Fleur‑de‑Lis Abdominoplasty Post‑Weight Loss
Book Online NowA Fleur‑de‑Lis Abdominoplasty post weight loss (also called fleur de lis abdominoplasty) is a major surgical procedure that focuses on removing excess skin and tightening the abdominal wall after significant weight loss. This approach is designed for patients who have achieved massive weight loss through diet, exercise, or bariatric surgery and now experience loose skin that drapes in both vertical and horizontal directions across the abdominal area.
What Is a Fleur‑de‑Lis Abdominoplasty?
A fleur de lis abdominoplasty differs from a traditional abdominoplasty (tummy tuck procedure) in that it removes excess abdominal skin in two planes. The technique involves both a horizontal incision (across the lower abdomen) and an additional vertical incision through the midline. This dual approach allows the surgeon to remove significant excess skin in both directions—making it particularly useful after major weight loss when the skin is loose not just downward but also side‑to‑side.
In addition to removing excess skin, the procedure often includes tightening of abdominal muscles (diastasis recti) that have separated (a condition known as diastasis recti), treating core stability and abdominal shape. Some patients may also have hernias repaired simultaneously, or liposuction (suction-assisted lipectomy) to remove excess fat deposits that remain after weight loss.
Book Online NowWho Is a Candidate?
Candidacy for a fleur de lis abdominoplasty depends on several factors, but two main groups of considerations guide the decision: the pattern of loose skin and the patient’s overall medical readiness for surgery. It is particularly suitable for those who have undergone bariatric surgery or achieved weight reduction through other means, such as medication or lifestyle change. There is no set weight requirement; however, Medicare defines significant weight loss as a reduction of five BMI units. In Dr Beldholm’s experience, a loss of more than 30 kilograms is often required to create enough loose skin to consider a Fleur‑de‑Lis Abdominoplasty.
Where Is the Loose Skin?
When people are overweight, the abdominal skin stretches to accommodate fat tissue beneath it, like a balloon expanding. After major weight loss, the skin may not retract fully, leaving folds in the upper and lower abdomen. The direction of this looseness determines which surgical technique is most appropriate:
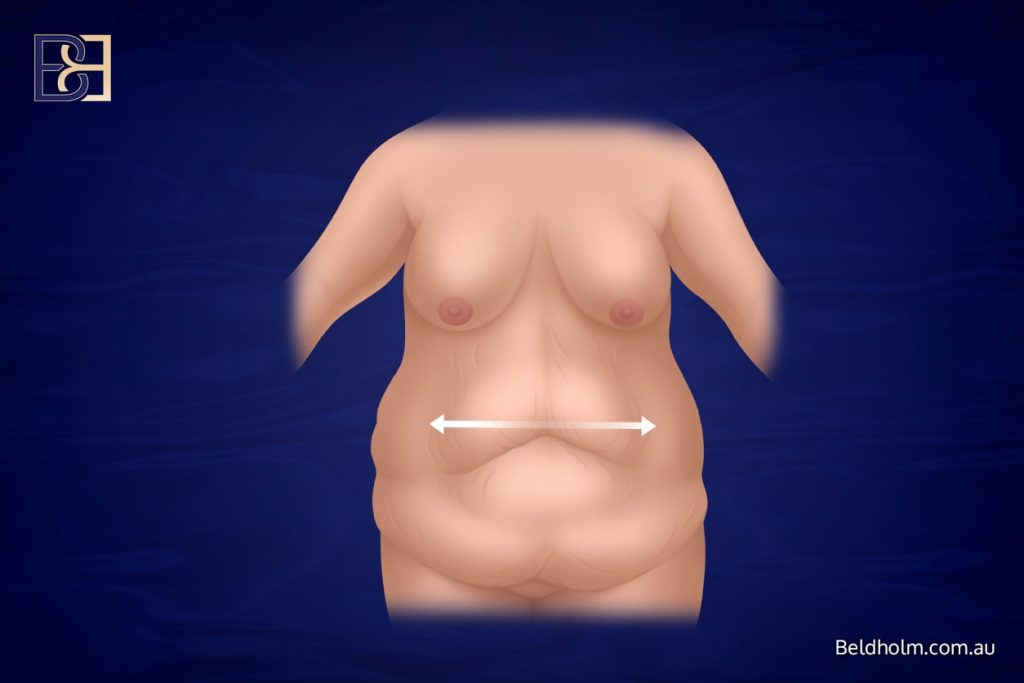
Horizontal looseness: When the skin is loose across the midline and sides, a fleur de lis abdominoplasty is indicated. This approach uses horizontal and vertical incisions to remove tissue from both directions, focusing on the horizontal laxity that a standard tummy tuck (abdominoplasty) cannot correct.
