Gynaecomastia Surgery in Newcastle, Maitland & Hunter Valley Australia
Book Online NowGynaecomastia is a common condition where male breast tissue enlarges due to hormonal imbalances. Over the past 15+ years, Dr. Bernard Beldholm has been focused on gynaecomastia surgery, helping men in the Newcastle, Maitland, and Hunter Valley regions with this issue and their chest appearance. Dr. Beldholm takes a distinctive approach to diagnosing and treating gynaecomastia, ensuring each patient receives the best possible care.
Dr. Beldholm performs gynaecomastia surgeries at Maitland Private Hospital, providing expert care in a modern medical environment.
Key Takeaways
- Gynaecomastia is the enlargement of male breast tissue caused by hormonal imbalances, which can affect men of all ages.
- Common symptoms include soft lumps in the breasts, which may be sensitive or painful to touch.
- Treatment options range from medications to surgical procedures, with a focus on personalised care and post-operative recovery to ensure optimal results.
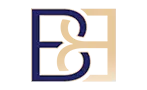
What is Gynaecomastia (male breast enlargement)?
Gynaecomastia is the enlargement of male breast tissue, a condition that can affect men at any age. It results from an imbalance between oestrogen and testosterone levels. When oestrogen levels are higher relative to testosterone, it can lead to the growth of breast tissue in men. This condition can affect one or both breasts and is often asymmetrical.
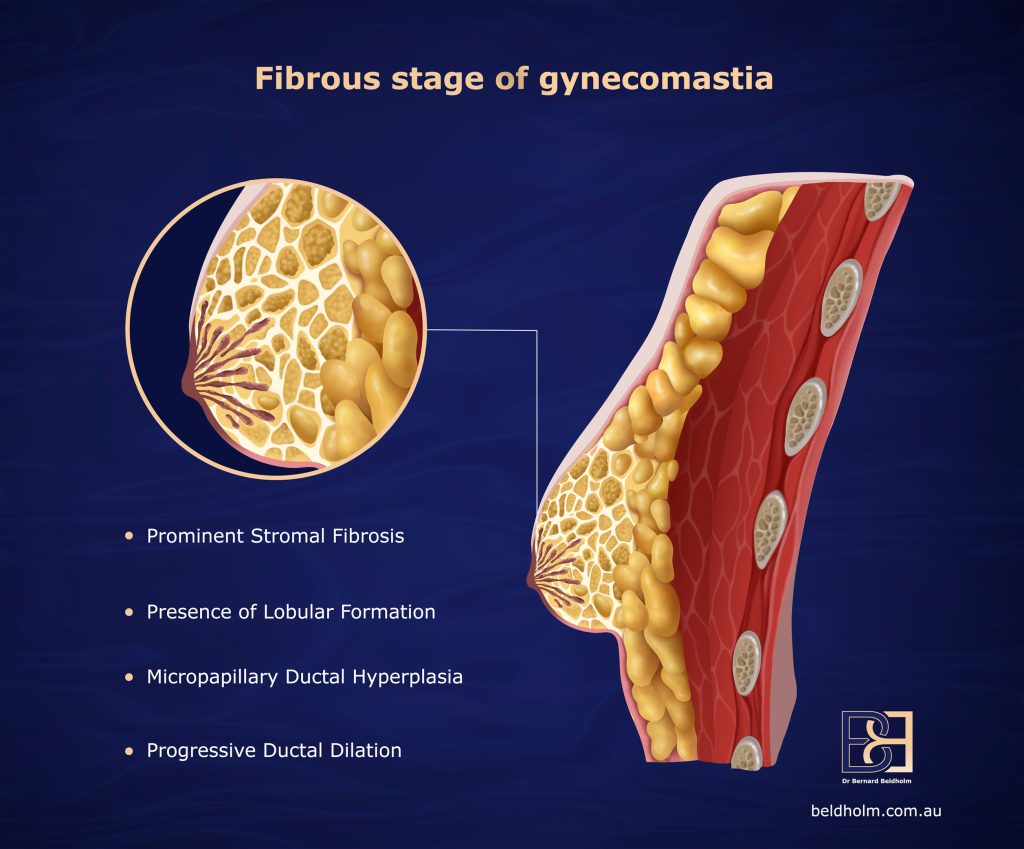
Book Online NowThe key difference between real gynaecomastia and pseudo-gynaecomastia lies in their causes. Real gynaecomastia is due to hormonal imbalances, whereas pseudo-gynaecomastia is caused by fat accumulation. In older men, increased oestrogen and decreased testosterone contribute to breast tissue growth. During puberty, the rise in testosterone usually prevents further breast development in males, but higher oestrogen levels can cause breast tissue enlargement.
