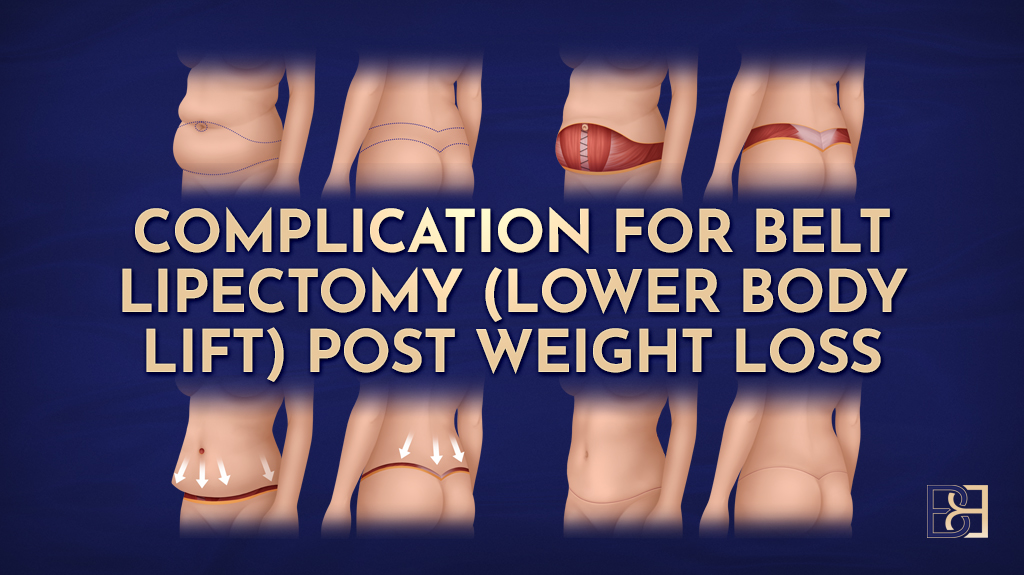
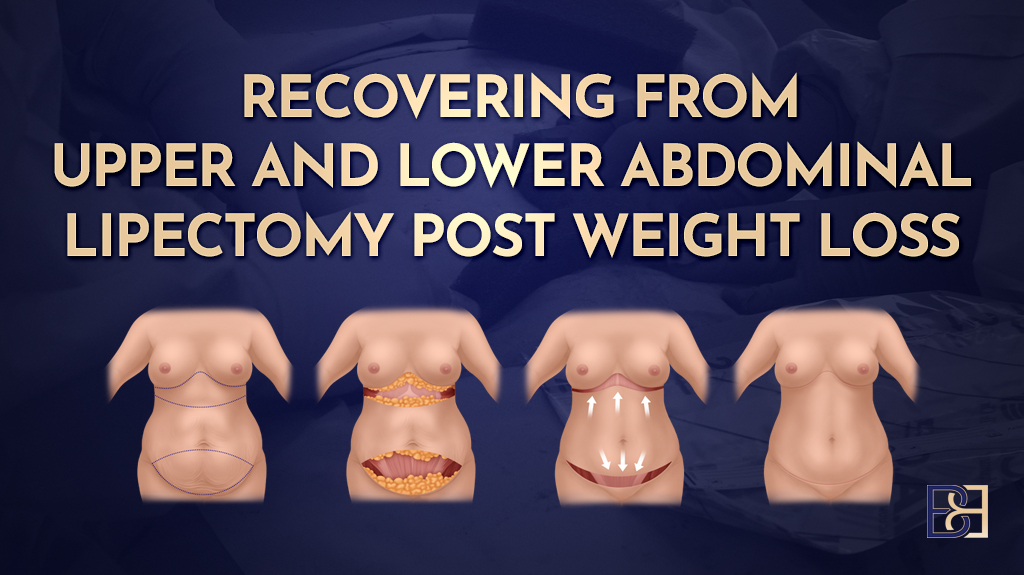
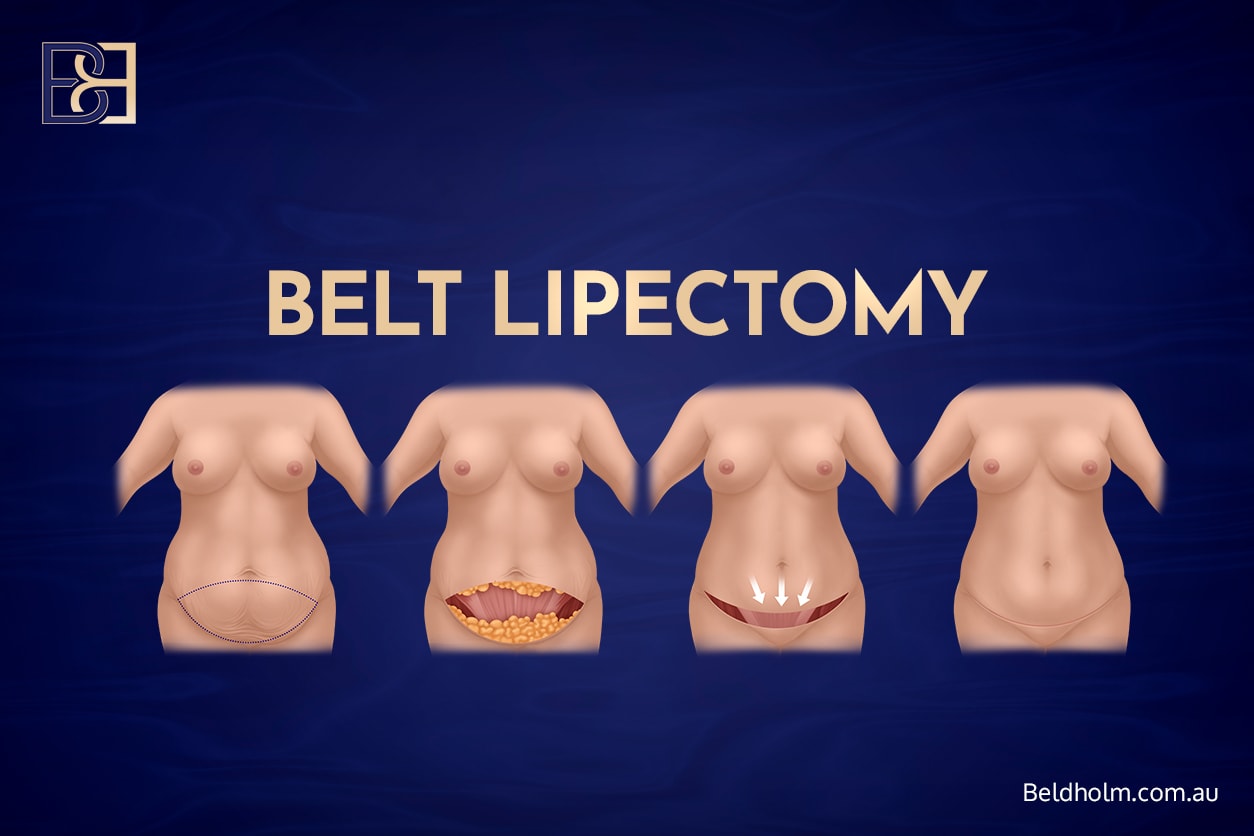
A belt lipectomy, sometimes called a lower body lift, is a major body-contouring procedure designed to remove excess skin and fat around the entire torso after significant weight loss or bariatric surgery. Many patients with significant weight loss choose this operation to address loose skin, improve hygiene issues such as rashes, and achieve new body contours that conform to their lower-body shape.