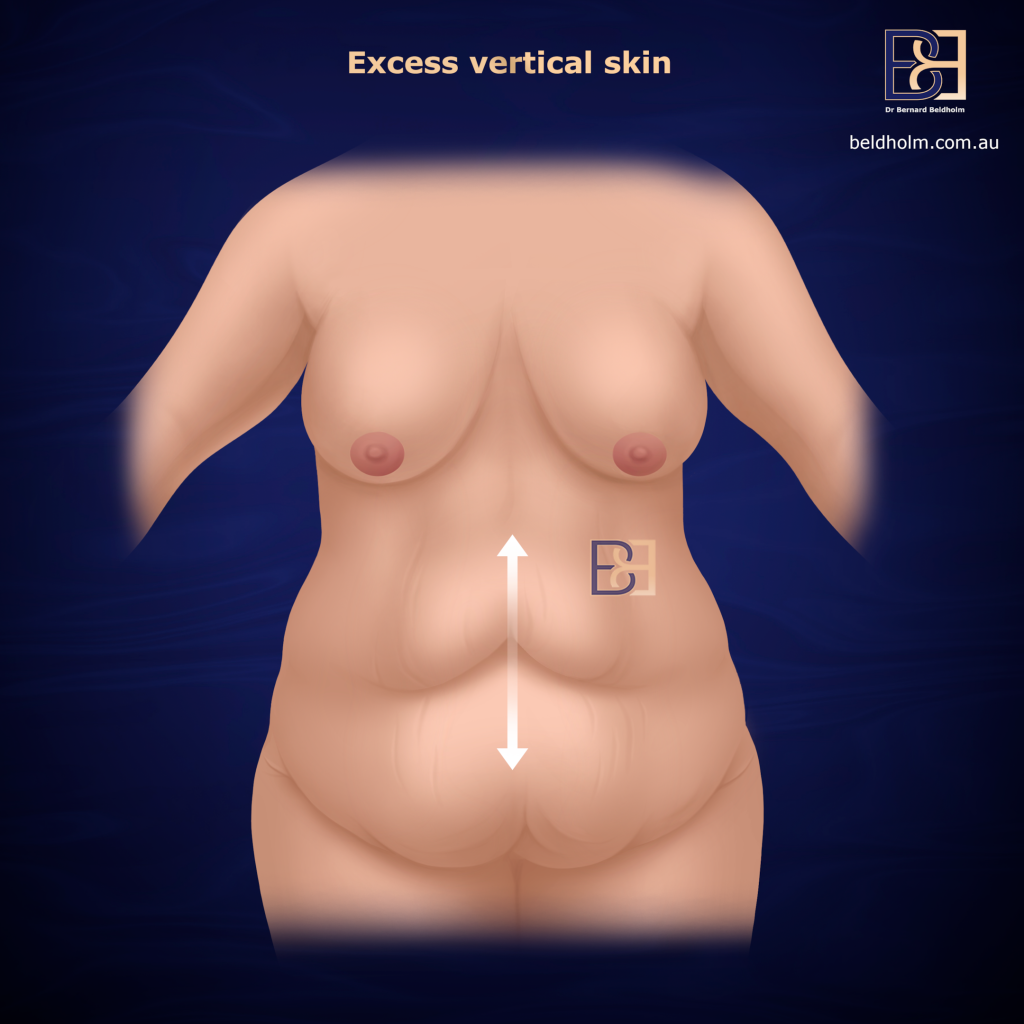
Vertical looseness: A traditional abdominoplasty or extended abdominoplasty is often sufficient if most of the looseness is vertical (the skin hangs downward).
Patients who have experienced significant weight loss and have excess skin that drapes from side to side benefit most from this operation.
Medical and Lifestyle Factors
Good surgical candidates must also be medically suitable. This includes:
General Health
Patients should be in good physical condition with no uncontrolled medical conditions such as diabetes, heart disease, or immune disorders.


Smoking Status
Smoking increases the risk of poor wound healing and delayed recovery. Non‑smokers are preferred candidates; smokers must stop well in advance of surgery.
Stable Weight
Achieving and maintaining a stable weight for at least six months—ideally 12 months—is crucial before surgery. Performing the operation while the weight is still fluctuating can compromise results.

Nutritional Health
Adequate protein and micronutrient intake help support wound healing and recovery.
Realistic Expectations
The operation removes excess skin, but it is not a weight‑loss procedure. Patients should understand the functional and aesthetic goals in realistic terms.
When Should I Consider the Operation?
The fleur de lis abdominoplasty is considered when excess skin causes discomfort, hygiene difficulties, or limitations in clothing. Common concerns include rashes beneath skin folds & difficulty exercising. The operation can also repair weakened abdominal muscles and hernias that may have developed after pregnancy or massive weight loss.
A tailored surgical plan is created for each patient based on their medical history, examination findings, and goals.
