Indications: Post-pregnancy loose skin, abdominal muscle separation, and femoral hernia with functional issues
Approach: Extended VASER Lipo-abdominoplasty (Tummy Tuck) with Diastasis Recti and Femoral Hernia Repair
Introduction
A 44 year-old female who experienced significant weight loss presented with a moderate amount of post-pregnancy loose abdominal skin that extended beyond the lower abdominal region, abdominal diastasis recti (separated lower abdominal muscles), and a left femoral hernia which was causing her pain and discomfort. I performed an Extended Abdominoplasty using VASER Liposuction, along with Diastasis Recti and Left Femoral Hernia Repair.

Book your appointment online now
Preparing the Patient/Markings in Anaesthetic Bay
Upon arrival at the hospital, the patient was asked to meet me in the anaesthesia bay where I answered any of her last minute questions and reviewed her complete medical history. I started by making incisional markings on her body as she stood upright, to allow me to be precise during surgery.
The anaesthetist began by administering premedications. Once in the operating room, the patient was given general anaesthesia.
Initial Abdominoplasty Incision

The first part of the operation is an incision across the lower abdomen, beyond the hips. I also released the umbilicus at this stage. This is an extended abdominoplasty.
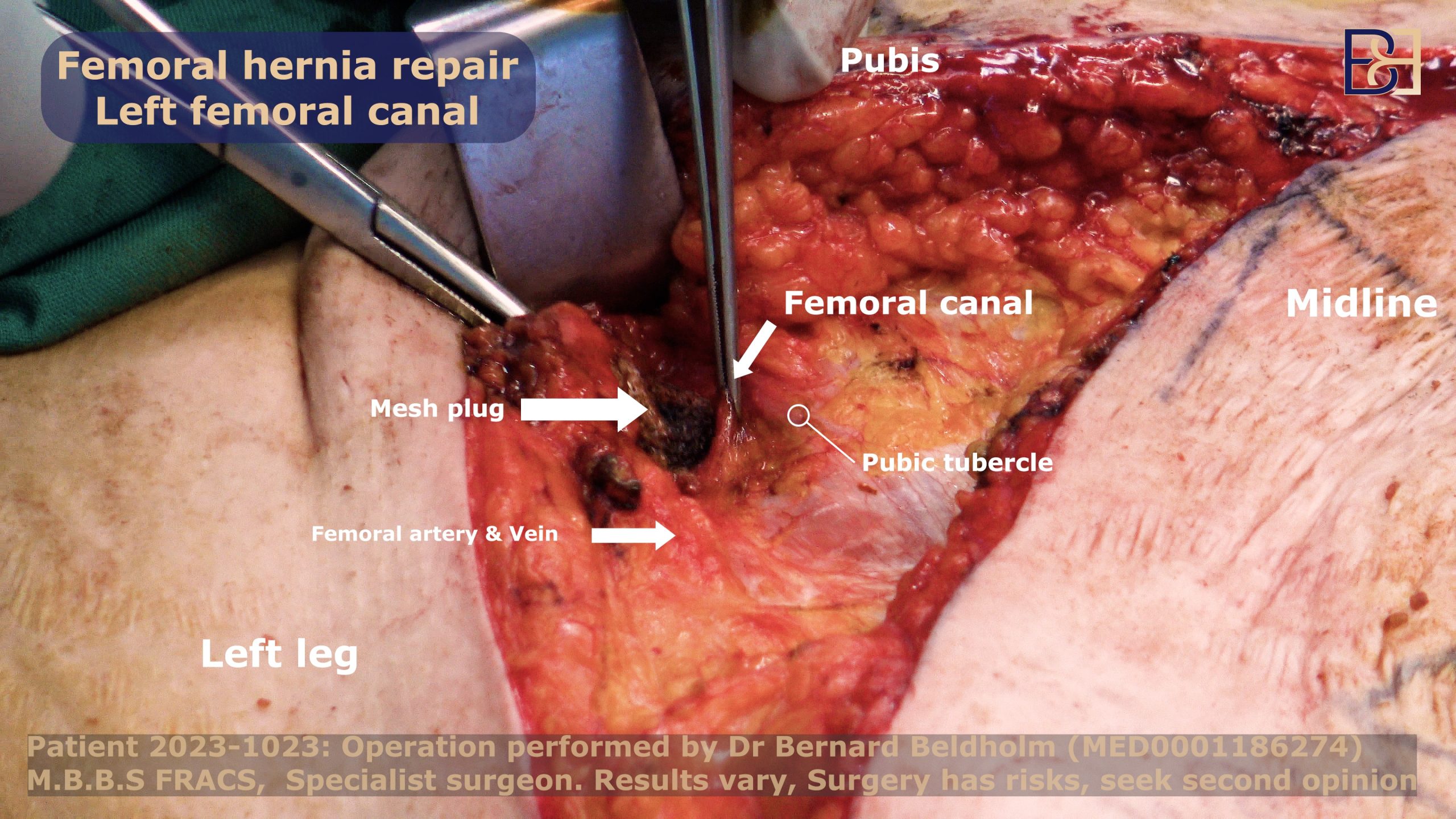
Femoral Hernia Repair as Part of the Abdominoplasty Surgery
Femoral hernia repair as part of abdominoplasty surgery is the next phase of the operation. Normally, a hernia repair is performed using a very small incision in the groin, but I use the same incision I use to perform the extended tummy tuck (Abdominoplasty). I use mesh and permanent sutures to secure it. The mesh will stay once the tissue heals, resulting in a very strong repair.