While a belt lipectomy can reshape the lower abdomen, flanks, hips, buttocks, and outer upper thighs, it is also among the more complex body-contouring procedures available. The procedure involves the removal of excess skin and fat as key components to improve body contour and appearance. Because it involves a long circumferential incision and works across the entire torso, there are meaningful risks that every patient should understand before committing to surgery.
It is important to be aware of the risks of belt lipectomy and fully understand them before undergoing the procedure.
Why Complications Can Occur After a Belt Lipectomy

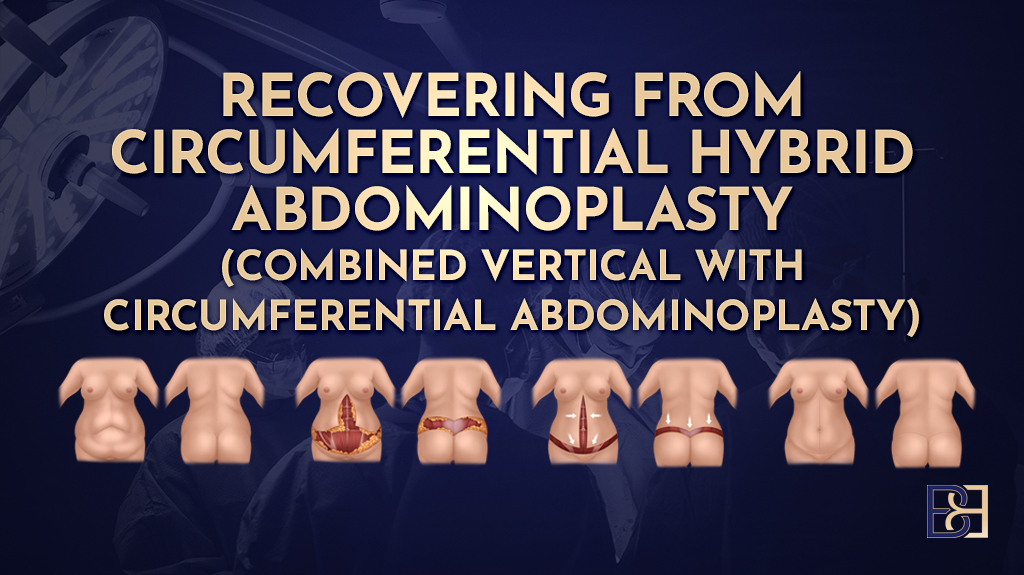
A belt lipectomy is a surgical procedure performed under general anaesthesia. It is designed to remove excess skin after weight-loss surgery, significant weight loss, or other weight-loss methods. Because the operation combines elements of a tummy tuck (Abdominoplasty), flank lift, and buttock lift (Gluteoplasty) into a single circumferential procedure, the body must heal a long incision line and adapt to changes in tension around the lower torso.
Complications can occur for several reasons:
- Altered skin elasticity after weight loss
- Reduced blood supply in stretched skin
- Nutrient deficiencies are common after bariatric procedures, which can affect wound healing
- The length of the incision and the tension on the wound
- Degree of tissue dissection
- Medical comorbidities
- Smoking, which severely affects wound healing
Understanding potential complications helps patients prepare realistically for their recovery period.
Candidate Selection and Preparation

Selecting appropriate candidates and ensuring thorough preparation are essential to a safe and successful lower-body lift (belt lipectomy). Because this body contouring surgery is a major procedure—often performed on patients who have experienced massive weight loss or undergone bariatric surgery—careful assessment and planning can significantly reduce the risk of complications.
Common Complication Types and How They Are Managed
Below are the key complications that can follow a belt lipectomy. Surgical complications and complication rates are important considerations for patients undergoing belt lipectomy, as these risks can vary based on individual health factors and preparation.
Wound Dehiscence (Wound Separation)

Wound dehiscence is one of the most common complications after a belt lipectomy, with reported rates ranging from 17% to more than 30%, depending on the study and surgical technique [1–3]. It occurs when part of the incision line partially reopens during healing. In most cases, this separation is small — typically a few millimetres to a couple of centimetres and occurs along areas of greatest tension, such as the hips or central abdomen. Skin quality, particularly reduced skin elasticity after significant weight loss, can further increase the risk of wound dehiscence by making wound closure more challenging and affecting the healing process. It does not mean that the entire wound opens, nor does it usually expose deeper tissues.