Gynaecomastia is quite common during adolescence, with up to 60% of teenage boys experiencing some degree of breast enlargement by age 14. For men aged 50 to 80, the prevalence ranges from 24% to 65%, with about 66% of males over 50 being affected. Real gynaecomastia is characterised by firm or rubbery breast tissue, often symmetrical, while pseudo-gynaecomastia involves soft, fatty tissue.
Recognising gynaecomastia is essential. Whether mild or severe, understanding the condition assists in finding appropriate treatment and support.
Symptoms of Gynaecomastia
Men with gynaecomastia often experience soft, movable lumps in their breasts, which can be sensitive when touched. Enlarged breasts may occur in one or both breasts, leading to noticeable changes in the chest area. These physical changes can have a profound emotional impact.
Common symptoms include excess fat, a palpable, tender, firm, mobile, disc-like mound of tissue under the nipple, and sometimes breast pain. This combination of physical discomfort and emotional distress often leads to significant challenges in daily life.
Recognising these symptoms is vital for those with gynaecomastia, as it aids in seeking medical advice and support.
Causes of Gynaecomastia
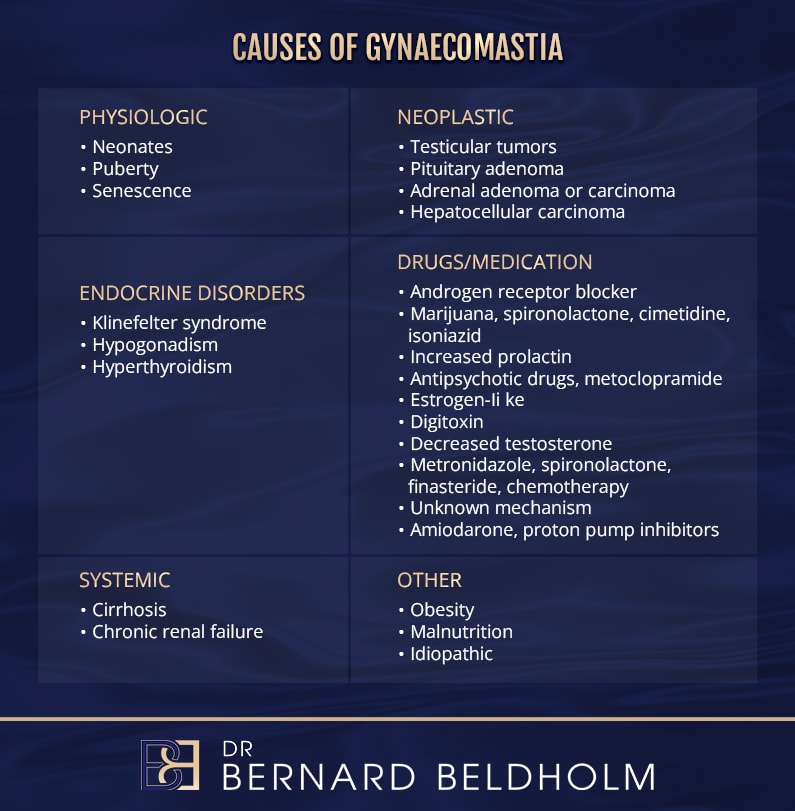
Gynaecomastia is primarily caused by hormonal imbalances, specifically an increase in oestrogen or a decrease in testosterone. Conditions such as hypogonadism and increased aromatase activity can contribute to these imbalances, leading to the development of gynaecomastia. Certain medications, including anti-androgens and anabolic steroids, can also trigger the condition by altering hormonal levels.