How Fleur-de-Lis Abdominoplasty Works
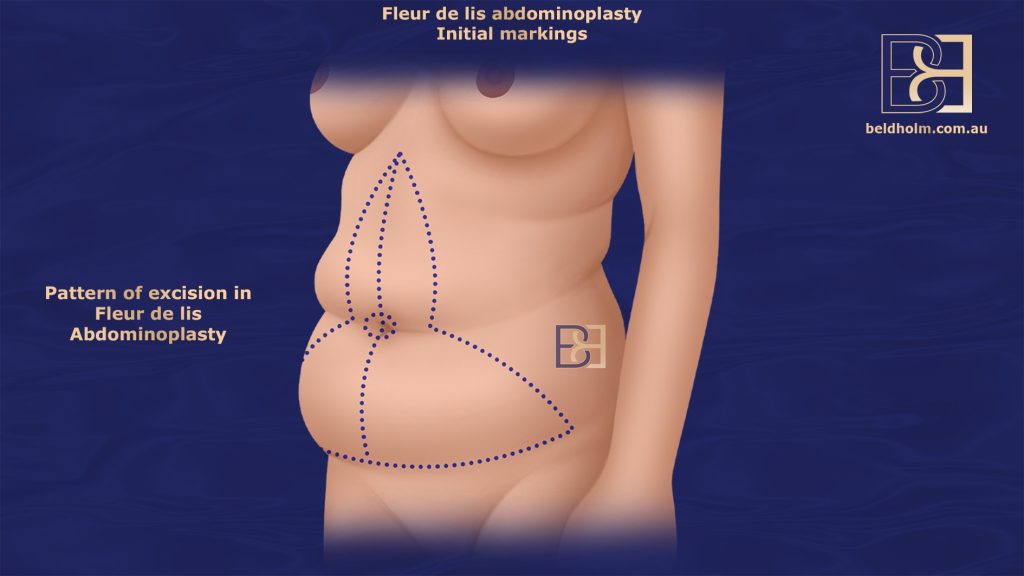
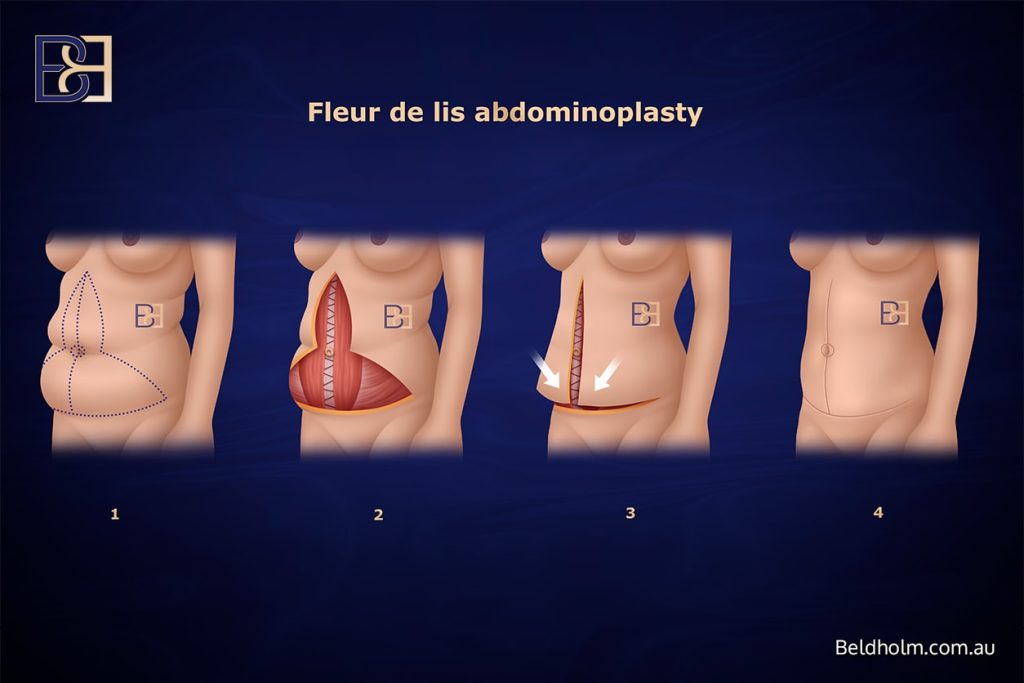
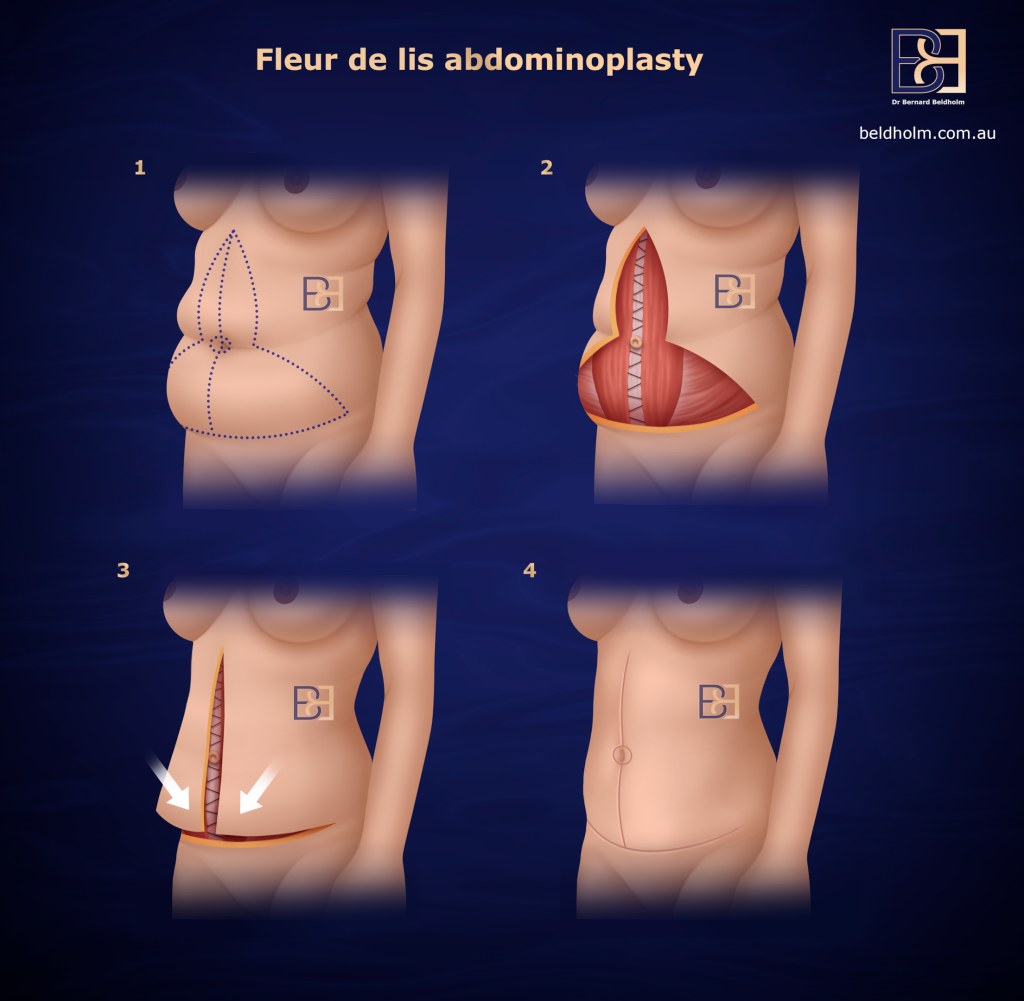
The operation begins with detailed pre‑operative planning. Surgical markings are made while the patient is standing to define where excess abdominal skin will be removed. Under general anaesthesia, Dr Beldholm performs the following steps:
