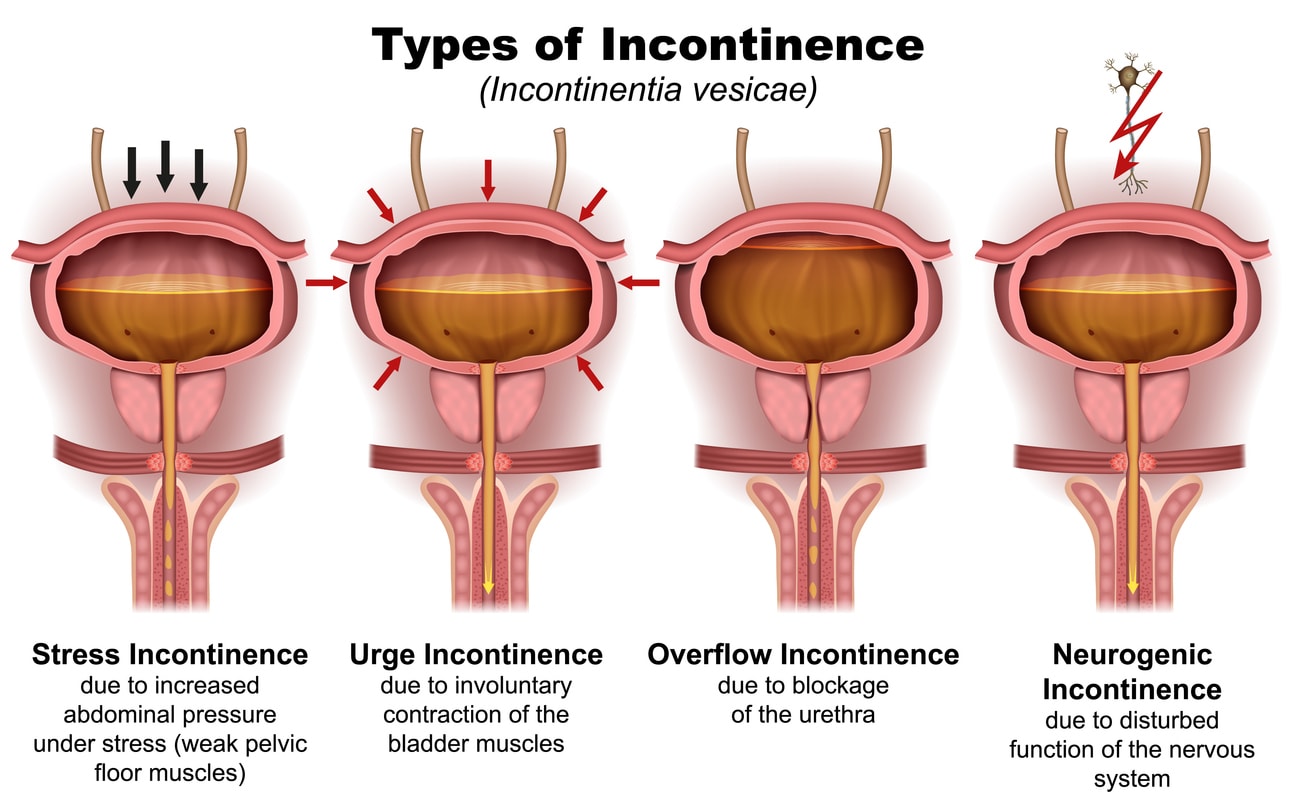
This condition can lead to various symptoms, including:
- hernia
- pelvic pain or urinary symptoms
- constipation
- poor posture
- low back pain
- feeling bloated
- urinary incontinence
- a lower tummy pooch
- reduced trunk stability
- a visible gap between the abdominal muscles and urinary symptoms.
Abdominoplasty can effectively alleviate these symptoms. Studies have shown that women who undergo this procedure experience significant relief from lower back pain and urinary incontinence. For instance, around 51% of women reported moderate to severe back pain before surgery, which decreased to only 9% six months post-operation. Similarly, urinary incontinence, which affected 42.5% of women pre-surgery, dropped to less than 2% after six months.
Consulting a specialist surgeon offers further insights into how abdominoplasty can alleviate these symptoms. This procedure is about functionality and comfort, not just aesthetics.
Required Documentation and Diagnostic Imaging
Proper documentation is essential for claiming the Medicare rebate for post-pregnancy abdominoplasty. This starts with a GP referral outlining the patient’s symptoms, the date of the last pregnancy, and a request for an ultrasound of the rectus wall, establishing the medical necessity of the procedure.
Diagnostic imaging is crucial for confirming diastasis recti, with a separation of at least 3 cm required to meet Medicare criteria. Comprehensive medical records, including conservative treatment outcomes and associated symptoms, are essential for Medicare approval of the surgical procedure.
Explanatory notes and diagnostic imaging prior to the procedure ensure all necessary steps are followed, making the claim process smoother and more efficient. Having the right paperwork supports your case.
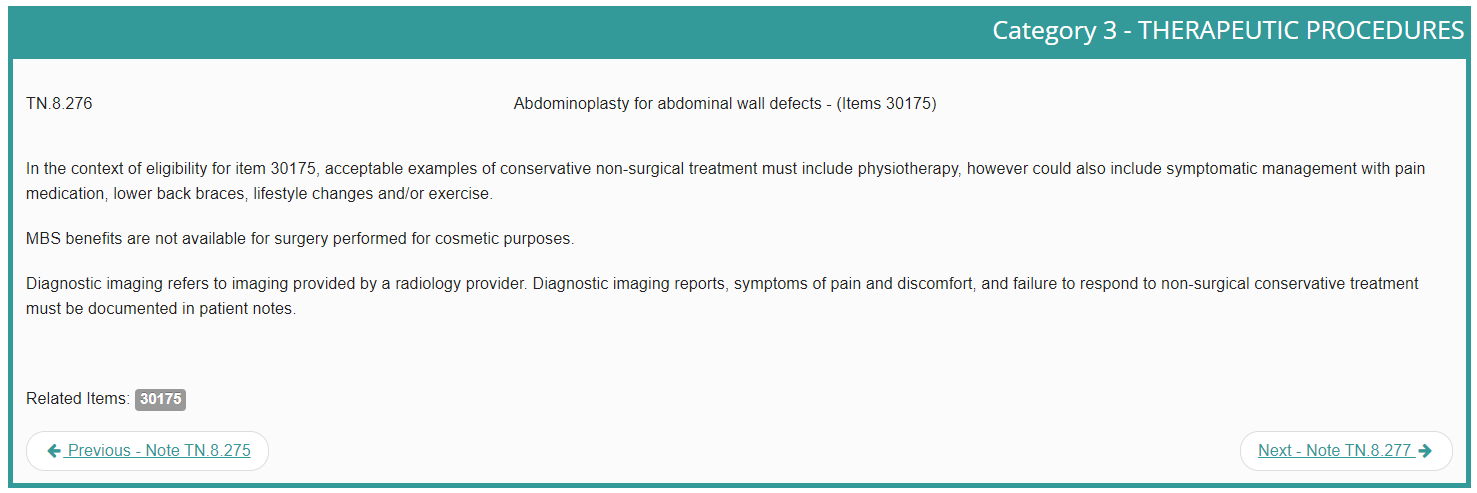
The Role of Non-Surgical Conservative Treatment
Patients must demonstrate that non-surgical conservative treatments, such as physiotherapy, lifestyle adjustments, and symptomatic management, have been ineffective before qualifying for surgery. Physiotherapy services specialising in abdominal muscle separation can be particularly helpful in managing the condition before considering surgery.
Conservative treatments may also involve pain medication, lower back braces, and exercise routines. The aim is to exhaust non-surgical options before considering surgery, and documentation showing the failure of these treatments is essential for Medicare approval when claiming abdominoplasty.
Patients must have attempted these non-surgical treatments and not been pregnant in the last 12 months to qualify for the rebate, ensuring that surgery is a last resort reserved for those who genuinely need it.
Outcomes and Benefits