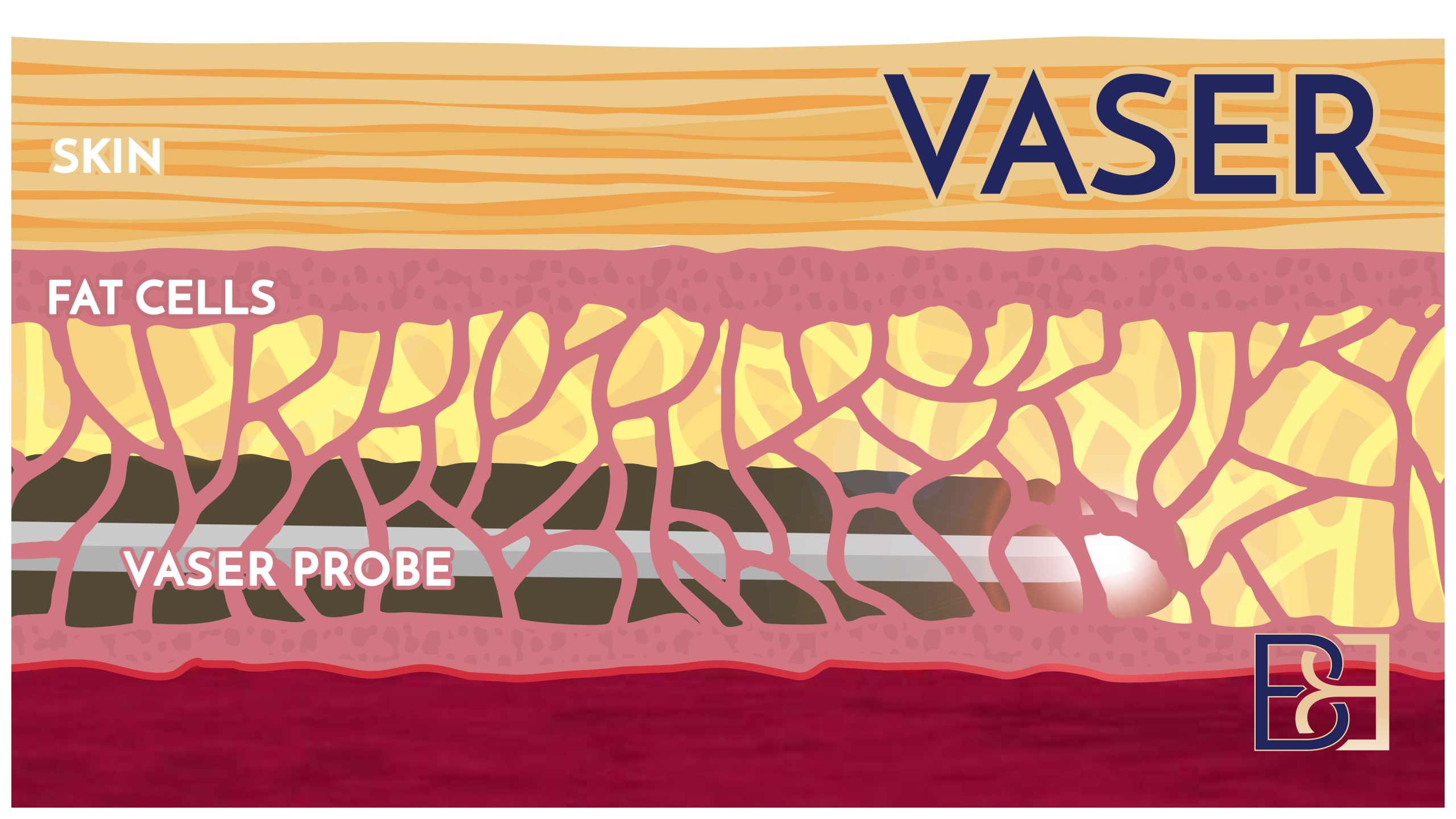
VASER Liposuction (Suction-assisted lipectomy) as Part of the Abdominoplasty Surgery
Because this particular patient had very little excessive fat, I only had to use VASER liposuction (Suction-assisted lipectomy) for 10 to 20 minutes. These are the steps involved.