Medical conditions like Klinefelter syndrome, liver disease, and spinal cord disorders can significantly contribute to the development of gynaecomastia. Substance abuse, particularly the use of anabolic steroids, is another factor that can lead to hormonal changes promoting gynaecomastia. Despite these known causes, around 25% of cases remain idiopathic, meaning no specific cause can be identified.
Identifying the root causes of gynaecomastia is key to effective treatment. Correcting hormonal imbalances or underlying medical conditions, including those related to the pituitary gland, can mitigate or prevent the condition.
Diagnosis of Gynaecomastia
The diagnosis of gynaecomastia involves a detailed assessment, which typically starts with your GP. A comprehensive history and physical examination are essential for making an accurate diagnosis. In cases where there is no underlying medical condition, a referral to a surgeon may be necessary.
Initial Assessment by Your GP

Your GP will begin the process by taking a thorough medical history. The history of gynaecomastia is very important and may provide sufficient information to make a diagnosis. Many men who have had gynaecomastia since their teenage years, particularly those whose condition has not resolved, often fall into this category. Gynaecomastia caused by the use of anabolic steroids is also quite common and should be considered during the history-taking.
Importance of Medical History
The medical history is crucial in identifying the cause of gynaecomastia. If the condition began in adolescence and has not changed over time, this can be indicative of a persistent, benign form of the condition. For men who have used anabolic steroids, it is essential to disclose this information as it can be a contributing factor to the development of gynaecomastia. In many cases, the history alone may provide enough evidence to confirm the diagnosis without the need for additional testing.
Physical Examination
Gynaecomastia is usually not painful, and its presence is often noticeable upon examination. Your GP will perform a physical examination to assess the size and consistency of the breast tissue. A common sign of gynaecomastia is the enlargement of glandular tissue under the nipple, which is typically soft and movable.
In some cases, a discreet lump on one side of the breast may lead to suspicion of breast cancer. Although this is a rare occurrence in men, it is important for the GP to rule out other possibilities, particularly if the lump is hard or irregular in shape.
Diagnostic Imaging: Ultrasound
If the physical examination suggests gynaecomastia, an ultrasound is a common imaging test used to confirm the diagnosis. The ultrasound helps differentiate between glandular tissue and fat tissue, allowing for an accurate assessment of the condition. It may also help identify any underlying abnormalities, such as a cyst or tumor, if present.
Blood Endocrine Screen
To ensure there are no hormonal diseases contributing to gynaecomastia, a blood endocrine screen may be conducted. This test will measure hormone levels, including oestrogen and testosterone, to determine if there is a hormonal imbalance. Conditions such as hypogonadism or other endocrine disorders can sometimes be the underlying cause of gynaecomastia, so excluding these conditions is important for a complete diagnosis.
Referrals and Further Management
If no underlying condition is identified and the diagnosis of gynaecomastia is confirmed, your GP will likely refer you to a surgeon. It is typically at this stage that surgical options are discussed if conservative treatments are not suitable.

When Surgery Becomes an Option
For men who are past their teenage years, gynaecomastia is unlikely to resolve without surgical intervention. If the condition persists and causes physical discomfort or cosmetic concerns, surgery may be recommended. Surgical procedures, such as suction-assisted lipectomy (liposuction) or subcutaneous mastectomy, can effectively treat gynaecomastia, resulting in a flatter chest appearance.
Your GP can provide a referral to a specialist, such as Dr. Bernard Beldholm, who will evaluate the condition further and recommend the best treatment option based on your individual needs and goals.