- Excision of excess skin — The surgeon removes redundant tissue from both the vertical and horizontal directions.
- Vertical incision — Extends up the midline, allowing removal of skin across the upper abdomen as well.
- Horizontal incision — Made low across the lower abdomen, similar to a standard tummy tuck (abdominoplasty).
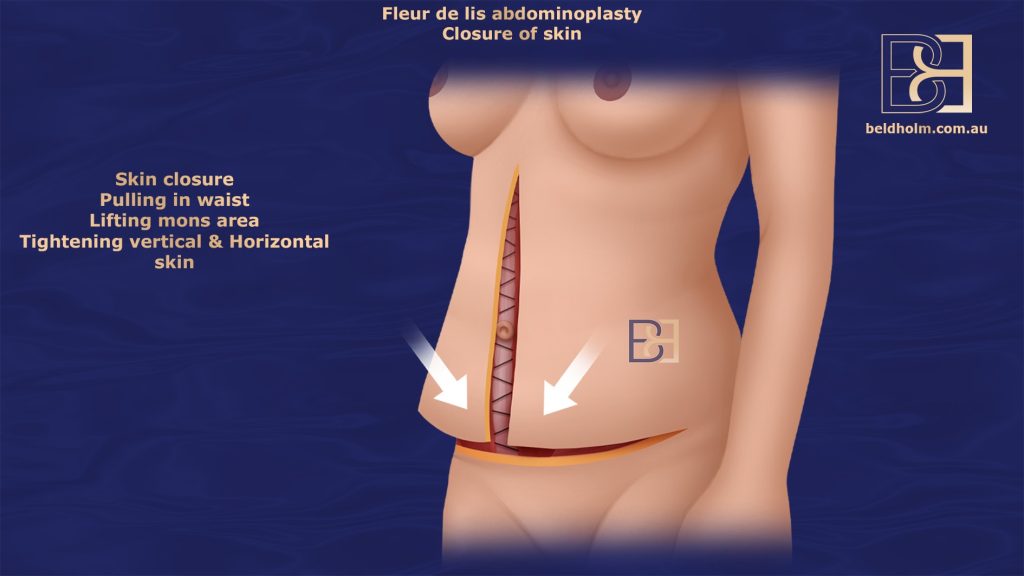
- Tightening the abdominal wall — The abdominal muscles are brought together and reinforced if they have separated (diastasis recti).