- First, I inject tumescent fluid mixed with adrenaline and a local anaesthetic into the target area.
- Next, I make a small incision and pass the VASER (Suction-assisted lipectomy) ultrasound probe into the skin, focusing on the lateral and mons pubis areas.
- Because the VASER (Suction-assisted lipectomy) device gets hot, I place protective ports in the skin to prevent burns before introducing the probe.
- When the VASER (Suction-assisted lipectomy) is powered on, it vibrates to gently break down the fat cells.
- Once the fat reaches the consistency of liquid butter, I turn off the VASER and insert a cannula (a thin hollow tube).
- The tube is hooked up to a suction device, which suctions out the fat.
By targeting the specific areas with excess fat, VASER liposuction (Suction-assisted lipectomy) reduces the need for extensive tissue dissection. This technique helps me minimise damage to the underlying structures.
For a more in-depth look at my VASER-Liposuction abdominoplasty method for post-pregnancy patients, refer to this article: Two at Once? Can I Get Abdominoplasty and Liposuction at the Same Time?
Freeing the Umbilicus in Abdominoplasty Surgery
Abdominoplasty (tummy tuck) surgery begins by first freeing the umbilicus (navel). The reason for moving the belly button is that when the skin is cut away to create a smooth, flat tummy, the skin is pulled taut to close the incision. As the skin is pulled down, the belly button is pulled down as well. This makes the belly button sit too low on the tummy, which looks unnatural. Therefore, the surgical procedure also involves relocating the belly button so it sits in a more natural position.