Why It Happens
Several factors make wound separation more likely after a belt lipectomy:
- High wound tension from removing large amounts of skin, especially in the upper abdomen, where tissue removal and repositioning increase stress on the closure
- Large tissue resections creating increased pull on the closure
- Low protein levels, which impair skin healing
- Smoking, which reduces blood flow and oxygenation to tissues
- Diabetes, due to microvascular changes
- Early stretching or excessive movement during recovery
These factors reduce the skin’s ability to stay closed while healing.
How Common It Is
- Meta-analyses report wound dehiscence rates of approximately 17% [1], as documented in clinical research.
- Individual large series report rates ranging from 32–61%, depending on technique and patient factors [2,3], according to studies published in clinical medicine journals.
While the numbers may seem high, most of these separations are minor, small, and manageable.
How It Is Managed
Treatment depends on the size of the opening:
Small openings:

- Regular wound dressings (foam, gauze, hydrocolloids)
- Protecting the area from friction
- Keeping the wound clean and dry
- Avoiding stretching movements
Moderate openings:
- Dressings plus negative‑pressure wound therapy (NPWT) to help close the wound
Large openings (rare):
- May require minor revision surgery to re‑close the area once swelling settles
Antibiotics are only required if signs of infection are present.
How Long It Take to Heal
- Small areas: 2–3 weeks with simple dressings
- Moderate areas with NPWT (Negative Pressure Wound Therapy): 3–6 weeks
- Larger areas requiring revision: 6–8+ weeks, depending on healing and overall health
Most wound dehiscence issues do not affect the final contour or long‑term outcome, but they can slow recovery and require additional dressing care.
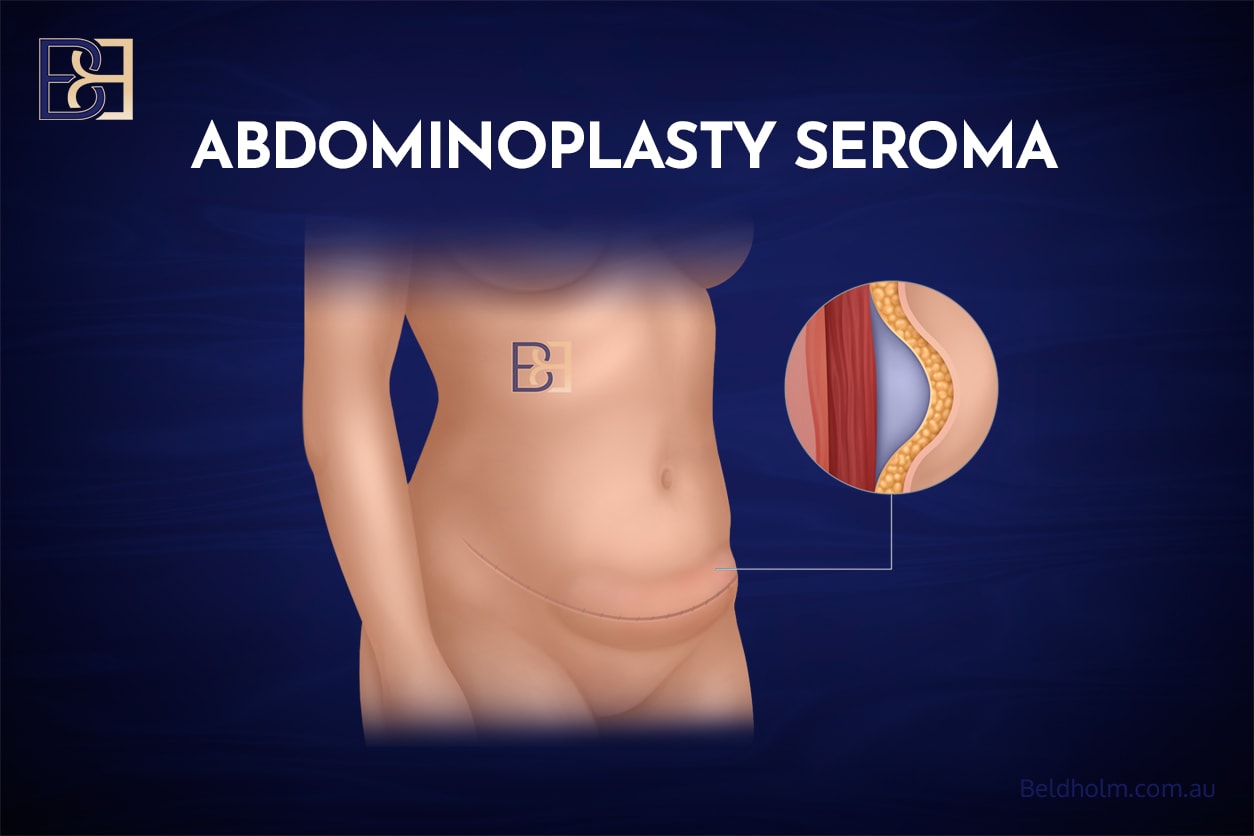
Seroma (Fluid Collection)
Note: Wound dehiscence occurs more frequently than seroma in most studies, making seroma a common but not the most common complication.
A seroma is a common complication after belt lipectomy, with published rates ranging from 9% to 35% depending on the surgical technique and extent of tissue dissection [1,3]. It refers to a collection of clear, straw‑coloured fluid that accumulates under the skin where tissue was removed. The removal of extra skin after significant weight loss, along with the potential for excessive bleeding during surgery, can increase the risk of postoperative wound complications such as seroma.

What a Seroma Is
A seroma forms when the space created during surgery (the “dead space”) fills with fluid instead of healing immediately. The abdomen, flanks, and lower back are common locations for seroma formation.