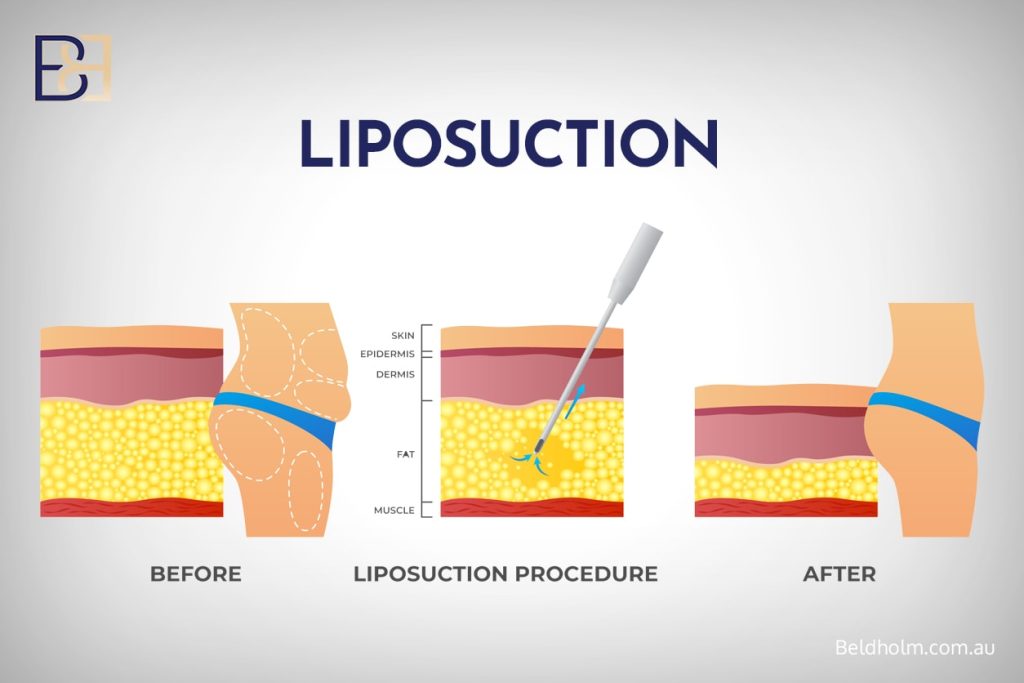
- Optional liposuction (suction-assisted lipectomy) — Used to remove fat in the surrounding areas, such as the flanks or lower chest
- Belly button repositioning — The belly button is relocated on the newly tightened skin.
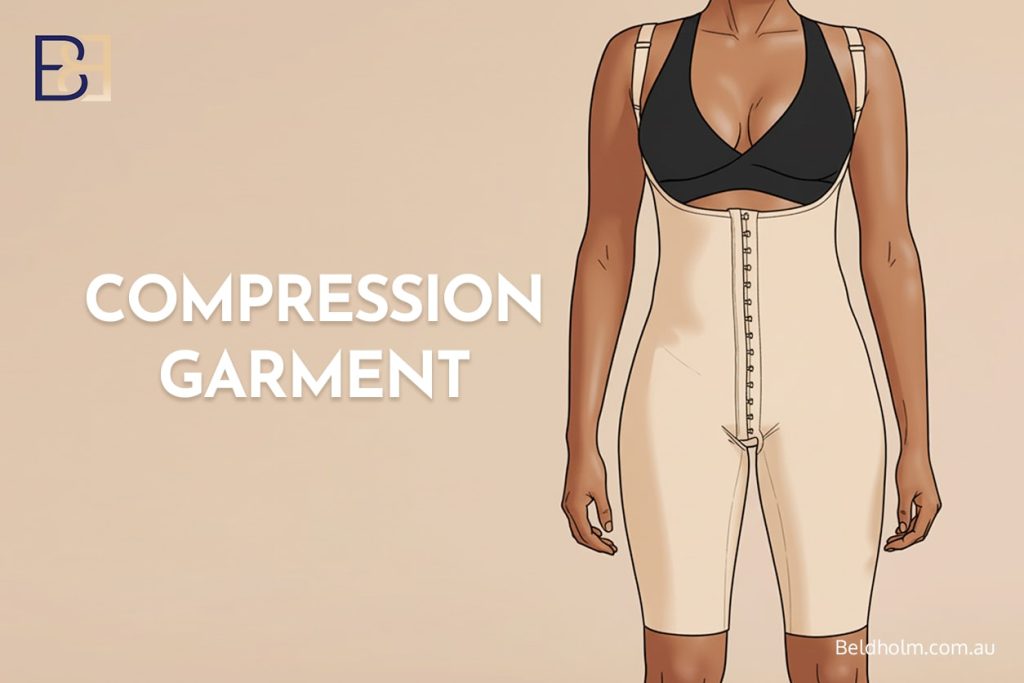
- Dressings and compression garments — Applied to support the healing process and reduce swelling.