Because the navel sits deep in the abdomen, I carefully cut around it, then pull the loose abdominal muscles and skin downward after removing excess skin. This leaves the patients with a flat tummy. Once the skin is pulled down, I create a new hole in the abdomen for the newly structured navel.
First Dissection/Dissecting the Lower Abdominal Flap
I make an incision on the upper abdomen from where I made the initial markings. I prefer straight incisions, (90 degree angle to the skin) since they heal better than bevelled ones. After the incision, I separate the skin from the underlying tissue, staying just below Scarpa’s fascia to preserve blood vessels, aiding in a speedier recovery.
In case any blood vessels happen to burst during dissection, I will use the diathermy technique to coagulate tissues and control bleeding. Once I reach the belly button, I will then create an epigastric tunnel in the abdomen to get a clear view of the linea alba and see the extent of muscle separation.
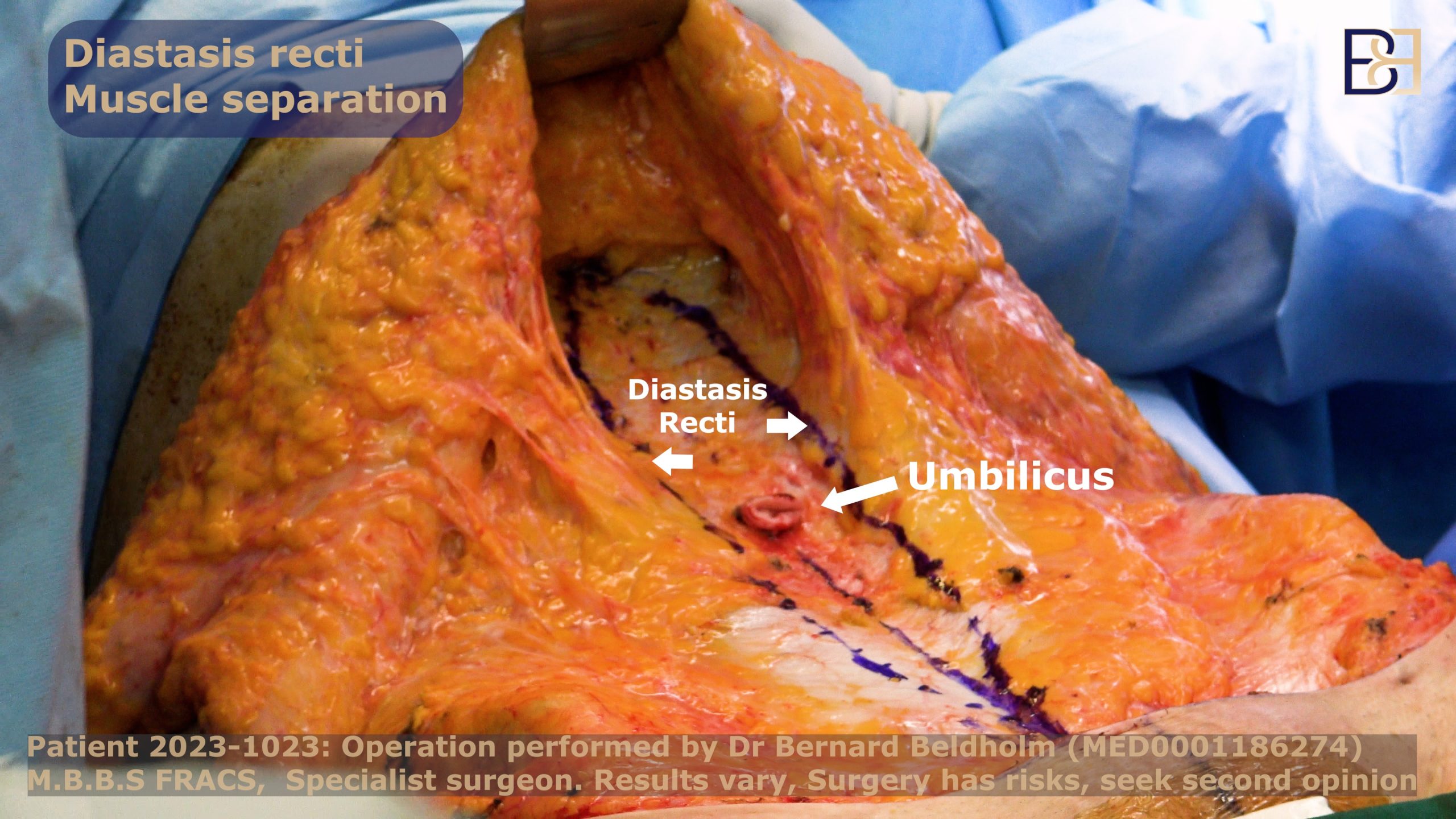
Repairing Diastasis Recti
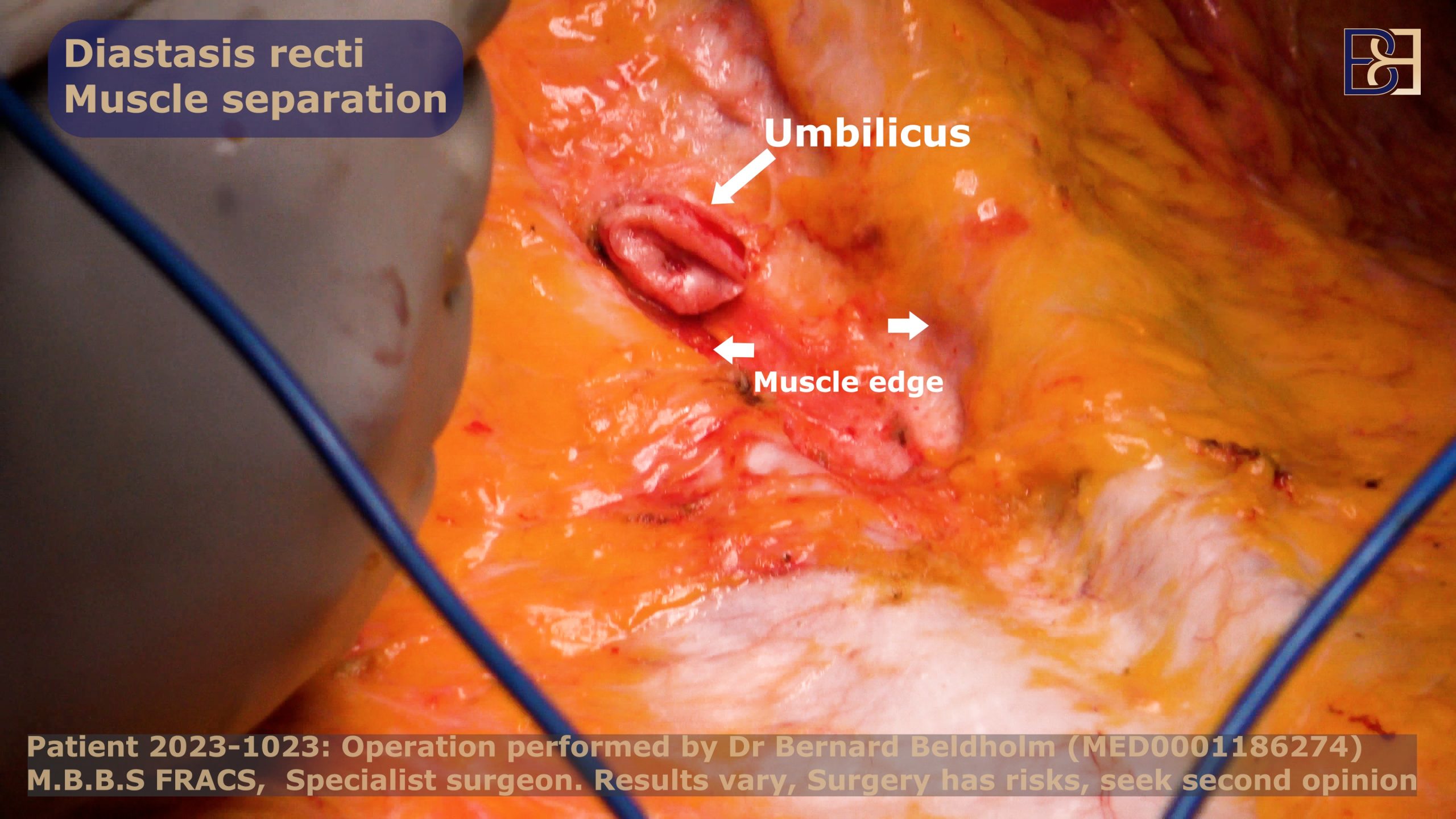
The main function of the rectus muscles is to provide strength to the core muscles which can separate due to multiple pregnancies or massive weight loss. This causes a protruding belly and torn abdominal muscles. To perform muscle repair during surgery, I bring the separated muscles together using barbed sutures called V-Loc 1 permanent sutures, which do not require knotting to guarantee a durable and effective repair at the incision site.