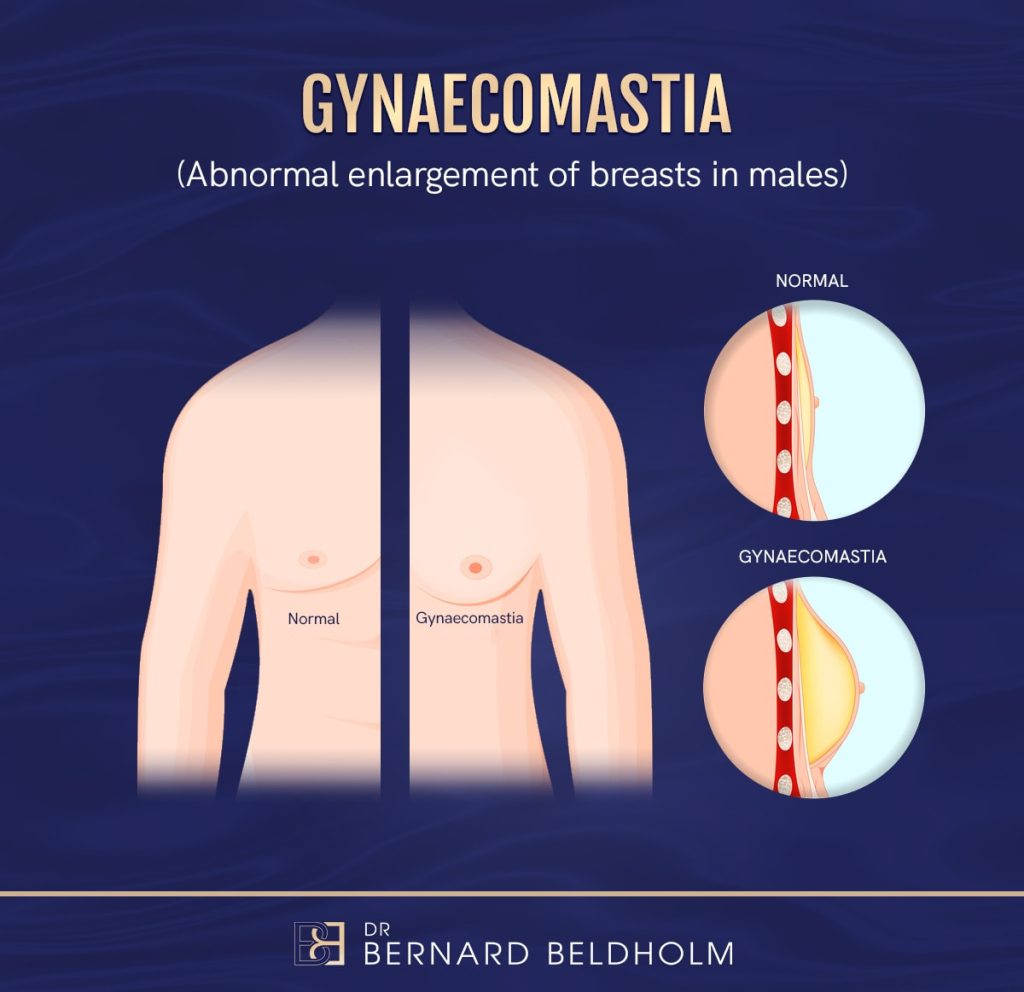
Dr Bernard Beldholm Gynaecomastia Grading System
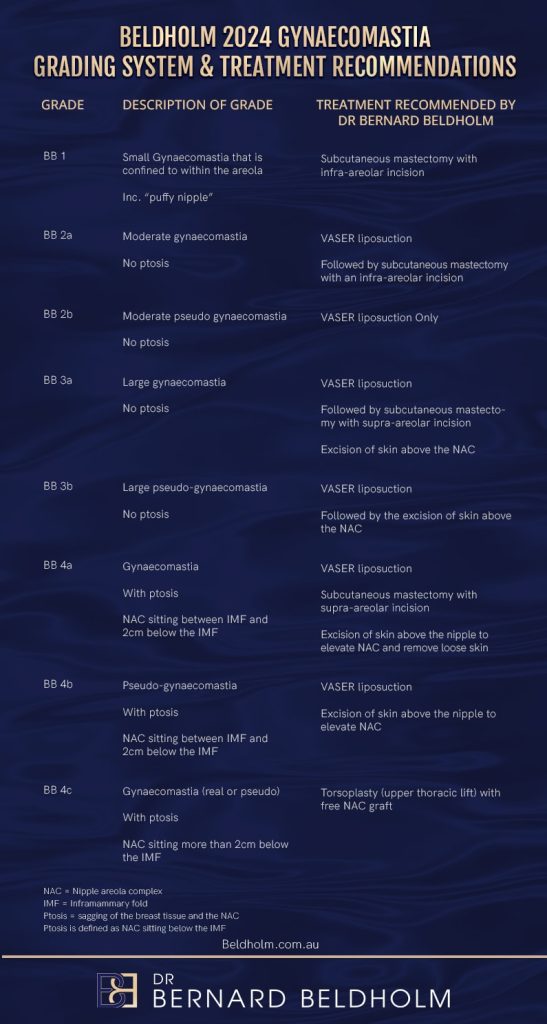
Dr. Bernard Beldholm’s 2024 Gynaecomastia Grading System is a valuable tool for assessing the severity of gynaecomastia and guiding treatment decisions. This system includes both real gynaecomastia and pseudo-gynaecomastia, providing a comprehensive framework for diagnosis and treatment.
The grading system helps differentiate between various degrees of breast tissue growth and excess skin. For moderate gynaecomastia without ptosis, suction-assisted lipectomy (liposuction) along with subcutaneous mastectomy is recommended. This approach ensures effective removal of excess breast tissue while focusing on aesthetic concerns.
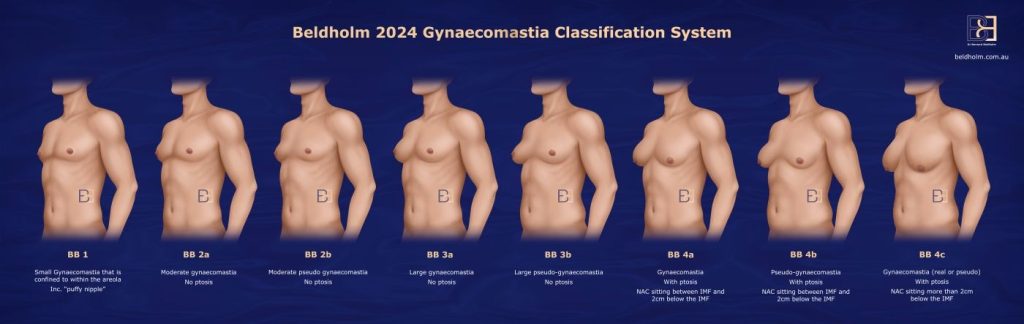
This grading system is beneficial for both patients and healthcare providers. It provides a standardised method for assessing gynaecomastia, ensuring that treatment plans are individualised.
Dr. Beldholm’s grading system assists in diagnosis and outcome prediction, making it a vital tool in managing gynaecomastia. For more detailed information, visit the Beldholm 2024 Gynaecomastia Grading System and Treatment Recommendations page.
Treatment Options for Gynaecomastia
Treatment for gynaecomastia depends on the severity of the condition, the underlying cause (if identified), and the impact it has on the patient. Treatment options range from medical therapies to surgical procedures. In many cases, surgical intervention becomes the most effective approach if medical treatment does not resolve the condition.
Medical Treatments
While medical treatments can be an option in some cases, Dr. Beldholm generally does not recommend medical treatment for gynaecomastia, as it has minimal long-term effect and there is a lack of substantial long-term data supporting its effectiveness. These treatments may help in certain cases, particularly when there are hormonal imbalances, but they are often less reliable than surgical options.