This major surgical procedure may take three to five hours, depending on complexity. Patients stay in Maitland Private Hospital, which offers 24‑hour medical supervision and on‑site ICU facilities.
Combining Procedures for Optimal Results
A fleur de lis abdominoplasty may include complementary procedures. These are tailored to each patient’s anatomy and medical needs.
VASER Liposuction (suction-assisted lipectomy)
VASER-assisted liposuction (suction-assisted lipectomy) is Dr Beldholm’s preferred method for removing residual fat tissue that may remain after weight loss. It uses ultrasound energy to emulsify fat before removal. VASER liposuction (suction-assisted ultrasonic lipectomy) is especially useful for the flanks, lower chest, and pubic region.
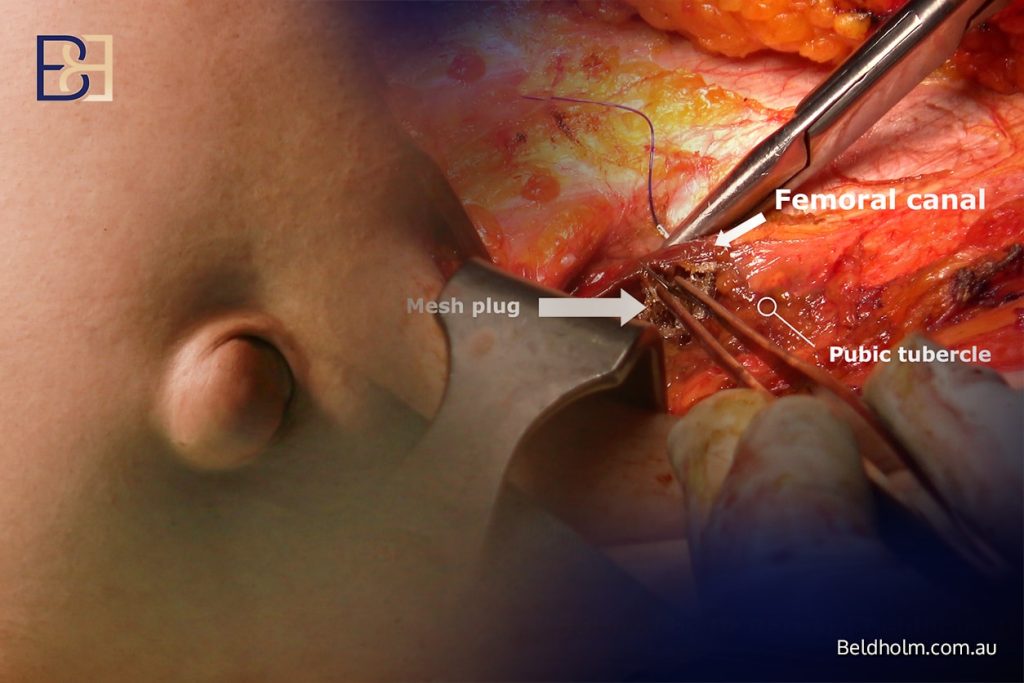
Hernia Repair
Some patients who have undergone massive weight loss or bariatric surgery may develop abdominal hernias due to weakened connective tissue or prior surgical incisions. Common types that can be repaired during a fleur de lis abdominoplasty include:
- Umbilical hernias: Occur around the belly button, where the abdominal wall has thinned or stretched.
- Epigastric hernias: Appear along the midline above the navel and are common after major weight changes.
- Incisional hernias: Develop at the site of previous abdominal surgery or laparoscopic ports.
- Ventral hernias: Form anywhere in the front abdominal wall from general tissue weakness.
Repairing these hernias during the same operation allows Dr Beldholm to reinforce the abdominal wall while simultaneously removing excess skin. This integrated approach targets strength, comfort, and function while avoiding the need for a separate procedure.
Diastasis Recti Repair
Separation of the abdominal muscles (rectus abdominis) is common after significant weight loss or pregnancy. Tightening these abdominal muscles (diastasis recti) during surgery provides better trunk stability. Repairing diastasis recti can also treat posture and functional core strength.