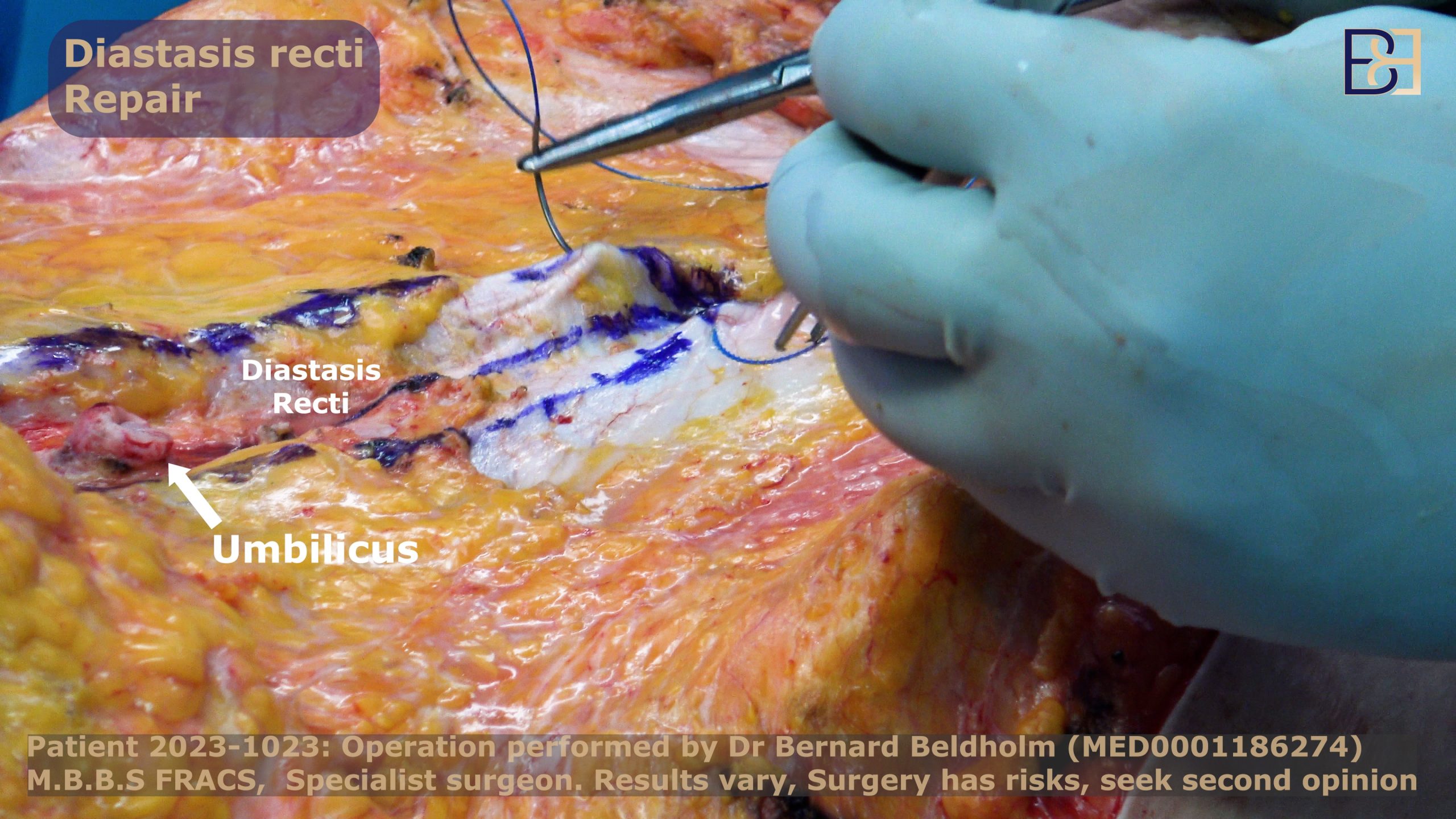
My technique involves two layers of sutures, with the final layer being only in the abdominal sheet and not any deeper, so as not to damage the nerves, muscles, or blood vessels.