Androgens, Anti-Estrogens, and Aromatase Inhibitors
Medications like tamoxifen and raloxifene, which are anti-estrogens, may help reduce breast tissue by blocking estrogen’s effects. Aromatase inhibitors are another option, working by inhibiting the conversion of testosterone into estrogen.
- Tamoxifen and Raloxifene: These medications can be used to reduce the size of the breast tissue in some patients by lowering estrogen levels in the body. However, they can have side effects such as hot flashes, joint pain, reduced libido, and a possible impact on bone strength.
- Aromatase Inhibitors: These medications may also be prescribed to reduce estrogen levels, particularly in cases where the imbalance between estrogen and testosterone is significant.
Although pharmacological treatments can provide relief in some cases, they may not be suitable for long-term management or for more severe cases of gynaecomastia.
Surgical Treatments
If medical treatment does not sufficiently treat the condition, or if gynaecomastia is severe, persistent, or associated with functional impairment, surgical treatments may be recommended. If the patient is concerned about their gynaecomastia, Dr. Beldholm will generally recommend surgery, as it is the most effective treatment option with long-term results. Surgical options aim to remove excess breast tissue and result in a more typical male chest.
Overview of Surgical Treatment Options
- Subcutaneous Mastectomy for “Puffy Gland”
- For patients with “puffy nipples” or mild to moderate gynaecomastia, a subcutaneous mastectomy can be performed to remove the glandular tissue beneath the nipple. This procedure is used for patients with localised glandular enlargement without significant fat or excess skin. It aims to create a flatter chest contour.
- Subcutaneous Mastectomy with VASER Suction-Assisted Lipectomy (Liposuction) for Larger Gynaecomastia
- For larger gynaecomastia involving both glandular tissue and excess fat, a combination of subcutaneous mastectomy and VASER liposuction may be used. VASER Suction-Assisted Lipectomy (Liposuction) uses ultrasonic energy to break down fat before it is suctioned out, allowing for targeted removal of excess fat while minimising trauma to surrounding tissues.
- Subcutaneous Mastectomy with VASER Suction-Assisted Lipectomy (Liposuction) and Skin Excision for Gynaecomastia with Skin Laxity
- In cases where there is loose or excess skin in addition to enlarged breast tissue, subcutaneous mastectomy combined with VASER Suction-Assisted Lipectomy (Liposuction) and skin excision may be recommended. This approach addresses glandular tissue, excess fat, and redundant skin to achieve a firmer and flatter chest contour.
- Upper Body Lift (Upper Torsoplasty) for Significant Skin Laxity
- In cases of severe skin laxity or excessive skin, particularly after significant weight loss, an upper body lift (Upper Torsoplasty) may be considered. This more extensive procedure addresses the chest and surrounding areas, such as the back and sides, by removing excess skin and fat and tightening the remaining tissue. An upper body lift (Upper Torsoplasty) is generally performed when skin laxity cannot be corrected with subcutaneous mastectomy and VASER Suction-Assisted Lipectomy (Liposuction) alone.
Recovery After Gynaecomastia Surgery
Most gynaecomastia surgeries are performed as day procedures, meaning patients can go home the same day after surgery. However, for more extensive procedures like the upper body lift, an overnight stay in the hospital is typically required for monitoring and recovery.
Post-Operative Care
During the initial recovery period, drains are commonly used, except for the smallest type of operations. These drains help remove excess fluid from the surgical site, which may reduce the risk of certain complications. You will also have a compression dressing applied to place gentle pressure on the chest area, along with a compression garment to help manage swelling and support the healing process.
The compression dressing is usually removed the day after surgery. Drains are typically removed the following day, depending on the amount of fluid collected.
Follow-Up Appointments
The first week following surgery often involves the most frequent follow-up care. During this time, you will see Dr. Beldholm and his nurse for regular check-ups, Healite™ LED treatment, and dressing changes. These appointments are important for monitoring the healing process and addressing any concerns that may arise early in recovery.