Disclaimer: Operation performed by Dr Bernard Beldholm. Adult content, surgery has risks; individual results vary, seek 2nd opinion. Please see the full disclaimer.
Abdominoplasty offers various benefits, increasing core strength and enhancing overall function. The procedure specifically treats rectus diastasis, which impacts physical stability and core strength after pregnancy. Repairing this condition can reduce chronic pain.
Lower back pain, commonly caused by weakened core muscles, can be significantly alleviated through surgery. These outcomes highlight the functional use of the procedure beyond cosmetics.
The Medicare Benefits Schedule aims to provide these benefits to eligible mothers, ensuring access to necessary medical services. Increased core strength and reduced discomfort can significantly impact daily life, helping mothers regain physical stability.
Cost and Medicare Rebate Details

The new MBS item number aims to alleviate the financial burden of surgery. The Medicare benefit for abdominoplasty under item 30175 is $828.90, 75% of the total schedule fee of $1,105.15. This rebate is a crucial support for eligible mothers, making the surgery more accessible.
Medicare does not provide rebates for abdominoplasty performed for purely cosmetic reasons. Eligible mothers can only use the rebate once in their lifetime, emphasising the importance of meeting all eligibility criteria.
Find out more amount the cost of an abdominoplasty in my detailed article on the subject: “What is the Average Cost of Abdominoplasty (Tummy Tuck) Surgery in Australia?”
Dr Beldholm’s Final Thoughts

In my opinion, the MBS item number for post-pregnancy abdominoplasty marks a significant advancement in supporting mothers who suffer from muscle separation (Diastasis recti) after pregnancy. Understanding the eligibility criteria, required documentation, and the role of non-surgical treatments is crucial for eligible mothers to make informed decisions.
This initiative not only helps with the physical challenges faced by postpartum women but also provides financial relief, making essential medical procedures more accessible. If you meet the criteria, I encourage you to consult with your GP.
Frequently Asked Questions
What percentage of mothers experience abdominal muscle separation (diastasis recti) after pregnancy?
About 60% of moms deal with abdominal muscle separation (diastasis recti) after pregnancy.
What should patients do if they think they have diastasis recti?
If you think you have diastasis recti, inform your doctor about your symptoms and any treatments you’ve tried.
What is the new Medicare item number for abdominoplasty related to muscle separation?
The new Medicare item number for abdominoplasty related to muscle separation is MBS Item 30175.
How often can eligible mothers access the Medicare rebate for abdominoplasty?
Eligible mothers can access the Medicare rebate for abdominoplasty only once in their lifetime.
What are the eligibility criteria for the new Medicare item number?
To qualify for the new Medicare item number, you need to have diastasis recti from pregnancy, wait at least 12 months post-pregnancy, show a separation of 3 cm or more in your abdominal muscles, and have tried other treatments without success, along with documentation of moderate-to-severe pain.