Last Dissection to Tighten Loose Skin
After I tighten the underlying muscles, a substantial amount of loose skin will be left hanging. During the last dissection, I will bend the operating table slightly.
Bending Operating Table for Correct Amount of Tightness
By tilting the table 15° to 20° degrees, I attain the correct amount of tightness before stitching the umbilicus as umbilical positioning is very important. I create a new hole and pull the stalk through, removing any fat underneath before suturing it in place.
Plication of the Lower Abdominal Wall
Using plication stitches, suturing the abdominal skin to the abdominal wall, minimises the space between the skin and the wall and puts tension on the abdominal wall and not the mons. I use progressive sutures to finalise the surgery to ensure that the wound is closed evenly, minimising the risk of the wound reopening. Progressive sutures secure the repaired tissues and reduce the likelihood of seroma formation. I also use tissue glue to reduce the chance of seromas.
Excess Skin Removal of the Lower Abdominal Wall
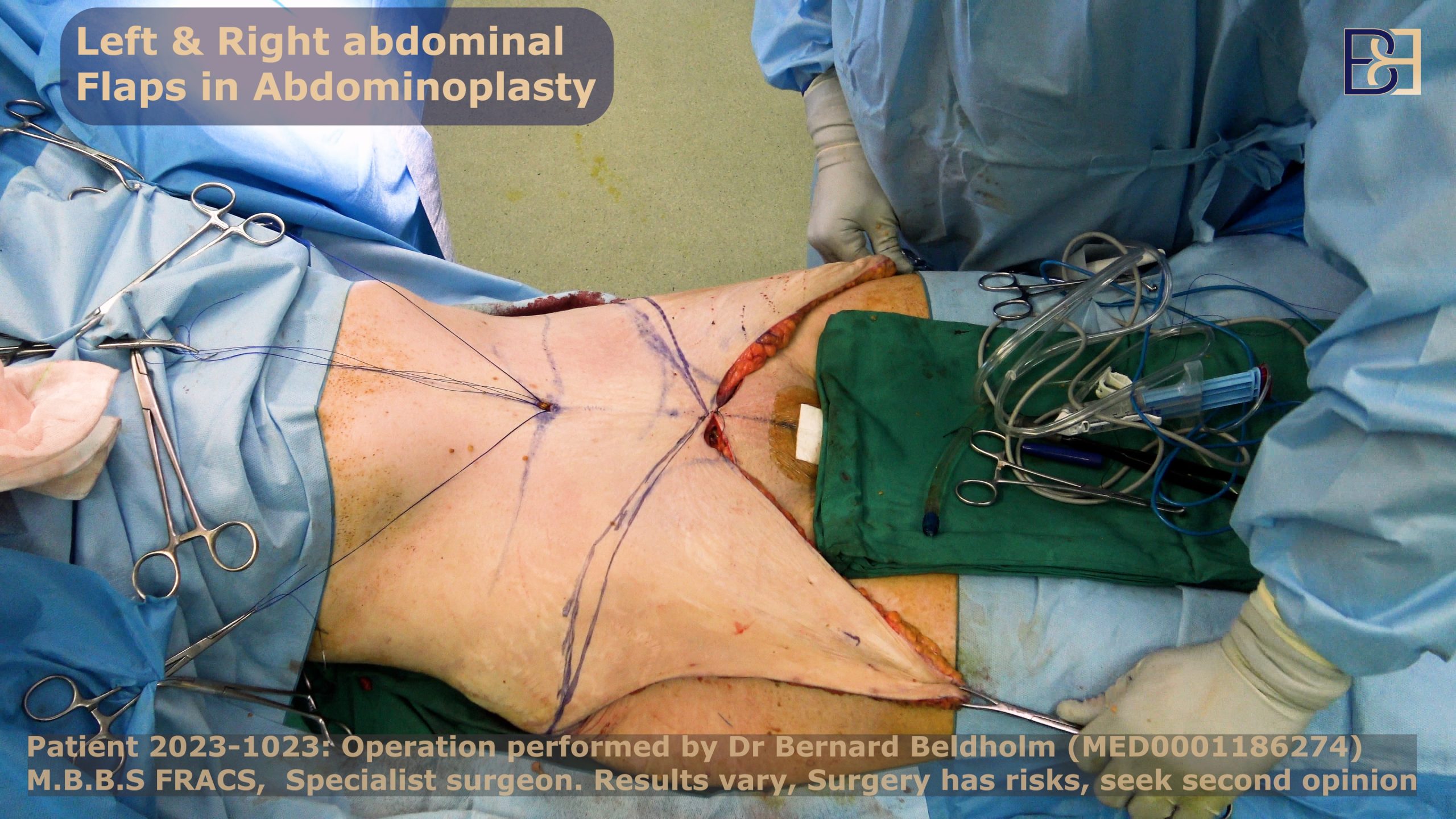
After repositioning the belly button, I will remove the excess skin I need to resect. Some general surgeons cut the excess skin by segments, but I opt to mark out the excess skin using Alice forceps, then resecting the skin as marked.