Patients may notice:
- Localised swelling
- A sloshing or fluid‑shift sensation
- Discomfort or tightness
- Clear or slightly blood‑tinged drainage
Why It Happens
Seromas are more likely in situations where:
- Large areas of tissue were removed, creating a wide dead space
- The patient moves too quickly in early recovery
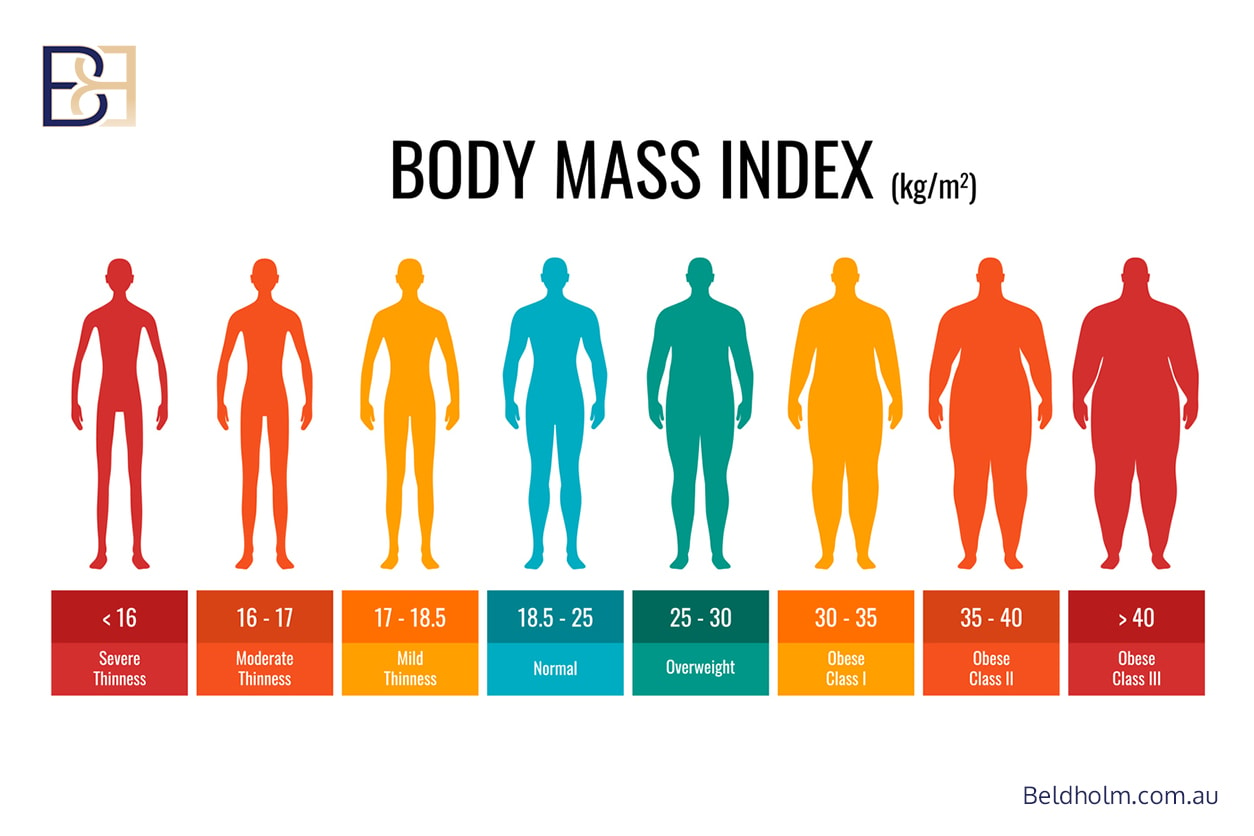
- The BMI is higher, adding weight and tension to the wound
- Drains are removed before the output is low
- There is a history of seromas from previous surgeries
How Common It Is
The literature reports:
- 13% seroma rate in meta‑analysis of body lifts [1]
- Up to 35% in limited‑undermining techniques where dead space still forms despite preserved blood supply
How It Is Managed
Most seromas are not dangerous but may be uncomfortable.