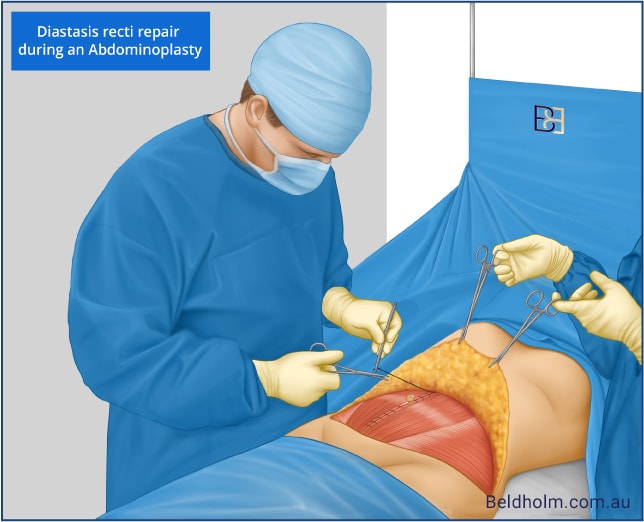
Loose Abdominal Wall Tightening
In some patients, the abdominal wall becomes stretched and weakened not only between the rectus muscles but also in the side and lower regions. Dr Beldholm can tighten the entire loose abdominal wall as part of the operation. This is done by carefully re‑approximating and reinforcing the fascial layers across the abdomen.
Dr Beldholm develops a tailored surgical plan that combines these options when appropriate, ensuring each element works together.
Recovery Process and Follow‑Up Care
Because this is a major surgical procedure, recovery requires time and structured care. Dr Beldholm’s post‑operative program in Maitland is designed to support patients through every phase of the healing process.
Early Recovery (First 2 Weeks)

Patients usually stay in hospital for 2–3 nights. During this time, nurses assist with mobility, drain management, and pain relief.
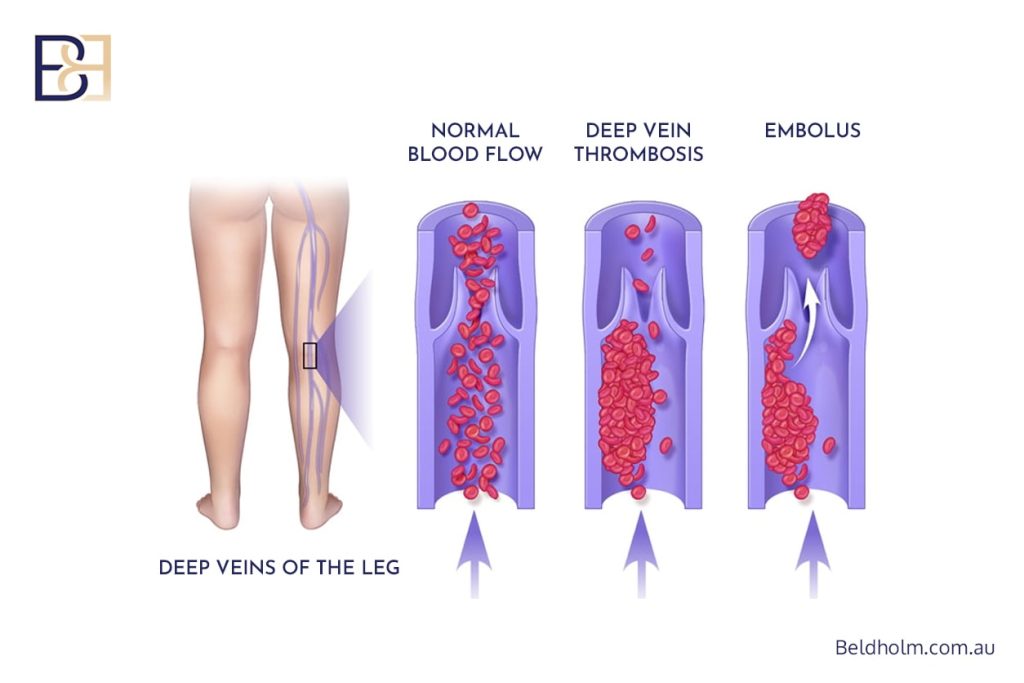
After discharge home, LED light therapy is used to promote wound healing, and dressings are changed regularly. At home, patients are encouraged to walk short distances to reduce the risk of deep vein thrombosis (DVT).
Compression garments are worn continuously to support healing and minimise swelling. PICO or Hypafix dressings are used for optimal wound protection. Prescribed medications help manage pain.
Ongoing Recovery (Weeks 3–6)

During this stage, light daily activities can be resumed. Patients must avoid heavy lifting or strenuous exercise while internal tissues continue to heal. Swelling gradually subsides.
Long‑Term Recovery (Months 3–12)
Most patients return to normal activities within six weeks, but full recovery—including scar maturation—can take up to 12 months. Routine follow up appointments at 1,3 6 and 12 months are included in the procedure fee. Telehealth reviews are available for regional patients.
Maintaining a healthy lifestyle, good hydration, and a stable weight helps ensure proper recovery.