Applying PICO Dressing

After the abdominoplasty procedure, I carefully place PICO dressings on the patient’s incision wound. This device remains on the patient for 7 days.
Compression Garment
Additionally, wearing a compression garment is recommended to reduce swelling, provide support to the surgical site and area, promote proper healing, and aid in the recovery process.
What is the PICO System?
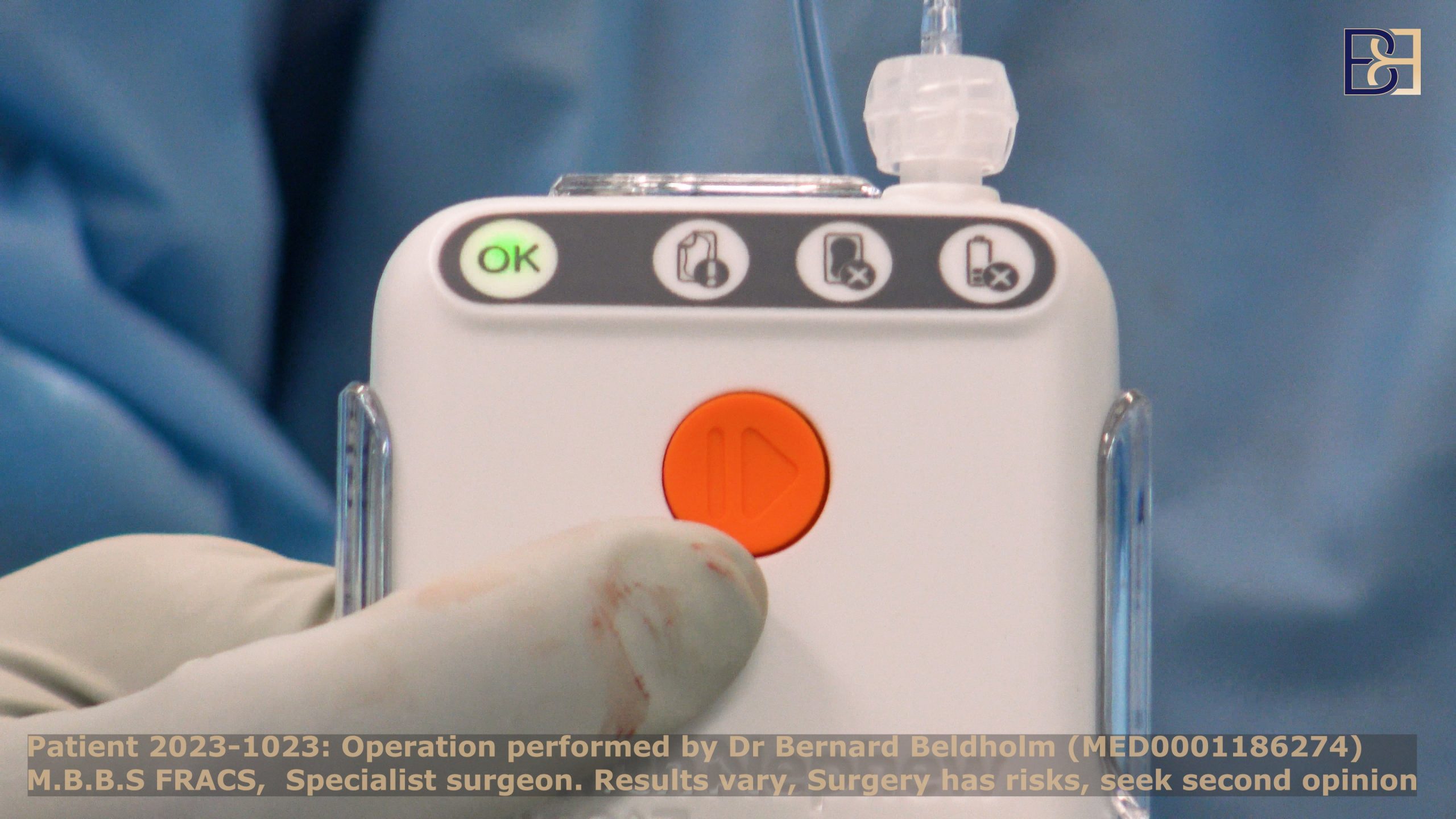
Suitable for home care settings, PICO Negative Pressure Therapy creates an ideal healing environment for incision wounds. With powerful components that work together to promote healing, reduce the chances of developing complications, and prioritise the patient’s comfort, the PICO system works by drawing out excess fluids from the wound while applying pressure, safeguarding the affected area from contamination, and fostering optimal healing.