Common treatments include:
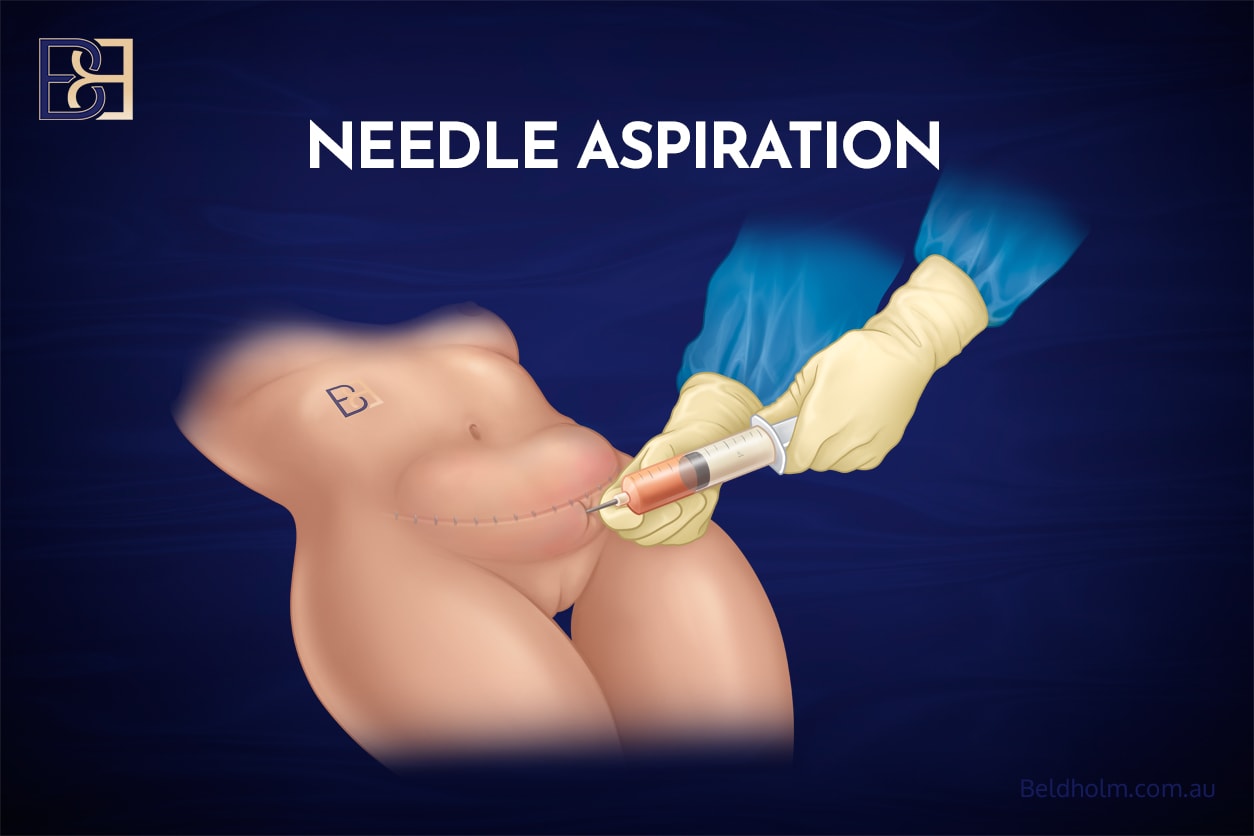
- Needle aspiration: Removal of the fluid using a fine needle; may need 1–3 repeat sessions
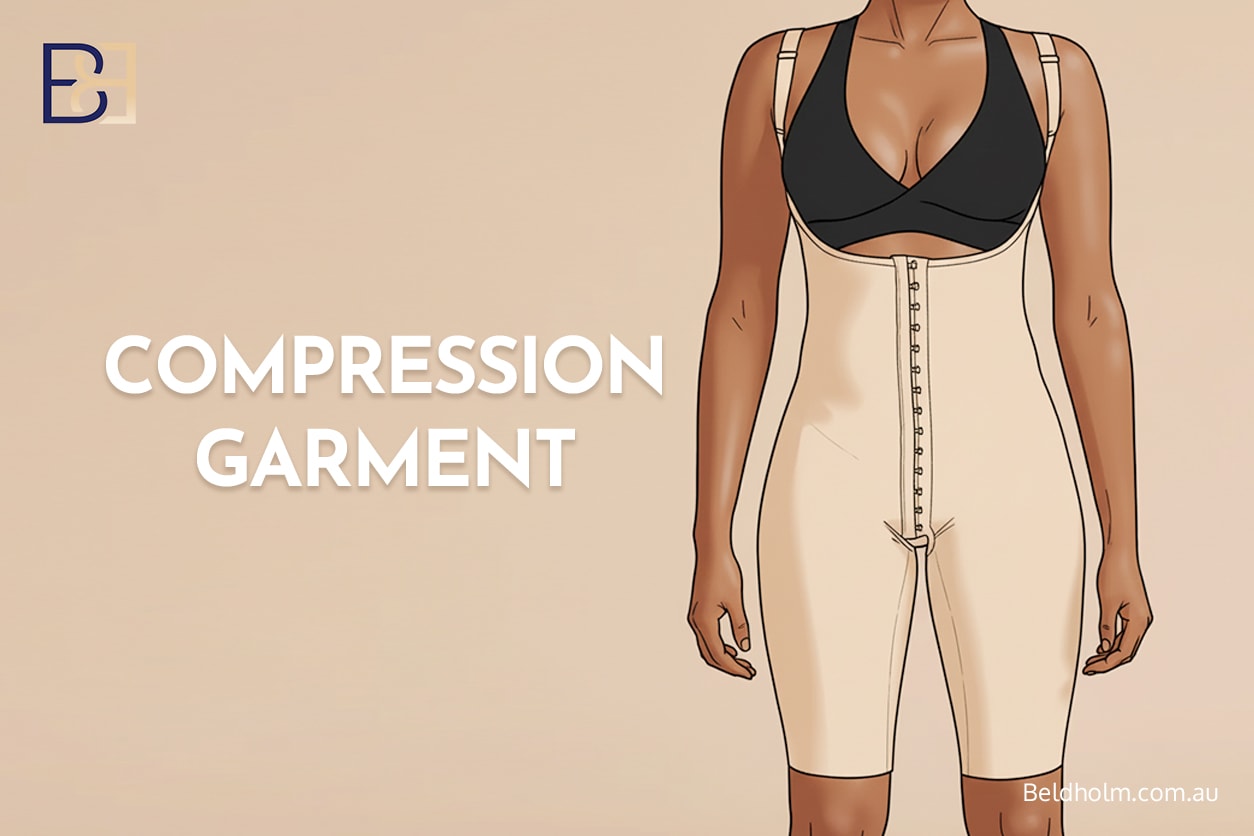
- Compression garments: Help tissues adhere and reduce fluid production
- Drain management: Drains may be left in longer if output remains high
- Sclerotherapy: Injection of a mild irritant such as doxycycline for persistent seromas
- Rare surgical intervention if a capsule forms around the fluid
How Long Does It Take to Resolve
- Small seromas: 1–3 weeks
- Larger seromas: 3–6+ weeks, especially if weekly aspiration is needed
- Chronic seromas with a capsule (rare): 6–12 weeks, sometimes longer if surgery is required
Most seromas heal without long‑term problems.