Since the sutures used in gynaecomastia surgery are absorbable, there is no need for them to be removed.
Returning to Work and Activities
- Desk-type work: Most patients are able to return to work within a few days, provided it involves minimal physical activity and is desk-based.
- More intense work: For jobs requiring more intense activity, it is usually advised to wait 1-2 weeks before returning.
- Heavy lifting: For work that involves heavy lifting or strenuous physical exertion, you should plan to take 2-4 weeks off to allow proper healing and avoid complications.
Travel and Extended Stay
If you are travelling for surgery, it is ideal to stay in the area for 3-4 days after surgery to ensure proper follow-up and monitoring. For more extensive procedures like the upper body lift (Upper Torsoplasty), a stay of 1-2 weeks is recommended to ensure you have adequate time for proper recovery and follow-up care.
By following Dr. Beldholm’s post-operative instructions and attending the necessary follow-up appointments, you will be well on your way to achieving optimal results.
Complications from Gynaecomastia Surgery
As with any surgical procedure, gynaecomastia surgery carries potential risks and complications. These can vary between individuals and may depend on the type of surgery performed and personal health factors. While steps are taken during surgery and recovery to reduce these risks, it is important to be aware of them before deciding whether to proceed.
Possible complications may include:
- Bleeding
- Infection
- Fluid accumulation (seroma or haematoma)
- Delayed wound healing
- Scarring
- Changes in nipple or breast sensation, which may be temporary or permanent
- Asymmetry or contour irregularities
- Skin laxity that does not fully tighten after surgery
- Issues related to anaesthesia
- Need for further surgery

Dr. Beldholm’s Final Thoughts on Gynaecomastia Surgery
Gynaecomastia surgery is one option available for men with enlarged breast tissue. The condition can be associated with various factors, including hormonal changes, weight fluctuations, and certain medical conditions or medications. While the surgery can address the removal of excess glandular tissue and/or fat, outcomes vary between individuals.
As a surgeon, my role is to perform each procedure with the goal of achieving a chest contour that is in proportion with the patient’s body. Gynaecomastia surgery involves more than just removing excess tissue — it is about addressing the specific anatomical concerns that each patient presents with.
Surgical intervention may be considered for patients who have not achieved their desired change through non-surgical measures. Procedures such as suction-assisted lipectomy (VASER liposuction) and subcutaneous mastectomy can be adapted to the individual’s anatomy and clinical needs.
For mild to moderate gynaecomastia, subcutaneous mastectomy with or without suction-assisted lipectomy (VASER liposuction) may be sufficient to address glandular tissue and excess fat. In cases involving significant skin laxity, a more extensive approach — such as skin excision or an upper body lift (Upper Torsoplasty) may be required to address both tissue and skin changes.
A personalised treatment plan is developed for each patient based on their individual condition. Post-operative care, including adherence to recovery instructions and attending scheduled follow-up appointments, plays an important role in monitoring healing and supporting the best possible outcome for that individual.
Frequently Asked Questions
What causes gynaecomastia?
Gynaecomastia is the enlargement of male breast tissue, and it is primarily caused by an imbalance between the hormones oestrogen and testosterone. The condition can affect one or both breasts and may vary in severity. Below are some common causes of gynaecomastia:
How is gynaecomastia diagnosed?
Diagnosing gynaecomastia involves a thorough evaluation by a healthcare professional, typically a specialist or your GP, who will assess the condition through a combination of medical history, physical examination, and diagnostic tests. The goal is to confirm that the breast enlargement is due to glandular tissue growth (gynaecomastia) rather than other conditions, such as fat accumulation (pseudo-gynaecomastia) or, in rare cases, breast cancer.
What are the treatment options for gynaecomastia?
The treatment for gynaecomastia depends on the severity of the condition, the underlying cause (if identified), and the patient’s goals. Treatment options can range from medical therapies to surgical interventions, with surgery often being the most effective and long-term solution, especially for persistent or severe cases.