The PICO Negative Pressure device features two dressing kits and a sterile pump that creates negative pressure on the entire wound surface, which effectively promotes healing. Generating negative pressure (80mmHg nominal), the sterile dressing kits keep the wound dry by absorbing any discharge and evaporating it through the outer layer.
Procedure Performed on this Patient 2023-1023
- 100 ml of fat removed with VASER liposuction surgical procedures
- Abdominal skin removed
- Right side: 337 grams
- Left side: 382 grams
- Femoral hernia repaired
- Diastasis recti repaired
FAQs
How soon after pregnancy can I get abdominoplasty surgery?
I highly recommend that my patients wait at least twelve months after pregnancy before undergoing abdominoplasty (tummy tuck) surgery because it gives the body time to heal and allows loose skin to shrink on its own, while also allowing mums time to spend bonding time with their baby.
Is abdominoplasty covered by Medicare?
Medicare will cover your abdominoplasty surgery if it is deemed medically necessary. If you meet the specified criteria, such as if the excess skin and fat are affecting your work and daily life, you may qualify for a Medicare Benefits Schedule (MBS) Item Number.
What Is Diastasis Recti?
Diastasis recti is defined as an inter-rectus distance (IRD) of 22 mm, three cm above the umbilicus. The connective tissue between the muscle is called the linea alba which can become stretched during pregnancy or weight gain. This leads to leading to muscle separation which can be repaired with reconstructive surgery.
The degree of separation varies from one individual to the next depending on what caused diastasis recti among other factors. In some cases, the degree of separated muscles is minimal and barely visible externally. In other cases, there can be an observable pouch of hanging skin and fat.
Diastasis recti is the weakening and stretching of the abdominal muscles. Commonly known as the “six-pack,” this happens when the connective tissues that hold the rectus abdominis muscles together (linea alba) stretch forward to accommodate a growing foetus.
How can I tell if my abdominal muscles were torn during pregnancy?
Diastasis recti can go undetected if you aren’t sure what to look for. Below are some of the symptoms of diastasis recti.
- A jelly-like texture around the navel: Excess tissue or decreased muscle tone causes skin’s texture around the belly button to change.
- Difficulty lifting and performing everyday tasks: The rectus abdominis muscles give the abdomen strength to do basic tasks like lifting. Weak muscles make daily tasks difficult.
- Pain: Core muscles support the spine during movement. Weak abdominal muscles cause imbalance and overuse of the pelvic and hip muscles.
- Urinary Incontinence: Weak abdominal muscles can cause bladder disruption, leading to involuntary urine leakage.
- Back pain: Lack of core strength puts a lot of pressure on the lower back muscles, resulting in back pain.
- Visible protrusion: The separation of abdominal muscles causes the belly to protrude, giving the illusion of pregnancy even after giving birth.
- Poor posture: Weakened core muscles make it difficult to adequately support the spine, causing a slouch.
- Constipation: Diastasis recti can impact the movement of the bowels, leading to constipation.
- Coning or doming of the abdominal muscles during physical exertion: When abdominal muscles are separated, they protrude outwards when sitting or lifting heavy objects.
- Lack of core muscle strength: Diastasis recti makes it challenging for core muscles, such as the abdominal and lower back muscles, to function normally.
- Pain during intercourse: You may experience pain during intense activities like intercourse due to poor abdominal support.
At-Home Test for Muscle Separation

If you have the symptoms of diastasis recti, taking the test below can confirm whether you indeed have muscles separation.
- Step 1: Lay flat on your back and bend your knees, keeping your feet flat on the floor.
- Step 2: Place one hand horizontally across your midsection.
- Step 3: Slowly position yourself in a mini-crunch.
- Step 4: Feel for gaps between the rectus abdominis (abdominal muscle). You may also notice a jelly-like texture around the navel.
- Step 5: If you feel a gap of more than one finger in width, your abdominal muscles could be separated.
Related article: How to Tell if Your Abdominal Muscles Were Torn (Diastasis Recti) During Pregnancy
Is abdominoplasty considered major surgery?
Abdominoplasty is considered major surgery because not only does it remove significant amounts of excess skin, the body’s largest organ, but it alters the body’s anatomical structure, is a complex procedure with potential for risks, involves the use of general anaesthesia, and requires a hospital stay.