Skin Necrosis (Poor Blood Supply)
Skin necrosis refers to tissue that does not receive adequate blood flow after surgery and begins to die. Reported rates vary from 1–10% depending on technique, smoking history, and tissue quality [1,2,4]. Necrosis typically develops in the first few weeks after surgery and, if extensive, can be considered one of the major complications of belt lipectomy post weight loss.
What Skin Necrosis Is
Necrosis occurs when small or large areas of skin become:
- Darkened or black
- Firm or leathery
- Slow to heal
- Scabbed with dry or hardened tissue
This is generally a localised complication, not a systemic one.
Why It Happens
Risk factors include:
- Smoking, the strongest contributor due to reduced oxygen delivery
- Tight wound closure, reducing the blood supply to the edges
- Thin, stretched skin after major weight loss
- Aggressive undermining or liposuction, which compromises blood vessels
- Diabetes, which affects microvascular circulation
How It Is Managed
Management depends on severity:
Small superficial areas:
- Regular dressing changes
- Gentle cleansing
- Protection from pressure
Moderate necrosis:
- Negative‑pressure wound therapy to stimulate blood flow
- Allowing tissue to demarcate naturally
Large/full‑thickness necrosis:
- Surgical removal of dead tissue (debridement)
- Possible delayed closure or skin grafting in severe cases
How Long Does It Take to Heal
- Small areas: 3–4 weeks
- Moderate areas: 4–8 weeks
- Extensive necrosis needing surgery: 8–12+ weeks, depending on wound size and patient health
Necrosis can prolong recovery significantly but is treatable.
Book your appointment online now
Infection

Infection after a belt lipectomy can present in several different ways, ranging from minor superficial inflammation to deeper infections that require hospital‑level treatment. Reported infection rates range from 3–9% in systematic reviews [1,3]. Wound infections are a common concern after belt lipectomy, often occurring shortly after surgery and presenting with symptoms such as pus, redness, and warmth at the surgical incision. Because infection can delay wound healing and prolong recovery, it is helpful to understand the different types, how they are managed, and how long recovery typically takes.
Superficial Infection (Local Cellulitis), also referred to as Superficial Surgical Site Infection (SSI)
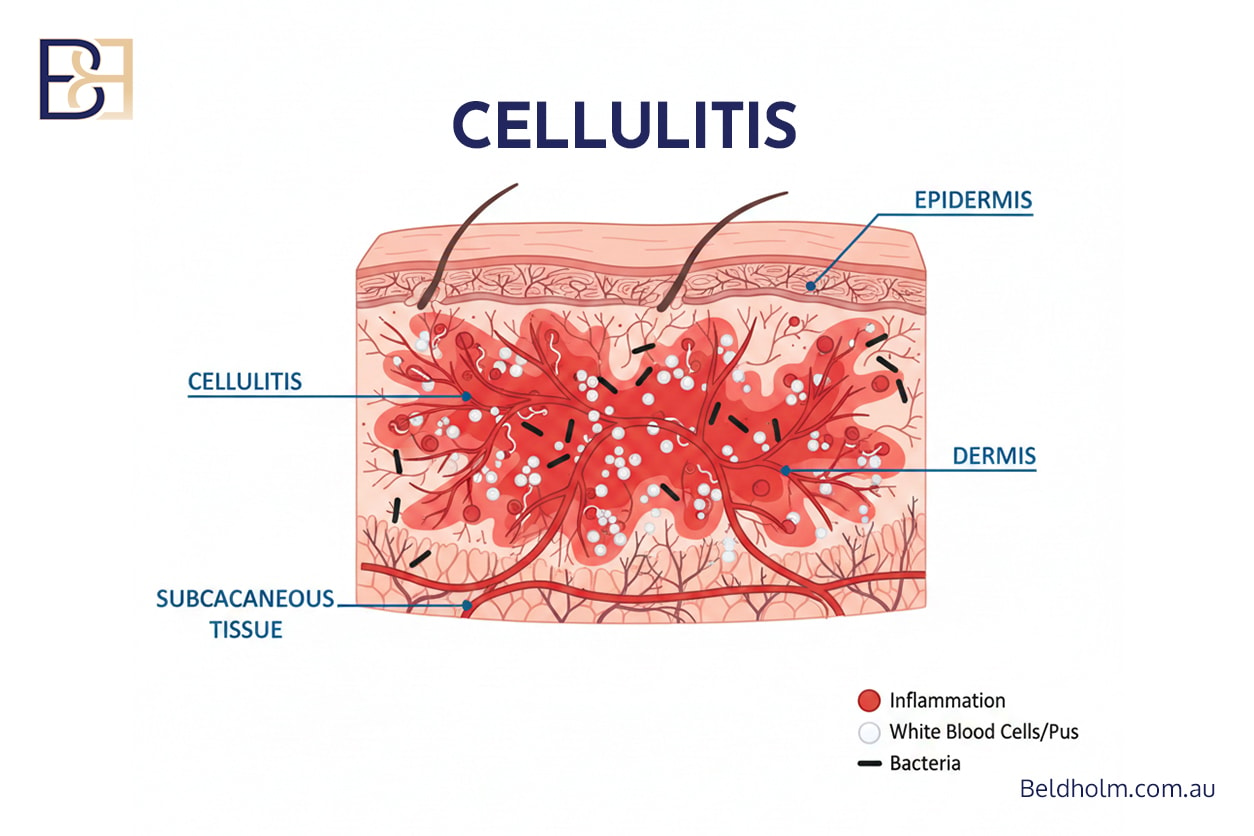
This is the most common and least severe type of infection. It affects only the upper layers of the skin.
What it looks like:
- Redness around the wound
- Warmth and tenderness
- Localised swelling
- No fevers or systemic symptoms
Why it happens:
- Mild bacterial contamination at the incision line
- Friction or moisture in skin folds
- Irritated sutures or tension points
How it is managed:
- Outpatient treatment
- Oral antibiotics targeting common skin bacteria
- Local wound care and monitoring
Healing time:
- Usually, within 48–72 hours of antibiotics
- Resolves fully within 5–10 days
Cellulitis With Systemic Symptoms
This type of infection spreads beyond the incision into deeper layers of the skin and may enter the bloodstream.