Potential Risks
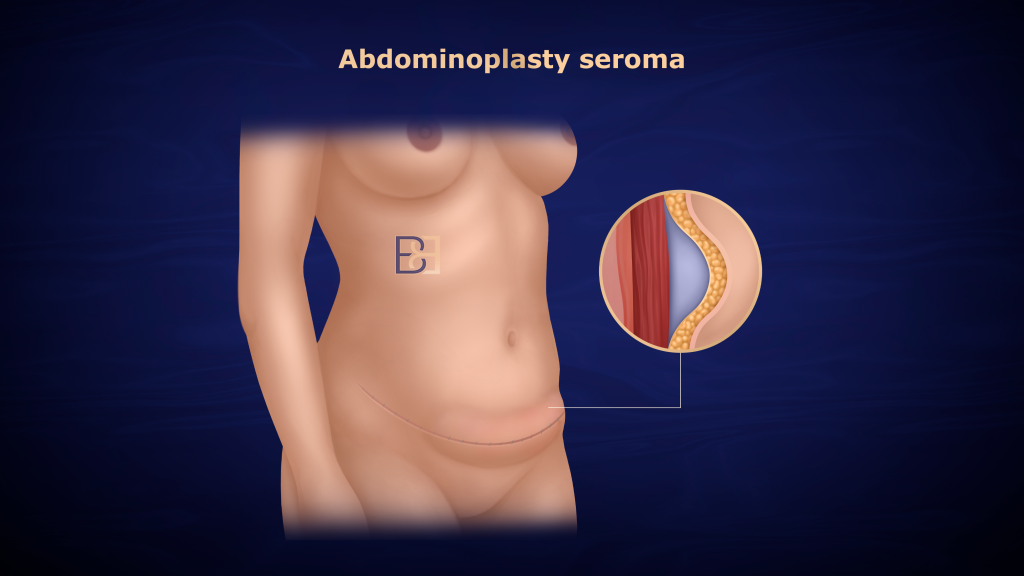
All abdominoplasty procedures carry potential risks, which are carefully discussed during consultation. Risks include:
- Poor wound healing or delayed wound healing
- Seroma (fluid accumulation)
- Infection or bleeding
- Deep vein thrombosis (DVT) or pulmonary embolism
- Changes in skin sensation near incision sites
- Prominent scarring from horizontal and vertical incisions
Dr Beldholm’s team takes multiple steps to reduce these risks, including the use of compression stockings, early mobilisation, and precise surgical techniques. Following all instructions and attending regular follow-up appointments supports a smooth recovery.
Frequently Asked Questions
What happens if I lose more weight after abdominoplasty?
Losing additional weight after surgery may lead to new loose skin. Dr Beldholm recommends reaching a stable weight before surgery to maintain long‑term results.
What is the BMI cut off for abdominoplasty?
There’s no strict cut-off. Lower BMI levels are generally better for surgery. In my experience, patients who are closer to normal weight or only slightly overweight (BMI 18 to 30) will generally achieve better results from body contouring surgery. If there is a significant amount of excess adipose tissue, this may limit the result I can achieve. Medicare eligibility requires that you’ve reduced your BMI by at least 5 units after weight loss surgery or lifestyle change.
Do you need skin removal surgery after weight loss?
Not everyone does. Some people have good skin elasticity and less remaining skin. Others, especially those who have undergone bariatric surgery, may consider operations such as abdominoplasty or lipectomy.
How long does a Fleur‑de‑Lis tummy tuck (abdominoplasty) take to heal?
Most patients resume normal activities after a few weeks, but full recovery—including scar softening—takes several months. The initial recovery period focuses on rest, wound care, and compression.
What are the pros and cons of the Fleur‑de‑Lis tummy tuck (abdominoplasty)?
Pros: Removes excess skin in two directions, repairs abdominal muscles
Cons: Longer scars and a more complex operation compared with a traditional tummy tuck (abdominoplasty).
Does Medicare cover the procedure?
Medicare may provide a rebate if strict post‑weight‑loss criteria are met (e.g., massive weight loss and functional symptoms like rashes). Eligibility is assessed individually during consultation.
Dr Beldholm’s Final Conclusions

As Dr Bernard Beldholm, Specialist General Surgeon, explains, a Fleur‑de‑Lis Abdominoplasty post weight loss is a carefully planned surgical procedure that treats significant excess skin and a weakened abdominal wall following major weight loss. Depending on the patient’s needs, the operation can also include additional techniques such as VASER‑assisted liposuction (suction-assisted lipectomy), hernia repair, and diastasis recti repair when appropriate.
Dr Beldholm performs this surgery at Maitland Private Hospital, where patients benefit from a structured care program that includes thorough pre‑operative assessment, attentive in‑hospital management, and ongoing follow‑up appointments. The procedure aims to treat functional concerns for patients who have experienced significant weight loss, but results vary between individuals. Dr Beldholm encourages patients to maintain a stable weight, follow all post‑operative care instructions, and attend scheduled reviews to support a predictable recovery.