What it looks like:
- Redness that is spreading quickly
- Increasing pain or heat
- Fever, chills, or feeling unwell
- Occasionally nausea or fatigue
Why does it happen?
- Bacteria enter through a compromised section of the incision
- Immune system or nutrition issues
- Occurs more often when a seroma or dehiscence is present
How it is managed:
- Readmission to the hospital may be required
- Intravenous (IV) antibiotics
- Monitoring of vital signs and blood tests
- Ultrasound scans if deeper infection is suspected
Healing time:
- Early, within 2–4 days of IV antibiotics
- Full recovery often takes 2–4 weeks, depending on severity
Deep Infection / Abscess
A deep infection forms a collection of pus underneath the skin, known as an abscess. This is the most serious form of postoperative infection.
What it looks like:
- Increasing one‑sided swelling
- Severe tenderness
- Difficulty standing upright
- Fever and chills
- Thick, cloudy or foul‑smelling drainage
Why does it happen?
- Bacterial contamination in deeper tissues
- Presence of a seroma that becomes colonised
- Breakdown of internal sutures or tissue pockets
How it is managed:

- Requires active surgical treatment rather than antibiotics alone
- Incision and drainage (I&D) to release pus
- Placement of packing or negative‑pressure wound therapy (NPWT)
- Ongoing dressings and sometimes further antibiotics
Healing time:
- Initial recovery: 1–2 weeks
- Full wound healing: 4–6+ weeks, depending on cavity size and whether NPWT is needed
Summary
Superficial infections are the most common. Systemic infections and abscesses are less common but more severe and may require hospitalisation. Early recognition and treatment are key to preventing long‑term issues.
Infections generally resolve without long‑term problems when treated promptly and appropriately.
Haematoma (Bleeding Under the Skin)

A haematoma is an accumulation of blood under the skin, usually occurring within the first 24–72 hours after surgery. Excessive bleeding during or after surgery can increase the risk of haematoma, especially in patients with certain pre-existing conditions or those taking medications that affect blood clotting. Rates for haematoma are around 2–4% in circumferential procedures [1,3].
What a Haematoma Is
Haematomas may appear as:
- Firm swelling
- Bruised appearance
- Increasing pressure or pain on one side
- Asymmetry between the left and right sides
Why It Happens
Contributors include:
- Elevated blood pressure after surgery
- Bleeding from small vessels not fully sealed during the operation
- Straining, coughing, or early movement
- Use of blood thinners
How It Is Managed
Small haematomas:
- Monitoring
- Cold compresses in early stages
- The body reabsorbs the blood naturally
Larger or expanding haematomas:
- Urgent return to theatre to remove the clot and control bleeding
How Long Does It Take to Heal
- Small haematomas: 2–4 weeks to reabsorb
- Surgical evacuation: 4–6 weeks of recovery for swelling and bruising to settle
Haematomas are typically straightforward to treat when recognised promptly.
Blood Clots (Deep Vein Thrombosis and Pulmonary Embolism)
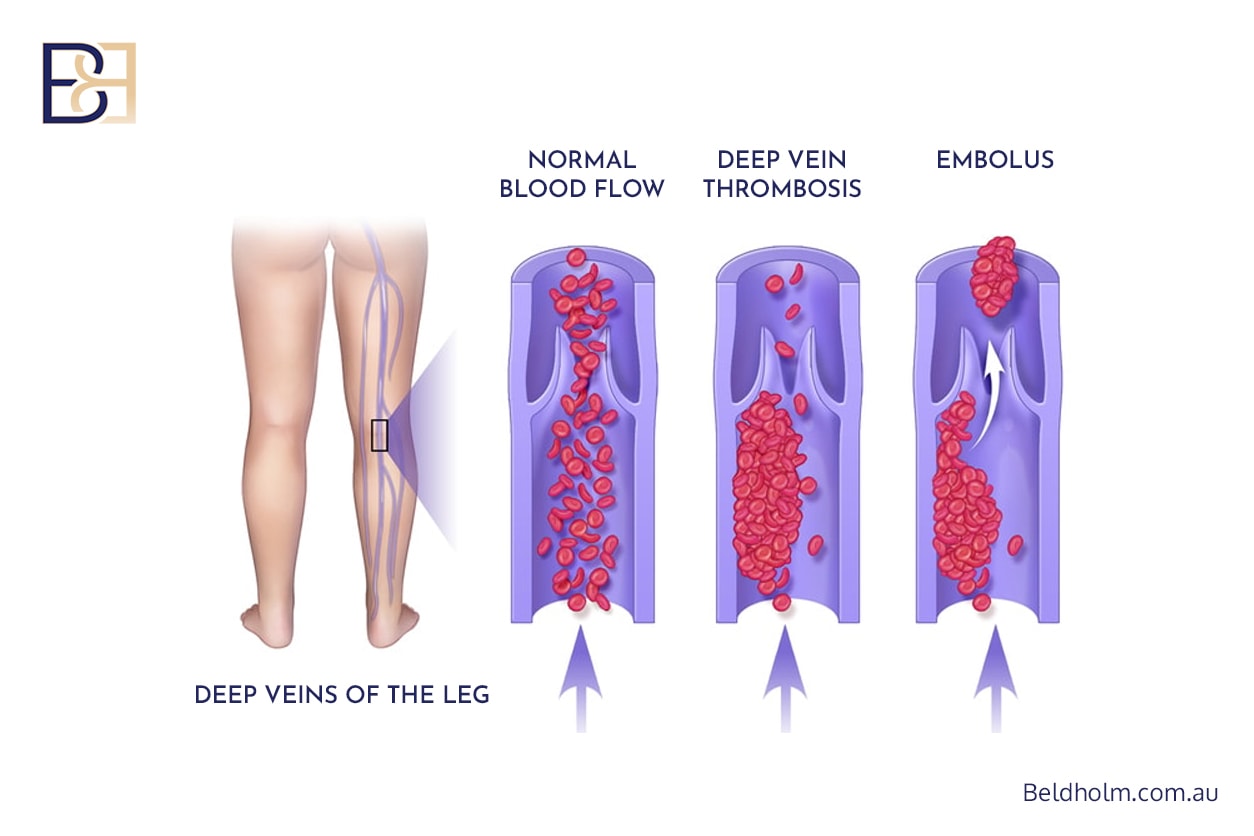
Although uncommon, blood clots are one of the more serious complications. Older studies reported rates of 2–9%, whereas modern preventive protocols reduce this to <1% [1,3].
What DVT and PE Are
- DVT (Deep Vein Thrombosis): A clot forming in the deep veins of the leg.
- PE (Pulmonary Embolism): A clot travelling to the lungs, which can be life‑threatening.
Symptoms
DVT (Deep Vein Thrombosis):
- Unilateral leg swelling
- Pain or tightness
- Warmth and redness
PE (Pulmonary Embolism):
- Sudden shortness of breath
- Chest pain
- Rapid heart rate
- Feeling lightheaded
Why It Happens
Risk increases with:
- Reduced mobility after major surgery
- Higher BMI
- Smoking
- Oestrogen‑based medications
- Personal or family history of clots
Prevention
Surgeons use several strategies:
- Early mobilisation (day 1)
- Compression stockings
- Intermittent pneumatic compression devices
- Blood thinners for moderate‑to‑high‑risk patients
Management
If a clot occurs:
- Hospital monitoring
- Anticoagulant medication
- Imaging tests (ultrasound or CT)
How Long Does It Take to Recover
- DVT: 3 months of anticoagulation on average
- PE: 3–6 months depending on severity
Systemic and General Complications
Not all complications are wound-related.
Anaemia
Blood loss during surgery can cause low haemoglobin [2].
Management:
- Iron supplementation
- Transfusion if severe
Allergic Reactions
Rare reactions to dressings or medications may occur.
Management:
- Change in dressings
- Steroid creams or antihistamines
Delayed Return of Function
Tightness across the abdominal muscles and lower body can make early movement uncomfortable.
Patients should follow:
- Early walking
- Slightly bent posture
- Reduced activity for up to six weeks
Late Complications
Some issues arise after the early recovery period.
Scar Problems
Most belt lipectomy scars heal well [1,4], but some may become wide or raised.
Management:
- Silicone therapy
- Massage
- Laser treatments
- Scar revision if needed
Skin Laxity Recurrence
If patients lose further weight [5], they may develop more loose skin. It is important to achieve and maintain a healthy weight before undergoing belt lipectomy, as further weight loss after surgery can increase the risk of recurrence of skin laxity.
Maintaining a stable weight reduces this risk.
Asymmetry or Contour Irregularities
Healing is not perfectly symmetrical. Some contour adjustments may be considered.
Risk Factors That Increase the Chance of Complications

Patient-Related
- High BMI
- Weight fluctuations
- Nutrient deficiencies
- Smoking
- Diabetes
- Older age
- Low haemoglobin
- Post-bariatric patients (at higher risk for complications due to nutritional and wound healing challenges)

Surgery-Related
- Large tissue resections
- Long operative times
- Liposuction performed simultaneously
- Large undermined areas
How Surgeons Reduce the Risk of Complications
Pre-Operative Optimisation

- Correct nutritional deficiencies and maintain a healthy diet before and after surgery to support recovery and overall health.
- Ensure weight stability
- Stop smoking
- Manage comorbidities
Surgical Technique Adjustments
- Limited undermining
- Avoiding aggressive liposuction
- SFS suspension to reduce tension
- Techniques from lower body lift (Belt lipectomy) surgery may be applied to optimise postoperative recovery and outcomes
Post-Operative Care
- Early mobilisation: Start gentle movement as soon as advised to reduce the risk of blood clots and promote healing.
- Wound monitoring: Regularly check your incisions for signs of infection, such as redness, swelling, or unusual discharge.
- Compression garments: Wear your compression garments as directed to help reduce swelling and support your new body contours.
- Drain care: Follow your surgeon’s instructions for caring for surgical drains to prevent infection and ensure proper healing.
- Carefully follow all your surgeon’s instructions regarding medication, activity restrictions, and wound care to minimise the risk of complications and support optimal recovery.
- Check your private health insurance cover to understand what post-operative care and potential claims are included, and ensure you meet any eligibility requirements.
Conclusion

A belt lipectomy is a powerful operation that helps many patients after major weight loss. While complications are common, most are manageable. Understanding the risks, maintaining realistic expectations, and following surgeon instructions can help patients navigate the recovery.
References
- Carloni R, Naudet F, Chaput B, et al. Are There Factors Predictive of Postoperative Complications in Circumferential Contouring of the Lower Trunk? Aesthetic Surgery Journal. 2016;36(10):1143-1154.
- Van Huizum MA, Roche NA, Hofer SOP. Circular belt lipectomy: A retrospective follow-up study on perioperative complications and cosmetic outcome. Ann Plast Surg. 2005;54:459–464.
- Carloni R, De Runz A, Chaput B, et al. Circumferential Contouring of the Lower Trunk: Indications, Techniques, and Outcomes—A Systematic Review. Aesth Plast Surg. 2016;40:652–668.
- Richter DF, Stoff A. Circumferential Body Contouring: The Lower Body Lift. Clin Plast Surg. 2014;41:775–788.
- El‑Sabbagh AH, El‑Hadidy MR, El‑Fahar MH. Postbariatric Abdominal Contouring: Technical Approach and Quality of Life. Plast Reconstr Surg. 2022;150(4):796–803.